IMPACT OF TIME SPENT WAITING FOR AUTOLOGOUS TRANSPLANTATION ON THE OUTCOME OF PATIENTS WITH MULTIPLE MYELOMA.
(Abstract release date: 05/19/16)
EHA Library. Ripamonti F. 06/09/16; 134853; PB1953

Dr. Francesco Ripamonti
Contributions
Contributions
Abstract
Abstract: PB1953
Type: Publication Only
Background
Autologous stem cell transplantation (Tx) is still the standard of care for symptomatic myeloma patients (pts) eligible for high-dose procedure. Whether time lasting between stem cell collection and Tx (Wait-Tx) has an impact on Tx outcome itself is matter of debate.
Aims
The aim of this study is to evaluate whether Wait-Tx impacts on the outcome of transplanted myeloma pts
Methods
We reviewed data of 233 myeloma pts treated with HD Melphalan between January 2000 and December 2013; 20 pts with primary refractory disease and 26 pts treated with a double transplant program were excluded. One hundred eighty seven (187) pts entered the analysis: Male/Female 99(53%)/88(47%), median age 55 years (28-69), Myeloma Type IgG/IgA/light chain/non secretory 111(59%)/38(20%)/33(18%)/5(3%), Durie&Salmon stage II/III 26(14%)/161(86%). Induction therapy consisted of 4 VAD cycles in 83 pts (44%) treated from 2000 to 2005 or 4 Bortezomib-based cycles in 104 pts (56%) treated from 2006 to 2013. Stem cell collection was primed with a single course of DCEP or HD-EDX followed by G-CSF at 10 mcg/kg until completing stem cell collection (PBSC). Tx conditioning regimen consisted of single HD-Melphalan infusion 200 mg/m2 in 137 pts (73%); HD Melphalan was given at the reduced dose of 160 mg/m2 in 50 pts (27%) due to comorbidity. Response was defined according to International Myeloma Working Group criteria.
Results
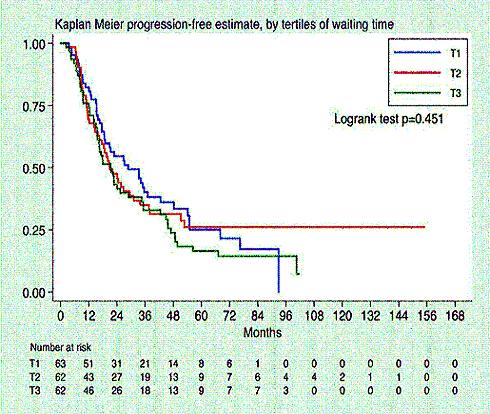
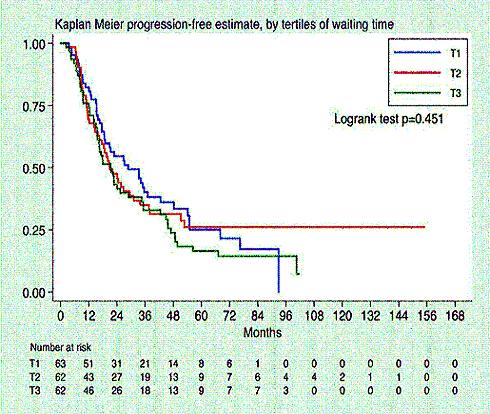
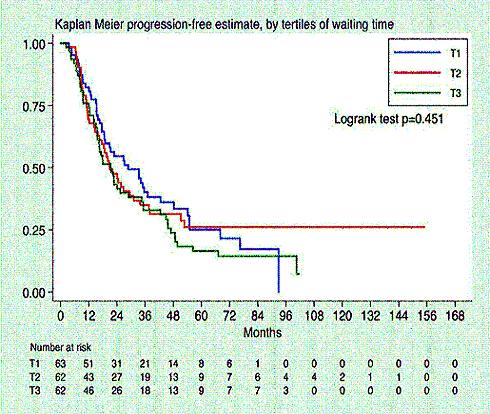
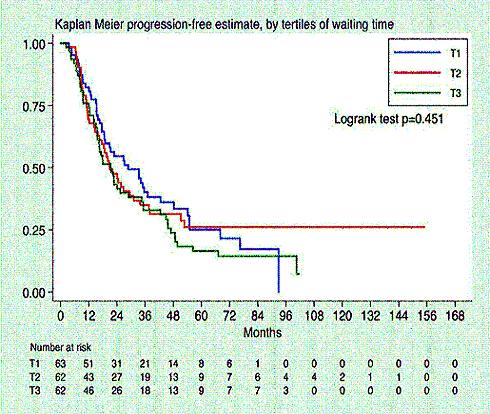
Median time between stem cell collection and transplantation (Wait-Tx) was 4 months (range 0.9-13.8 months). After a median follow up after Tx of 49 months (range 24-75 months), 140 patients (74%) relapsed or progressed, median progression free survival (PFS) after Tx was 23 months (range 12-54 months), with a median OS after Tx of 70 months (range 34 months -not reached). PFS was not different between tertiles of Wait-Tx (T1= 0.9-3.2 months, T2= 3.3- 4.6 months, T3=4.7-13.8 months; logrank test p=0.45, cfr Figure 1). When multivariate analysis was performed including Wait-Tx, age at Tx, disease status at Tx ( ≥VGPR vs PR vs
Conclusion
Time frame between PBSC collection and stem cell infusion had no significant impact on the outcome of transplanted myeloma patients. Response to induction treatment and bortezomib based induction therapy are both predictive of better outcome ensuring a longer PFS after transplantation.
Session topic: E-poster
Keyword(s): Autologous, Myeloma, Outcome, Transplant
Type: Publication Only
Background
Autologous stem cell transplantation (Tx) is still the standard of care for symptomatic myeloma patients (pts) eligible for high-dose procedure. Whether time lasting between stem cell collection and Tx (Wait-Tx) has an impact on Tx outcome itself is matter of debate.
Aims
The aim of this study is to evaluate whether Wait-Tx impacts on the outcome of transplanted myeloma pts
Methods
We reviewed data of 233 myeloma pts treated with HD Melphalan between January 2000 and December 2013; 20 pts with primary refractory disease and 26 pts treated with a double transplant program were excluded. One hundred eighty seven (187) pts entered the analysis: Male/Female 99(53%)/88(47%), median age 55 years (28-69), Myeloma Type IgG/IgA/light chain/non secretory 111(59%)/38(20%)/33(18%)/5(3%), Durie&Salmon stage II/III 26(14%)/161(86%). Induction therapy consisted of 4 VAD cycles in 83 pts (44%) treated from 2000 to 2005 or 4 Bortezomib-based cycles in 104 pts (56%) treated from 2006 to 2013. Stem cell collection was primed with a single course of DCEP or HD-EDX followed by G-CSF at 10 mcg/kg until completing stem cell collection (PBSC). Tx conditioning regimen consisted of single HD-Melphalan infusion 200 mg/m2 in 137 pts (73%); HD Melphalan was given at the reduced dose of 160 mg/m2 in 50 pts (27%) due to comorbidity. Response was defined according to International Myeloma Working Group criteria.
Results
Median time between stem cell collection and transplantation (Wait-Tx) was 4 months (range 0.9-13.8 months). After a median follow up after Tx of 49 months (range 24-75 months), 140 patients (74%) relapsed or progressed, median progression free survival (PFS) after Tx was 23 months (range 12-54 months), with a median OS after Tx of 70 months (range 34 months -not reached). PFS was not different between tertiles of Wait-Tx (T1= 0.9-3.2 months, T2= 3.3- 4.6 months, T3=4.7-13.8 months; logrank test p=0.45, cfr Figure 1). When multivariate analysis was performed including Wait-Tx, age at Tx, disease status at Tx ( ≥VGPR vs PR vs
Conclusion
Time frame between PBSC collection and stem cell infusion had no significant impact on the outcome of transplanted myeloma patients. Response to induction treatment and bortezomib based induction therapy are both predictive of better outcome ensuring a longer PFS after transplantation.
Session topic: E-poster
Keyword(s): Autologous, Myeloma, Outcome, Transplant
Abstract: PB1953
Type: Publication Only
Background
Autologous stem cell transplantation (Tx) is still the standard of care for symptomatic myeloma patients (pts) eligible for high-dose procedure. Whether time lasting between stem cell collection and Tx (Wait-Tx) has an impact on Tx outcome itself is matter of debate.
Aims
The aim of this study is to evaluate whether Wait-Tx impacts on the outcome of transplanted myeloma pts
Methods
We reviewed data of 233 myeloma pts treated with HD Melphalan between January 2000 and December 2013; 20 pts with primary refractory disease and 26 pts treated with a double transplant program were excluded. One hundred eighty seven (187) pts entered the analysis: Male/Female 99(53%)/88(47%), median age 55 years (28-69), Myeloma Type IgG/IgA/light chain/non secretory 111(59%)/38(20%)/33(18%)/5(3%), Durie&Salmon stage II/III 26(14%)/161(86%). Induction therapy consisted of 4 VAD cycles in 83 pts (44%) treated from 2000 to 2005 or 4 Bortezomib-based cycles in 104 pts (56%) treated from 2006 to 2013. Stem cell collection was primed with a single course of DCEP or HD-EDX followed by G-CSF at 10 mcg/kg until completing stem cell collection (PBSC). Tx conditioning regimen consisted of single HD-Melphalan infusion 200 mg/m2 in 137 pts (73%); HD Melphalan was given at the reduced dose of 160 mg/m2 in 50 pts (27%) due to comorbidity. Response was defined according to International Myeloma Working Group criteria.
Results
Median time between stem cell collection and transplantation (Wait-Tx) was 4 months (range 0.9-13.8 months). After a median follow up after Tx of 49 months (range 24-75 months), 140 patients (74%) relapsed or progressed, median progression free survival (PFS) after Tx was 23 months (range 12-54 months), with a median OS after Tx of 70 months (range 34 months -not reached). PFS was not different between tertiles of Wait-Tx (T1= 0.9-3.2 months, T2= 3.3- 4.6 months, T3=4.7-13.8 months; logrank test p=0.45, cfr Figure 1). When multivariate analysis was performed including Wait-Tx, age at Tx, disease status at Tx ( ≥VGPR vs PR vs
Conclusion
Time frame between PBSC collection and stem cell infusion had no significant impact on the outcome of transplanted myeloma patients. Response to induction treatment and bortezomib based induction therapy are both predictive of better outcome ensuring a longer PFS after transplantation.
Session topic: E-poster
Keyword(s): Autologous, Myeloma, Outcome, Transplant
Type: Publication Only
Background
Autologous stem cell transplantation (Tx) is still the standard of care for symptomatic myeloma patients (pts) eligible for high-dose procedure. Whether time lasting between stem cell collection and Tx (Wait-Tx) has an impact on Tx outcome itself is matter of debate.
Aims
The aim of this study is to evaluate whether Wait-Tx impacts on the outcome of transplanted myeloma pts
Methods
We reviewed data of 233 myeloma pts treated with HD Melphalan between January 2000 and December 2013; 20 pts with primary refractory disease and 26 pts treated with a double transplant program were excluded. One hundred eighty seven (187) pts entered the analysis: Male/Female 99(53%)/88(47%), median age 55 years (28-69), Myeloma Type IgG/IgA/light chain/non secretory 111(59%)/38(20%)/33(18%)/5(3%), Durie&Salmon stage II/III 26(14%)/161(86%). Induction therapy consisted of 4 VAD cycles in 83 pts (44%) treated from 2000 to 2005 or 4 Bortezomib-based cycles in 104 pts (56%) treated from 2006 to 2013. Stem cell collection was primed with a single course of DCEP or HD-EDX followed by G-CSF at 10 mcg/kg until completing stem cell collection (PBSC). Tx conditioning regimen consisted of single HD-Melphalan infusion 200 mg/m2 in 137 pts (73%); HD Melphalan was given at the reduced dose of 160 mg/m2 in 50 pts (27%) due to comorbidity. Response was defined according to International Myeloma Working Group criteria.
Results
Median time between stem cell collection and transplantation (Wait-Tx) was 4 months (range 0.9-13.8 months). After a median follow up after Tx of 49 months (range 24-75 months), 140 patients (74%) relapsed or progressed, median progression free survival (PFS) after Tx was 23 months (range 12-54 months), with a median OS after Tx of 70 months (range 34 months -not reached). PFS was not different between tertiles of Wait-Tx (T1= 0.9-3.2 months, T2= 3.3- 4.6 months, T3=4.7-13.8 months; logrank test p=0.45, cfr Figure 1). When multivariate analysis was performed including Wait-Tx, age at Tx, disease status at Tx ( ≥VGPR vs PR vs
Conclusion
Time frame between PBSC collection and stem cell infusion had no significant impact on the outcome of transplanted myeloma patients. Response to induction treatment and bortezomib based induction therapy are both predictive of better outcome ensuring a longer PFS after transplantation.
Session topic: E-poster
Keyword(s): Autologous, Myeloma, Outcome, Transplant
{{ help_message }}
{{filter}}


