PREVALENCE OF CYTOPENIAS IN PATIENTS LIVING WITH THE HUMAN IMMUNODEFICIENCY VIRUS. AN OBSERVATIONAL COHORT STUDY.
(Abstract release date: 05/19/16)
EHA Library. de Luca T. 06/09/16; 134790; PB1890

Theofilo Miguel de Luca
Contributions
Contributions
Abstract
Abstract: PB1890
Type: Publication Only
Background
HIV-induced immunosuppression was an important reason for the increased morbidity and mortality. Disorders in haematopoiesis are encountered far less frequently in the current era of highly active antiretroviral therapy (HAART). The expected survival of people living with HIV who are diagnosed early in the course of infection and who have access to modern antivirals now almost equals that of the general population. Ineffective haematopoiesis from direct suppression of bone marrow progenitor cells by HIV infection or indirectly through excessive secretion of inflammatory cytokines induced by HIV, can blunt haematopoiesis. So too can nutritional deficiencies, infiltrative bone marrow disease of infectious or neoplastic origin, and adverse drug effects. Cytopenias play a significant role in the morbidity associated with HIV. Although cytopenias may be poorly documented, they can also impact negatively on quality of life.
Aims
To analyze the prevalence of cytopenias in patients with HIV infection and evaluate the impact of HAART in our patients.
Methods
This is a retrospective study of 108 patients older than 16 years, HIV infected, diagnosed between 2002 - 2014. Their medical histories were analyzed. Data was collected from laboratory at the moment of diagnosis, one year later and two years of follow-up. 98 patients were included in this analysis. We did not include patients with pediatric HIV infection or a history of vertical transmission and patients with loss of follow-up (follow-up less than 2 years).
Results
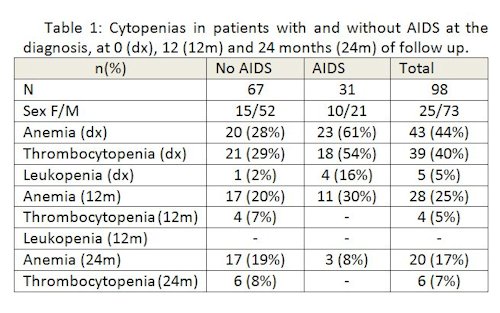
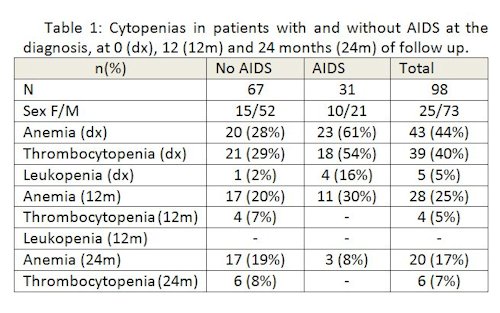
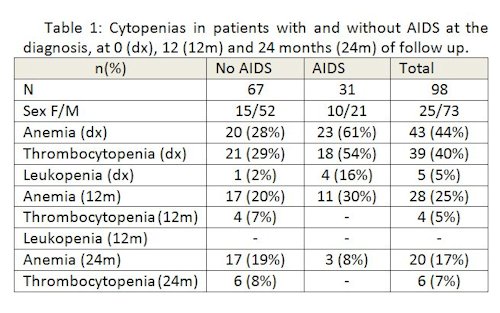
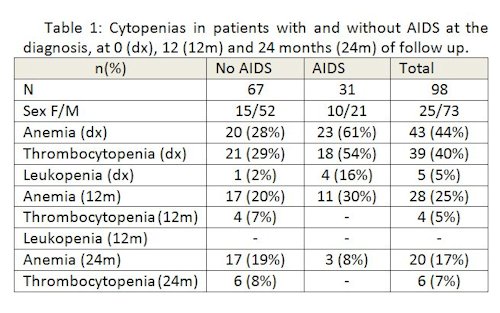
The selected 98 patients showed a median age of 37.7 years (r16-65), 74% were male. At the time of diagnosis, 44% had anemia, 40% thrombocytopenia and 5% leukopenia (table 1). Only 8% of the patients had neutropenia. At the beginning, anemia was present in 48% of female and 36% of male patients. At the time of diagnosis, 31.6% (n31) were diagnosed with AIDS (according to WHO criteria). Out of these 31 patients, 61% had anemia basal vs 28% in those without AIDS at the start (p: 0.001).At 12 months, only 29% of the patients showed anemia, with improvement in both male and female patients compared to the time of diagnosis as well as in the group of patients with initial AIDS. The presence of thrombocytopenia was observed in 5% of the patients. At 24 months of follow-up, 21% had anemia, and only 7% of those who initially had a diagnosis of AIDS. The thrombocytopenia appeared in 7%. None of the patients presented leukopenia at 12 or 24 months.As regards HAART, out of the 98 patients, 64.2% (n:63) received treatment since the diagnosis. Within this group, the emergence of anemia at 1 and at 2 years was 22% and 15% respectively, compared to 24% and 16% in patients who received no treatment at the beginning.Twenty-three of the patients who received zidovudine (AZT) developed anemia after one year of treatment. Those who did not receive AZT, the 27% presented anemia at 12 months. None of the patients who received AZT treatment showed leukopenia at one year of follow-up.
Conclusion
In our experience, the most frequent hematological alteration was anemia, mainly at the time of diagnosis and in patients with AIDS. The haemoglobin level evolved favorably in all patients, regardless of the presence or absence of antiretroviral therapy at the beginning. The thrombocytopenia was more frequent at the time of diagnosis, but it decreased with time. The less frequent cytopenia was the leukopenia, showing no association with HAART.HIV associated cytopenias are very frequent and its appearance occurs mainly at the time of the diagnosis. When faced with this type of cytopenias, it is mandatory to have this infectious disease in mind within the diagnosis algorithm.
Session topic: E-poster
Keyword(s): Anemia, HIV
Type: Publication Only
Background
HIV-induced immunosuppression was an important reason for the increased morbidity and mortality. Disorders in haematopoiesis are encountered far less frequently in the current era of highly active antiretroviral therapy (HAART). The expected survival of people living with HIV who are diagnosed early in the course of infection and who have access to modern antivirals now almost equals that of the general population. Ineffective haematopoiesis from direct suppression of bone marrow progenitor cells by HIV infection or indirectly through excessive secretion of inflammatory cytokines induced by HIV, can blunt haematopoiesis. So too can nutritional deficiencies, infiltrative bone marrow disease of infectious or neoplastic origin, and adverse drug effects. Cytopenias play a significant role in the morbidity associated with HIV. Although cytopenias may be poorly documented, they can also impact negatively on quality of life.
Aims
To analyze the prevalence of cytopenias in patients with HIV infection and evaluate the impact of HAART in our patients.
Methods
This is a retrospective study of 108 patients older than 16 years, HIV infected, diagnosed between 2002 - 2014. Their medical histories were analyzed. Data was collected from laboratory at the moment of diagnosis, one year later and two years of follow-up. 98 patients were included in this analysis. We did not include patients with pediatric HIV infection or a history of vertical transmission and patients with loss of follow-up (follow-up less than 2 years).
Results
The selected 98 patients showed a median age of 37.7 years (r16-65), 74% were male. At the time of diagnosis, 44% had anemia, 40% thrombocytopenia and 5% leukopenia (table 1). Only 8% of the patients had neutropenia. At the beginning, anemia was present in 48% of female and 36% of male patients. At the time of diagnosis, 31.6% (n31) were diagnosed with AIDS (according to WHO criteria). Out of these 31 patients, 61% had anemia basal vs 28% in those without AIDS at the start (p: 0.001).At 12 months, only 29% of the patients showed anemia, with improvement in both male and female patients compared to the time of diagnosis as well as in the group of patients with initial AIDS. The presence of thrombocytopenia was observed in 5% of the patients. At 24 months of follow-up, 21% had anemia, and only 7% of those who initially had a diagnosis of AIDS. The thrombocytopenia appeared in 7%. None of the patients presented leukopenia at 12 or 24 months.As regards HAART, out of the 98 patients, 64.2% (n:63) received treatment since the diagnosis. Within this group, the emergence of anemia at 1 and at 2 years was 22% and 15% respectively, compared to 24% and 16% in patients who received no treatment at the beginning.Twenty-three of the patients who received zidovudine (AZT) developed anemia after one year of treatment. Those who did not receive AZT, the 27% presented anemia at 12 months. None of the patients who received AZT treatment showed leukopenia at one year of follow-up.
Conclusion
In our experience, the most frequent hematological alteration was anemia, mainly at the time of diagnosis and in patients with AIDS. The haemoglobin level evolved favorably in all patients, regardless of the presence or absence of antiretroviral therapy at the beginning. The thrombocytopenia was more frequent at the time of diagnosis, but it decreased with time. The less frequent cytopenia was the leukopenia, showing no association with HAART.HIV associated cytopenias are very frequent and its appearance occurs mainly at the time of the diagnosis. When faced with this type of cytopenias, it is mandatory to have this infectious disease in mind within the diagnosis algorithm.
Session topic: E-poster
Keyword(s): Anemia, HIV
Abstract: PB1890
Type: Publication Only
Background
HIV-induced immunosuppression was an important reason for the increased morbidity and mortality. Disorders in haematopoiesis are encountered far less frequently in the current era of highly active antiretroviral therapy (HAART). The expected survival of people living with HIV who are diagnosed early in the course of infection and who have access to modern antivirals now almost equals that of the general population. Ineffective haematopoiesis from direct suppression of bone marrow progenitor cells by HIV infection or indirectly through excessive secretion of inflammatory cytokines induced by HIV, can blunt haematopoiesis. So too can nutritional deficiencies, infiltrative bone marrow disease of infectious or neoplastic origin, and adverse drug effects. Cytopenias play a significant role in the morbidity associated with HIV. Although cytopenias may be poorly documented, they can also impact negatively on quality of life.
Aims
To analyze the prevalence of cytopenias in patients with HIV infection and evaluate the impact of HAART in our patients.
Methods
This is a retrospective study of 108 patients older than 16 years, HIV infected, diagnosed between 2002 - 2014. Their medical histories were analyzed. Data was collected from laboratory at the moment of diagnosis, one year later and two years of follow-up. 98 patients were included in this analysis. We did not include patients with pediatric HIV infection or a history of vertical transmission and patients with loss of follow-up (follow-up less than 2 years).
Results
The selected 98 patients showed a median age of 37.7 years (r16-65), 74% were male. At the time of diagnosis, 44% had anemia, 40% thrombocytopenia and 5% leukopenia (table 1). Only 8% of the patients had neutropenia. At the beginning, anemia was present in 48% of female and 36% of male patients. At the time of diagnosis, 31.6% (n31) were diagnosed with AIDS (according to WHO criteria). Out of these 31 patients, 61% had anemia basal vs 28% in those without AIDS at the start (p: 0.001).At 12 months, only 29% of the patients showed anemia, with improvement in both male and female patients compared to the time of diagnosis as well as in the group of patients with initial AIDS. The presence of thrombocytopenia was observed in 5% of the patients. At 24 months of follow-up, 21% had anemia, and only 7% of those who initially had a diagnosis of AIDS. The thrombocytopenia appeared in 7%. None of the patients presented leukopenia at 12 or 24 months.As regards HAART, out of the 98 patients, 64.2% (n:63) received treatment since the diagnosis. Within this group, the emergence of anemia at 1 and at 2 years was 22% and 15% respectively, compared to 24% and 16% in patients who received no treatment at the beginning.Twenty-three of the patients who received zidovudine (AZT) developed anemia after one year of treatment. Those who did not receive AZT, the 27% presented anemia at 12 months. None of the patients who received AZT treatment showed leukopenia at one year of follow-up.
Conclusion
In our experience, the most frequent hematological alteration was anemia, mainly at the time of diagnosis and in patients with AIDS. The haemoglobin level evolved favorably in all patients, regardless of the presence or absence of antiretroviral therapy at the beginning. The thrombocytopenia was more frequent at the time of diagnosis, but it decreased with time. The less frequent cytopenia was the leukopenia, showing no association with HAART.HIV associated cytopenias are very frequent and its appearance occurs mainly at the time of the diagnosis. When faced with this type of cytopenias, it is mandatory to have this infectious disease in mind within the diagnosis algorithm.
Session topic: E-poster
Keyword(s): Anemia, HIV
Type: Publication Only
Background
HIV-induced immunosuppression was an important reason for the increased morbidity and mortality. Disorders in haematopoiesis are encountered far less frequently in the current era of highly active antiretroviral therapy (HAART). The expected survival of people living with HIV who are diagnosed early in the course of infection and who have access to modern antivirals now almost equals that of the general population. Ineffective haematopoiesis from direct suppression of bone marrow progenitor cells by HIV infection or indirectly through excessive secretion of inflammatory cytokines induced by HIV, can blunt haematopoiesis. So too can nutritional deficiencies, infiltrative bone marrow disease of infectious or neoplastic origin, and adverse drug effects. Cytopenias play a significant role in the morbidity associated with HIV. Although cytopenias may be poorly documented, they can also impact negatively on quality of life.
Aims
To analyze the prevalence of cytopenias in patients with HIV infection and evaluate the impact of HAART in our patients.
Methods
This is a retrospective study of 108 patients older than 16 years, HIV infected, diagnosed between 2002 - 2014. Their medical histories were analyzed. Data was collected from laboratory at the moment of diagnosis, one year later and two years of follow-up. 98 patients were included in this analysis. We did not include patients with pediatric HIV infection or a history of vertical transmission and patients with loss of follow-up (follow-up less than 2 years).
Results
The selected 98 patients showed a median age of 37.7 years (r16-65), 74% were male. At the time of diagnosis, 44% had anemia, 40% thrombocytopenia and 5% leukopenia (table 1). Only 8% of the patients had neutropenia. At the beginning, anemia was present in 48% of female and 36% of male patients. At the time of diagnosis, 31.6% (n31) were diagnosed with AIDS (according to WHO criteria). Out of these 31 patients, 61% had anemia basal vs 28% in those without AIDS at the start (p: 0.001).At 12 months, only 29% of the patients showed anemia, with improvement in both male and female patients compared to the time of diagnosis as well as in the group of patients with initial AIDS. The presence of thrombocytopenia was observed in 5% of the patients. At 24 months of follow-up, 21% had anemia, and only 7% of those who initially had a diagnosis of AIDS. The thrombocytopenia appeared in 7%. None of the patients presented leukopenia at 12 or 24 months.As regards HAART, out of the 98 patients, 64.2% (n:63) received treatment since the diagnosis. Within this group, the emergence of anemia at 1 and at 2 years was 22% and 15% respectively, compared to 24% and 16% in patients who received no treatment at the beginning.Twenty-three of the patients who received zidovudine (AZT) developed anemia after one year of treatment. Those who did not receive AZT, the 27% presented anemia at 12 months. None of the patients who received AZT treatment showed leukopenia at one year of follow-up.
Conclusion
In our experience, the most frequent hematological alteration was anemia, mainly at the time of diagnosis and in patients with AIDS. The haemoglobin level evolved favorably in all patients, regardless of the presence or absence of antiretroviral therapy at the beginning. The thrombocytopenia was more frequent at the time of diagnosis, but it decreased with time. The less frequent cytopenia was the leukopenia, showing no association with HAART.HIV associated cytopenias are very frequent and its appearance occurs mainly at the time of the diagnosis. When faced with this type of cytopenias, it is mandatory to have this infectious disease in mind within the diagnosis algorithm.
Session topic: E-poster
Keyword(s): Anemia, HIV
{{ help_message }}
{{filter}}


