THE POSITIVE IMPACT OF ANTIMICROBIAL STEWARDSHIP IN THE BIGGEST PEDIATRIC HAEMATOLOGY ONCOLOGY CENTRE, RUSSIA
(Abstract release date: 05/19/16)
EHA Library. Solopova G. 06/09/16; 134786; PB1886

Dr. Galina Solopova
Contributions
Contributions
Abstract
Abstract: PB1886
Type: Publication Only
Background
Multidrug resistant organisms (MDRO) are the emerging problem across the world, and one of the most effective and mandatory steps in solving it is optimization of antibiotics use. Here we present the first results of the fight against MDRO at the Dmitry Rogachev Center for Pediatric Hematology, Oncology and Immunology, Moscow, Russia (Center).
Aims
The Infection Prevention and Control Department (IPCD) has made a number of steps to rationalize the use of anti-infectives.
Methods
On January 1st, 2014, the algorithm for empirical anti-infective therapy in febrile neutropenia was implemented. It included recommendations for first line (empiric) antibacterial therapy (in accordance with the patient’s risk group), spectrum of recommended evaluation tests and rules for treatment modification. For example, fluoroquinolones and ceftazidime were excluded from empiric therapy and reserved for the targeted one only. The same recommendations were made regarding tigecycline and ertapenem.Another step was the implementation of guidelines for perioperative antibiotic therapy, with cephalosporins I-II regarded as the drugs of choice in most of cases. Along with those measures, precise control of antibiotics and antifungals discontinuation was established.For the evaluation of the effectiveness of the results we have calculated the use of the most common classes of antibiotics and antifungals (per 100 bed-days)—before the intervention and a year after it. Microorganisms’-wise drug resistance index (DRI) was also calculated.
Results
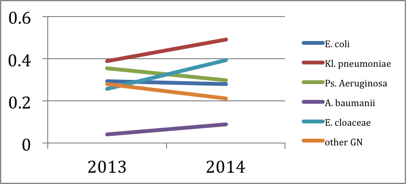
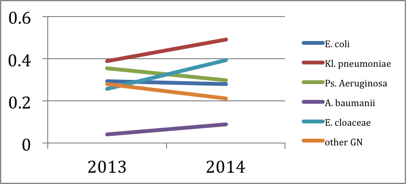
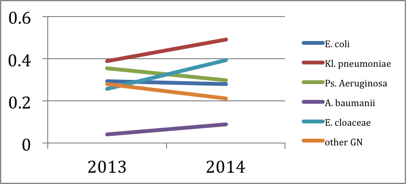
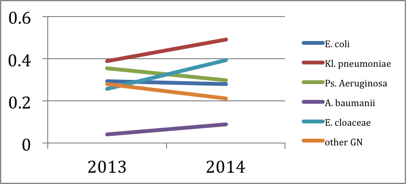
Having compared the respective rates before and after the intervention, we detected the overall decrease of use in vancomycin (64%), piperacillin/tazobactam (15%), aminoglycosides (15%) and fluoroquinolones (7%) in all the Center’s departments. Calculated separately, the rates were significantly higher for the intensive care unit, where interaction compliance with the IPCD was the highest: reduction of aminoglycosides use—58%, fluoroquinolones —66%, cephalosporins III-IV—8%, vancomycin—82,5%, piperacillin/tazobactam—52%, carbapenems—20%, linezolid —47%. The use of colistin remained on the same level, while the use of tigecycline raised 35%.As for antifungals, the analysis showed a 75% reduction of use in amphotericin B and an 18% reduction in case of voriconazole. Posaconazole raised 25%. Although echinocandins were used as the drugs of choice in empiric antifungal therapy in febrile neutropenia algorithm (in accordance with the ECIL recommendations), their use remained on the same level.During the surveillance period DRI levels for P. aeruginosa and E. coli dropped down (graph 1).In terms of money, the reduction of anti-infectives use have saved the Center around €500,000 in 12 months. It is important to mention that the rates of infections-related mortality has not increased since the intervention (26 in 2013 compared to 16 in 2014).
Conclusion
The reduction of antibiotics and antifungals use and as a result — the decrease of microbial resistance and money savings in hematology/oncology hospital is an achievable goal. Every hospital should make the effort to initiate and sustain an effective Antimicrobial Stewardship Program.
Session topic: E-poster
Keyword(s): Hematological malignancy, MDR, Pediatric
Type: Publication Only
Background
Multidrug resistant organisms (MDRO) are the emerging problem across the world, and one of the most effective and mandatory steps in solving it is optimization of antibiotics use. Here we present the first results of the fight against MDRO at the Dmitry Rogachev Center for Pediatric Hematology, Oncology and Immunology, Moscow, Russia (Center).
Aims
The Infection Prevention and Control Department (IPCD) has made a number of steps to rationalize the use of anti-infectives.
Methods
On January 1st, 2014, the algorithm for empirical anti-infective therapy in febrile neutropenia was implemented. It included recommendations for first line (empiric) antibacterial therapy (in accordance with the patient’s risk group), spectrum of recommended evaluation tests and rules for treatment modification. For example, fluoroquinolones and ceftazidime were excluded from empiric therapy and reserved for the targeted one only. The same recommendations were made regarding tigecycline and ertapenem.Another step was the implementation of guidelines for perioperative antibiotic therapy, with cephalosporins I-II regarded as the drugs of choice in most of cases. Along with those measures, precise control of antibiotics and antifungals discontinuation was established.For the evaluation of the effectiveness of the results we have calculated the use of the most common classes of antibiotics and antifungals (per 100 bed-days)—before the intervention and a year after it. Microorganisms’-wise drug resistance index (DRI) was also calculated.
Results
Having compared the respective rates before and after the intervention, we detected the overall decrease of use in vancomycin (64%), piperacillin/tazobactam (15%), aminoglycosides (15%) and fluoroquinolones (7%) in all the Center’s departments. Calculated separately, the rates were significantly higher for the intensive care unit, where interaction compliance with the IPCD was the highest: reduction of aminoglycosides use—58%, fluoroquinolones —66%, cephalosporins III-IV—8%, vancomycin—82,5%, piperacillin/tazobactam—52%, carbapenems—20%, linezolid —47%. The use of colistin remained on the same level, while the use of tigecycline raised 35%.As for antifungals, the analysis showed a 75% reduction of use in amphotericin B and an 18% reduction in case of voriconazole. Posaconazole raised 25%. Although echinocandins were used as the drugs of choice in empiric antifungal therapy in febrile neutropenia algorithm (in accordance with the ECIL recommendations), their use remained on the same level.During the surveillance period DRI levels for P. aeruginosa and E. coli dropped down (graph 1).In terms of money, the reduction of anti-infectives use have saved the Center around €500,000 in 12 months. It is important to mention that the rates of infections-related mortality has not increased since the intervention (26 in 2013 compared to 16 in 2014).
Conclusion
The reduction of antibiotics and antifungals use and as a result — the decrease of microbial resistance and money savings in hematology/oncology hospital is an achievable goal. Every hospital should make the effort to initiate and sustain an effective Antimicrobial Stewardship Program.
Session topic: E-poster
Keyword(s): Hematological malignancy, MDR, Pediatric
Abstract: PB1886
Type: Publication Only
Background
Multidrug resistant organisms (MDRO) are the emerging problem across the world, and one of the most effective and mandatory steps in solving it is optimization of antibiotics use. Here we present the first results of the fight against MDRO at the Dmitry Rogachev Center for Pediatric Hematology, Oncology and Immunology, Moscow, Russia (Center).
Aims
The Infection Prevention and Control Department (IPCD) has made a number of steps to rationalize the use of anti-infectives.
Methods
On January 1st, 2014, the algorithm for empirical anti-infective therapy in febrile neutropenia was implemented. It included recommendations for first line (empiric) antibacterial therapy (in accordance with the patient’s risk group), spectrum of recommended evaluation tests and rules for treatment modification. For example, fluoroquinolones and ceftazidime were excluded from empiric therapy and reserved for the targeted one only. The same recommendations were made regarding tigecycline and ertapenem.Another step was the implementation of guidelines for perioperative antibiotic therapy, with cephalosporins I-II regarded as the drugs of choice in most of cases. Along with those measures, precise control of antibiotics and antifungals discontinuation was established.For the evaluation of the effectiveness of the results we have calculated the use of the most common classes of antibiotics and antifungals (per 100 bed-days)—before the intervention and a year after it. Microorganisms’-wise drug resistance index (DRI) was also calculated.
Results
Having compared the respective rates before and after the intervention, we detected the overall decrease of use in vancomycin (64%), piperacillin/tazobactam (15%), aminoglycosides (15%) and fluoroquinolones (7%) in all the Center’s departments. Calculated separately, the rates were significantly higher for the intensive care unit, where interaction compliance with the IPCD was the highest: reduction of aminoglycosides use—58%, fluoroquinolones —66%, cephalosporins III-IV—8%, vancomycin—82,5%, piperacillin/tazobactam—52%, carbapenems—20%, linezolid —47%. The use of colistin remained on the same level, while the use of tigecycline raised 35%.As for antifungals, the analysis showed a 75% reduction of use in amphotericin B and an 18% reduction in case of voriconazole. Posaconazole raised 25%. Although echinocandins were used as the drugs of choice in empiric antifungal therapy in febrile neutropenia algorithm (in accordance with the ECIL recommendations), their use remained on the same level.During the surveillance period DRI levels for P. aeruginosa and E. coli dropped down (graph 1).In terms of money, the reduction of anti-infectives use have saved the Center around €500,000 in 12 months. It is important to mention that the rates of infections-related mortality has not increased since the intervention (26 in 2013 compared to 16 in 2014).
Conclusion
The reduction of antibiotics and antifungals use and as a result — the decrease of microbial resistance and money savings in hematology/oncology hospital is an achievable goal. Every hospital should make the effort to initiate and sustain an effective Antimicrobial Stewardship Program.
Session topic: E-poster
Keyword(s): Hematological malignancy, MDR, Pediatric
Type: Publication Only
Background
Multidrug resistant organisms (MDRO) are the emerging problem across the world, and one of the most effective and mandatory steps in solving it is optimization of antibiotics use. Here we present the first results of the fight against MDRO at the Dmitry Rogachev Center for Pediatric Hematology, Oncology and Immunology, Moscow, Russia (Center).
Aims
The Infection Prevention and Control Department (IPCD) has made a number of steps to rationalize the use of anti-infectives.
Methods
On January 1st, 2014, the algorithm for empirical anti-infective therapy in febrile neutropenia was implemented. It included recommendations for first line (empiric) antibacterial therapy (in accordance with the patient’s risk group), spectrum of recommended evaluation tests and rules for treatment modification. For example, fluoroquinolones and ceftazidime were excluded from empiric therapy and reserved for the targeted one only. The same recommendations were made regarding tigecycline and ertapenem.Another step was the implementation of guidelines for perioperative antibiotic therapy, with cephalosporins I-II regarded as the drugs of choice in most of cases. Along with those measures, precise control of antibiotics and antifungals discontinuation was established.For the evaluation of the effectiveness of the results we have calculated the use of the most common classes of antibiotics and antifungals (per 100 bed-days)—before the intervention and a year after it. Microorganisms’-wise drug resistance index (DRI) was also calculated.
Results
Having compared the respective rates before and after the intervention, we detected the overall decrease of use in vancomycin (64%), piperacillin/tazobactam (15%), aminoglycosides (15%) and fluoroquinolones (7%) in all the Center’s departments. Calculated separately, the rates were significantly higher for the intensive care unit, where interaction compliance with the IPCD was the highest: reduction of aminoglycosides use—58%, fluoroquinolones —66%, cephalosporins III-IV—8%, vancomycin—82,5%, piperacillin/tazobactam—52%, carbapenems—20%, linezolid —47%. The use of colistin remained on the same level, while the use of tigecycline raised 35%.As for antifungals, the analysis showed a 75% reduction of use in amphotericin B and an 18% reduction in case of voriconazole. Posaconazole raised 25%. Although echinocandins were used as the drugs of choice in empiric antifungal therapy in febrile neutropenia algorithm (in accordance with the ECIL recommendations), their use remained on the same level.During the surveillance period DRI levels for P. aeruginosa and E. coli dropped down (graph 1).In terms of money, the reduction of anti-infectives use have saved the Center around €500,000 in 12 months. It is important to mention that the rates of infections-related mortality has not increased since the intervention (26 in 2013 compared to 16 in 2014).
Conclusion
The reduction of antibiotics and antifungals use and as a result — the decrease of microbial resistance and money savings in hematology/oncology hospital is an achievable goal. Every hospital should make the effort to initiate and sustain an effective Antimicrobial Stewardship Program.
Session topic: E-poster
Keyword(s): Hematological malignancy, MDR, Pediatric
{{ help_message }}
{{filter}}


