RISK FACTORS AND MICROBIOLOGICAL FEATURES OF BLOODSTREAM NONTYPHOIDAL SALMONELLA INFECTION IN ADULT PATIENTS RECEIVING ALLOGENEIC HEMATOPOIETIC STEM CELL TRANSPLANTATION
(Abstract release date: 05/19/16)
EHA Library. Ko P. 06/09/16; 134783; PB1883

Mr. Po-Shen Ko
Contributions
Contributions
Abstract
Abstract: PB1883
Type: Publication Only
Background
In patients receiving allogeniec hematopoietic stem cell transplantation (allo-HSCT), it is not uncommon to encounter post-transplant infection and/or acute or chronic graft-versus-host disease (aGVHD or cGVHD) which commonly involve gastrointestinal tract and liver. Thus, post allo-HSCT patients might be vulnerable to foodborne pathogens, such as nontyphoidal salmonella (NTS) infection. To the best of our knowledge, very few reports discuss this issue of post allo-HSCT bloodstream NTS infection. We retrospectively analyzed the clinical risk factors and microbiological features of bloodstream NTS infection among adult allo-HSCT recipients during a 12-year period in our institution.
Aims
To determine the survival outcomes, the risk factors and microbiological features of bloodstream nontyphoiidal salmonella infection in adult allo-HSCT recipients.
Methods
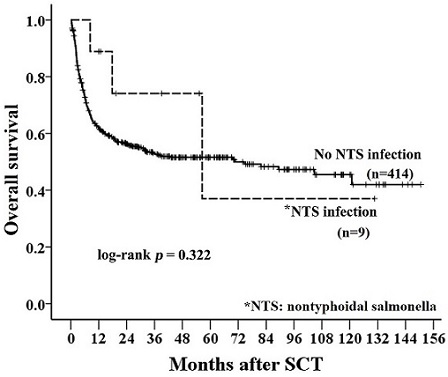
We retrospectively reviewed adult (age≥ 18 years) allo-HSCT recipients between 2003 and 2014 with regular follow-up till October 2015. Pre-transplant and transplant-related clinical data were collected. Myeloablative conditioning included busulfan (4mg/kg/day for 4 days) and cyclophosphamide (60mg/kg/day for 2 days), or total body irradiation (TBI) of 12 Gy combined with cyclophosphamide (60 mg/kg/day for 2 days). Fludarabine-based conditioning were administered to elderly patients or with comorbidities. Standard protocol with cyclosporin (i.v 3.0 mg/kg/day in 2 split doses with dose being adjusted to maintain trough plasma level at 100-250 ug/L) and short-term low dose methotrexate were adopted for GVHD prophylaxis. Recipients of unrelated donor transplants also recieved anti-thymocyte globulin (2mg/kg/day for 3 days). The overall survival (OS) in patients with or without bloodstream NTS infection was analyzed by Kaplan-Meier method. A log-rank test was used to compare survival curves for statistical significance. Odds ratios (ORs) and the 95% confidence interval (CI) were calculated using logistic regression models. We used multivariate logistic regression models to calculate odds ratios while adjusting for possible independent confounding factors. All risk factors with p<0.1 in the univariate model further entered into the multivariate analysis. All statistical testing was performed using 2-tailed tests; p< 0.05 was considered statistically significant.
Results
Total nine patients (2.13%) of 423 patients recieving allo-HSCT experienced post-tansplant bloodstream NTS infection in a median onset of 315 days after HSCT. As for the nine with NTS infection, fever was a majorly presenitng symptom. Metastatic infection of knee joint occurred in 2 patients. One suffered from concurrent bloodstream NTS infection and spetic arthritis and the other one had subsequent septic arthritis after 42 days of bloodstream NTS infection. Salmonella group D was cultured in eight out of nine patients (89%). Of note, among the 9 bloodstream NTS infection, 7 patients had cGVHD, 5 of whom suffered from extensive cGVHD. Fortunately, all patients recovered with antibiotic therapy, which comprised of a at least third-generation cephalosporin or a quinolone or both. In addition, in patients with or without bloodstream NTS infection, there was no statistical difference of post-transplant survival (p = 0.322; Figure). After multivariate analysis, there were statistical significances in patients receiving non-myeloablative conditioning (OR: 4.604; 95% CI: 1.098–19.308; p = 0.037) and post-transplant extensive cGVHD (OR: 8.054; 95% CI: 2.048–31.674; p = 0.003).
Conclusion
In a cohort of 423 adult patients recieving allogeneic hematopoietic SCT, 9 patients (2.13%) developed post-transplant NTS infection, including two patients had subsequent or combined metastatic infection. Multivariate analysis revealed that extensive chronic graft-versus-host disease (GVHD) (OR 8.054, p = 0.003) and non-myeloablative transplant conditioning (OR 4.604, p = 0.037) were significant risk factors for NTS infection. Our study determined the risk factors and microbiological features for this infection.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, Infection, Risk factor
Type: Publication Only
Background
In patients receiving allogeniec hematopoietic stem cell transplantation (allo-HSCT), it is not uncommon to encounter post-transplant infection and/or acute or chronic graft-versus-host disease (aGVHD or cGVHD) which commonly involve gastrointestinal tract and liver. Thus, post allo-HSCT patients might be vulnerable to foodborne pathogens, such as nontyphoidal salmonella (NTS) infection. To the best of our knowledge, very few reports discuss this issue of post allo-HSCT bloodstream NTS infection. We retrospectively analyzed the clinical risk factors and microbiological features of bloodstream NTS infection among adult allo-HSCT recipients during a 12-year period in our institution.
Aims
To determine the survival outcomes, the risk factors and microbiological features of bloodstream nontyphoiidal salmonella infection in adult allo-HSCT recipients.
Methods
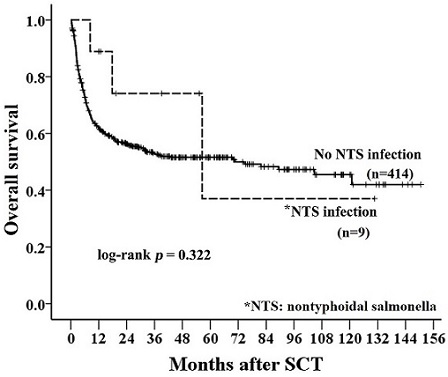
We retrospectively reviewed adult (age≥ 18 years) allo-HSCT recipients between 2003 and 2014 with regular follow-up till October 2015. Pre-transplant and transplant-related clinical data were collected. Myeloablative conditioning included busulfan (4mg/kg/day for 4 days) and cyclophosphamide (60mg/kg/day for 2 days), or total body irradiation (TBI) of 12 Gy combined with cyclophosphamide (60 mg/kg/day for 2 days). Fludarabine-based conditioning were administered to elderly patients or with comorbidities. Standard protocol with cyclosporin (i.v 3.0 mg/kg/day in 2 split doses with dose being adjusted to maintain trough plasma level at 100-250 ug/L) and short-term low dose methotrexate were adopted for GVHD prophylaxis. Recipients of unrelated donor transplants also recieved anti-thymocyte globulin (2mg/kg/day for 3 days). The overall survival (OS) in patients with or without bloodstream NTS infection was analyzed by Kaplan-Meier method. A log-rank test was used to compare survival curves for statistical significance. Odds ratios (ORs) and the 95% confidence interval (CI) were calculated using logistic regression models. We used multivariate logistic regression models to calculate odds ratios while adjusting for possible independent confounding factors. All risk factors with p<0.1 in the univariate model further entered into the multivariate analysis. All statistical testing was performed using 2-tailed tests; p< 0.05 was considered statistically significant.
Results
Total nine patients (2.13%) of 423 patients recieving allo-HSCT experienced post-tansplant bloodstream NTS infection in a median onset of 315 days after HSCT. As for the nine with NTS infection, fever was a majorly presenitng symptom. Metastatic infection of knee joint occurred in 2 patients. One suffered from concurrent bloodstream NTS infection and spetic arthritis and the other one had subsequent septic arthritis after 42 days of bloodstream NTS infection. Salmonella group D was cultured in eight out of nine patients (89%). Of note, among the 9 bloodstream NTS infection, 7 patients had cGVHD, 5 of whom suffered from extensive cGVHD. Fortunately, all patients recovered with antibiotic therapy, which comprised of a at least third-generation cephalosporin or a quinolone or both. In addition, in patients with or without bloodstream NTS infection, there was no statistical difference of post-transplant survival (p = 0.322; Figure). After multivariate analysis, there were statistical significances in patients receiving non-myeloablative conditioning (OR: 4.604; 95% CI: 1.098–19.308; p = 0.037) and post-transplant extensive cGVHD (OR: 8.054; 95% CI: 2.048–31.674; p = 0.003).
Conclusion
In a cohort of 423 adult patients recieving allogeneic hematopoietic SCT, 9 patients (2.13%) developed post-transplant NTS infection, including two patients had subsequent or combined metastatic infection. Multivariate analysis revealed that extensive chronic graft-versus-host disease (GVHD) (OR 8.054, p = 0.003) and non-myeloablative transplant conditioning (OR 4.604, p = 0.037) were significant risk factors for NTS infection. Our study determined the risk factors and microbiological features for this infection.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, Infection, Risk factor
Abstract: PB1883
Type: Publication Only
Background
In patients receiving allogeniec hematopoietic stem cell transplantation (allo-HSCT), it is not uncommon to encounter post-transplant infection and/or acute or chronic graft-versus-host disease (aGVHD or cGVHD) which commonly involve gastrointestinal tract and liver. Thus, post allo-HSCT patients might be vulnerable to foodborne pathogens, such as nontyphoidal salmonella (NTS) infection. To the best of our knowledge, very few reports discuss this issue of post allo-HSCT bloodstream NTS infection. We retrospectively analyzed the clinical risk factors and microbiological features of bloodstream NTS infection among adult allo-HSCT recipients during a 12-year period in our institution.
Aims
To determine the survival outcomes, the risk factors and microbiological features of bloodstream nontyphoiidal salmonella infection in adult allo-HSCT recipients.
Methods
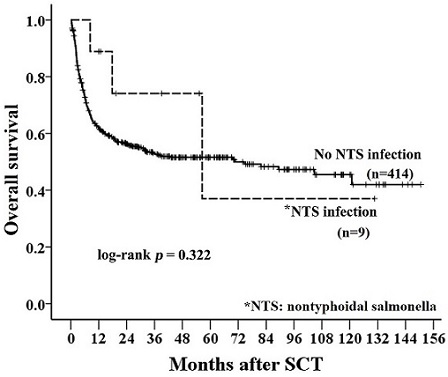
We retrospectively reviewed adult (age≥ 18 years) allo-HSCT recipients between 2003 and 2014 with regular follow-up till October 2015. Pre-transplant and transplant-related clinical data were collected. Myeloablative conditioning included busulfan (4mg/kg/day for 4 days) and cyclophosphamide (60mg/kg/day for 2 days), or total body irradiation (TBI) of 12 Gy combined with cyclophosphamide (60 mg/kg/day for 2 days). Fludarabine-based conditioning were administered to elderly patients or with comorbidities. Standard protocol with cyclosporin (i.v 3.0 mg/kg/day in 2 split doses with dose being adjusted to maintain trough plasma level at 100-250 ug/L) and short-term low dose methotrexate were adopted for GVHD prophylaxis. Recipients of unrelated donor transplants also recieved anti-thymocyte globulin (2mg/kg/day for 3 days). The overall survival (OS) in patients with or without bloodstream NTS infection was analyzed by Kaplan-Meier method. A log-rank test was used to compare survival curves for statistical significance. Odds ratios (ORs) and the 95% confidence interval (CI) were calculated using logistic regression models. We used multivariate logistic regression models to calculate odds ratios while adjusting for possible independent confounding factors. All risk factors with p<0.1 in the univariate model further entered into the multivariate analysis. All statistical testing was performed using 2-tailed tests; p< 0.05 was considered statistically significant.
Results
Total nine patients (2.13%) of 423 patients recieving allo-HSCT experienced post-tansplant bloodstream NTS infection in a median onset of 315 days after HSCT. As for the nine with NTS infection, fever was a majorly presenitng symptom. Metastatic infection of knee joint occurred in 2 patients. One suffered from concurrent bloodstream NTS infection and spetic arthritis and the other one had subsequent septic arthritis after 42 days of bloodstream NTS infection. Salmonella group D was cultured in eight out of nine patients (89%). Of note, among the 9 bloodstream NTS infection, 7 patients had cGVHD, 5 of whom suffered from extensive cGVHD. Fortunately, all patients recovered with antibiotic therapy, which comprised of a at least third-generation cephalosporin or a quinolone or both. In addition, in patients with or without bloodstream NTS infection, there was no statistical difference of post-transplant survival (p = 0.322; Figure). After multivariate analysis, there were statistical significances in patients receiving non-myeloablative conditioning (OR: 4.604; 95% CI: 1.098–19.308; p = 0.037) and post-transplant extensive cGVHD (OR: 8.054; 95% CI: 2.048–31.674; p = 0.003).
Conclusion
In a cohort of 423 adult patients recieving allogeneic hematopoietic SCT, 9 patients (2.13%) developed post-transplant NTS infection, including two patients had subsequent or combined metastatic infection. Multivariate analysis revealed that extensive chronic graft-versus-host disease (GVHD) (OR 8.054, p = 0.003) and non-myeloablative transplant conditioning (OR 4.604, p = 0.037) were significant risk factors for NTS infection. Our study determined the risk factors and microbiological features for this infection.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, Infection, Risk factor
Type: Publication Only
Background
In patients receiving allogeniec hematopoietic stem cell transplantation (allo-HSCT), it is not uncommon to encounter post-transplant infection and/or acute or chronic graft-versus-host disease (aGVHD or cGVHD) which commonly involve gastrointestinal tract and liver. Thus, post allo-HSCT patients might be vulnerable to foodborne pathogens, such as nontyphoidal salmonella (NTS) infection. To the best of our knowledge, very few reports discuss this issue of post allo-HSCT bloodstream NTS infection. We retrospectively analyzed the clinical risk factors and microbiological features of bloodstream NTS infection among adult allo-HSCT recipients during a 12-year period in our institution.
Aims
To determine the survival outcomes, the risk factors and microbiological features of bloodstream nontyphoiidal salmonella infection in adult allo-HSCT recipients.
Methods
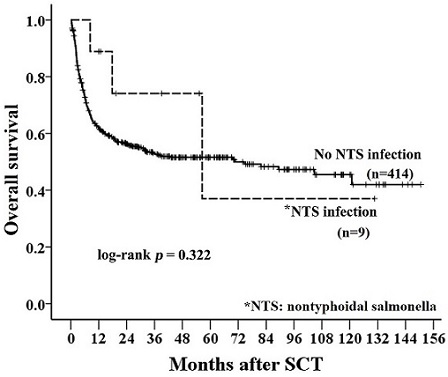
We retrospectively reviewed adult (age≥ 18 years) allo-HSCT recipients between 2003 and 2014 with regular follow-up till October 2015. Pre-transplant and transplant-related clinical data were collected. Myeloablative conditioning included busulfan (4mg/kg/day for 4 days) and cyclophosphamide (60mg/kg/day for 2 days), or total body irradiation (TBI) of 12 Gy combined with cyclophosphamide (60 mg/kg/day for 2 days). Fludarabine-based conditioning were administered to elderly patients or with comorbidities. Standard protocol with cyclosporin (i.v 3.0 mg/kg/day in 2 split doses with dose being adjusted to maintain trough plasma level at 100-250 ug/L) and short-term low dose methotrexate were adopted for GVHD prophylaxis. Recipients of unrelated donor transplants also recieved anti-thymocyte globulin (2mg/kg/day for 3 days). The overall survival (OS) in patients with or without bloodstream NTS infection was analyzed by Kaplan-Meier method. A log-rank test was used to compare survival curves for statistical significance. Odds ratios (ORs) and the 95% confidence interval (CI) were calculated using logistic regression models. We used multivariate logistic regression models to calculate odds ratios while adjusting for possible independent confounding factors. All risk factors with p<0.1 in the univariate model further entered into the multivariate analysis. All statistical testing was performed using 2-tailed tests; p< 0.05 was considered statistically significant.
Results
Total nine patients (2.13%) of 423 patients recieving allo-HSCT experienced post-tansplant bloodstream NTS infection in a median onset of 315 days after HSCT. As for the nine with NTS infection, fever was a majorly presenitng symptom. Metastatic infection of knee joint occurred in 2 patients. One suffered from concurrent bloodstream NTS infection and spetic arthritis and the other one had subsequent septic arthritis after 42 days of bloodstream NTS infection. Salmonella group D was cultured in eight out of nine patients (89%). Of note, among the 9 bloodstream NTS infection, 7 patients had cGVHD, 5 of whom suffered from extensive cGVHD. Fortunately, all patients recovered with antibiotic therapy, which comprised of a at least third-generation cephalosporin or a quinolone or both. In addition, in patients with or without bloodstream NTS infection, there was no statistical difference of post-transplant survival (p = 0.322; Figure). After multivariate analysis, there were statistical significances in patients receiving non-myeloablative conditioning (OR: 4.604; 95% CI: 1.098–19.308; p = 0.037) and post-transplant extensive cGVHD (OR: 8.054; 95% CI: 2.048–31.674; p = 0.003).
Conclusion
In a cohort of 423 adult patients recieving allogeneic hematopoietic SCT, 9 patients (2.13%) developed post-transplant NTS infection, including two patients had subsequent or combined metastatic infection. Multivariate analysis revealed that extensive chronic graft-versus-host disease (GVHD) (OR 8.054, p = 0.003) and non-myeloablative transplant conditioning (OR 4.604, p = 0.037) were significant risk factors for NTS infection. Our study determined the risk factors and microbiological features for this infection.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, Infection, Risk factor
{{ help_message }}
{{filter}}


