RISK OF HISTOLOGIC TRANSFORMATION (HT) IN SPLENIC MARGINAL ZONE LYMPHOMA (SMZL) PATIENTS TREATED WITH RITUXIMAB
(Abstract release date: 05/19/16)
EHA Library. Kalpadakis C. 06/09/16; 134767; PB1867

Assoc. Prof. Christina Kalpadakis
Contributions
Contributions
Abstract
Abstract: PB1867
Type: Publication Only
Background
SMZL is an indolent lymphoma with long survival. The risk of HT is not well defined, ranging between <5% to >20% in various reports. Rituximab has shown significant activity in the treatment of SMZL. In the rituximab era there is no study assessing the incidence of HT in SMZL patients.
Aims
To analyze the incidence and risk factors for HT in a large series of SMZL patients homogeneously treated with rituximab.
Methods
The studied cohort included 89 SMZL patients diagnosed and treated between 2003 and 2015 exclusively with rituximab monotherapy as first line treatment. 41% were males with a median age of 65 years (range, 41-95). 6/89 (7%) presented with B-symptoms and 43% with elevated LDH. According to IPI, 31% were classified as intermediate high and high risk. No patient was HCV(+). The response rate to rituximab was 95%. HT was confirmed by detailed immunomorphologic study and defined by a biopsy-proven transformation of previous SMZL into an aggressive entity. Overall survival (OS) and progression free survival (PFS) were estimated by the Kaplan-Meier method.
Results
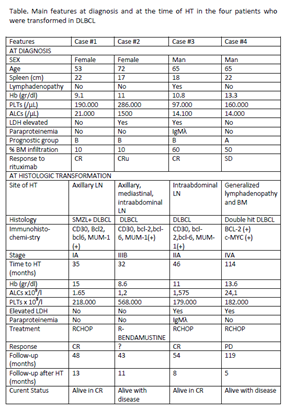
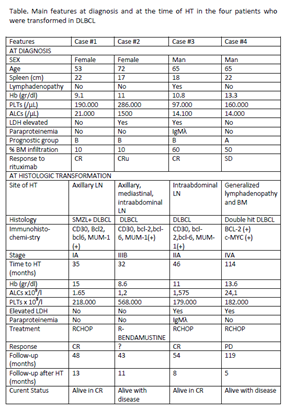
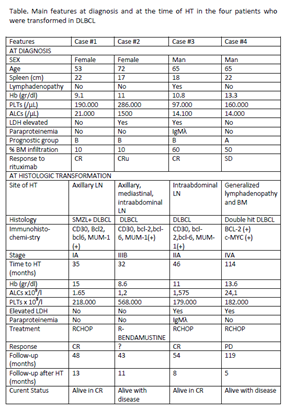
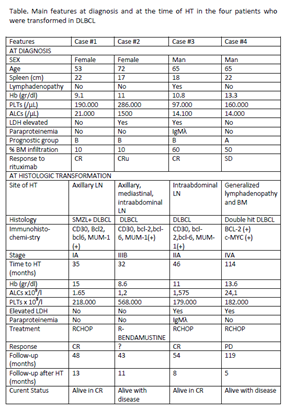
7-year PFS and OS of the whole population were 69% and 87%, respectively. After a median follow-up of ….years, HT was observed in 4(4%) patients. HT occurred at a median interval of 40 months (range: 32-114) after diagnosis. The main features at diagnosis of the patients who experienced HT are summarized in the Table. Transformation into diffuse large B cell lymphoma (DLBCL) was documented in all patients. In one of them a “double hit lymphoma” was reported due to the presence of the rearrangement of c-MYC, and BCL2. In one case a coexisting low-grade component was present in the context of the same specimen.Risk of HT was ?% at 5 and 10 years after diagnosis. At the time of HT 2 patients had high LDH and one B-symptoms. No patient had splenomegaly, while BM was infiltrated by HT in one patient (table). The site of transformation was the lymph nodes in all cases, and additionally BM in one case (the one with the double hit lymphoma). Immunohistochemistry showed positivity of CD30 in 3/4 cases. Treatment at the time of HT included RCHOP in 3 and R-Bendamustine in one case. Two patients achieved CR, one PR, while the fourth did not respond and is alive with progressive disease. At a median follow-up of 10 months (range, 5-13) after HT, 3 patients are alive, 2 in CR, 1 in PR and one with PD.
Conclusion
To our knowledge, this is one of the largest series of consecutive SMZL patients treated homogeneously with rituximab monotherapy, evaluating the incidence and risk factors for HT. HT occurred in 4% of the cases as a relatively early event during disease course. Post-transformation survival cannot be safely assessed due to short follow up after HT.
Session topic: E-poster
Keyword(s): Rituximab, Splenic marginal zone lymphoma, Transformation
Type: Publication Only
Background
SMZL is an indolent lymphoma with long survival. The risk of HT is not well defined, ranging between <5% to >20% in various reports. Rituximab has shown significant activity in the treatment of SMZL. In the rituximab era there is no study assessing the incidence of HT in SMZL patients.
Aims
To analyze the incidence and risk factors for HT in a large series of SMZL patients homogeneously treated with rituximab.
Methods
The studied cohort included 89 SMZL patients diagnosed and treated between 2003 and 2015 exclusively with rituximab monotherapy as first line treatment. 41% were males with a median age of 65 years (range, 41-95). 6/89 (7%) presented with B-symptoms and 43% with elevated LDH. According to IPI, 31% were classified as intermediate high and high risk. No patient was HCV(+). The response rate to rituximab was 95%. HT was confirmed by detailed immunomorphologic study and defined by a biopsy-proven transformation of previous SMZL into an aggressive entity. Overall survival (OS) and progression free survival (PFS) were estimated by the Kaplan-Meier method.
Results
7-year PFS and OS of the whole population were 69% and 87%, respectively. After a median follow-up of ….years, HT was observed in 4(4%) patients. HT occurred at a median interval of 40 months (range: 32-114) after diagnosis. The main features at diagnosis of the patients who experienced HT are summarized in the Table. Transformation into diffuse large B cell lymphoma (DLBCL) was documented in all patients. In one of them a “double hit lymphoma” was reported due to the presence of the rearrangement of c-MYC, and BCL2. In one case a coexisting low-grade component was present in the context of the same specimen.Risk of HT was ?% at 5 and 10 years after diagnosis. At the time of HT 2 patients had high LDH and one B-symptoms. No patient had splenomegaly, while BM was infiltrated by HT in one patient (table). The site of transformation was the lymph nodes in all cases, and additionally BM in one case (the one with the double hit lymphoma). Immunohistochemistry showed positivity of CD30 in 3/4 cases. Treatment at the time of HT included RCHOP in 3 and R-Bendamustine in one case. Two patients achieved CR, one PR, while the fourth did not respond and is alive with progressive disease. At a median follow-up of 10 months (range, 5-13) after HT, 3 patients are alive, 2 in CR, 1 in PR and one with PD.
Conclusion
To our knowledge, this is one of the largest series of consecutive SMZL patients treated homogeneously with rituximab monotherapy, evaluating the incidence and risk factors for HT. HT occurred in 4% of the cases as a relatively early event during disease course. Post-transformation survival cannot be safely assessed due to short follow up after HT.
Session topic: E-poster
Keyword(s): Rituximab, Splenic marginal zone lymphoma, Transformation
Abstract: PB1867
Type: Publication Only
Background
SMZL is an indolent lymphoma with long survival. The risk of HT is not well defined, ranging between <5% to >20% in various reports. Rituximab has shown significant activity in the treatment of SMZL. In the rituximab era there is no study assessing the incidence of HT in SMZL patients.
Aims
To analyze the incidence and risk factors for HT in a large series of SMZL patients homogeneously treated with rituximab.
Methods
The studied cohort included 89 SMZL patients diagnosed and treated between 2003 and 2015 exclusively with rituximab monotherapy as first line treatment. 41% were males with a median age of 65 years (range, 41-95). 6/89 (7%) presented with B-symptoms and 43% with elevated LDH. According to IPI, 31% were classified as intermediate high and high risk. No patient was HCV(+). The response rate to rituximab was 95%. HT was confirmed by detailed immunomorphologic study and defined by a biopsy-proven transformation of previous SMZL into an aggressive entity. Overall survival (OS) and progression free survival (PFS) were estimated by the Kaplan-Meier method.
Results
7-year PFS and OS of the whole population were 69% and 87%, respectively. After a median follow-up of ….years, HT was observed in 4(4%) patients. HT occurred at a median interval of 40 months (range: 32-114) after diagnosis. The main features at diagnosis of the patients who experienced HT are summarized in the Table. Transformation into diffuse large B cell lymphoma (DLBCL) was documented in all patients. In one of them a “double hit lymphoma” was reported due to the presence of the rearrangement of c-MYC, and BCL2. In one case a coexisting low-grade component was present in the context of the same specimen.Risk of HT was ?% at 5 and 10 years after diagnosis. At the time of HT 2 patients had high LDH and one B-symptoms. No patient had splenomegaly, while BM was infiltrated by HT in one patient (table). The site of transformation was the lymph nodes in all cases, and additionally BM in one case (the one with the double hit lymphoma). Immunohistochemistry showed positivity of CD30 in 3/4 cases. Treatment at the time of HT included RCHOP in 3 and R-Bendamustine in one case. Two patients achieved CR, one PR, while the fourth did not respond and is alive with progressive disease. At a median follow-up of 10 months (range, 5-13) after HT, 3 patients are alive, 2 in CR, 1 in PR and one with PD.
Conclusion
To our knowledge, this is one of the largest series of consecutive SMZL patients treated homogeneously with rituximab monotherapy, evaluating the incidence and risk factors for HT. HT occurred in 4% of the cases as a relatively early event during disease course. Post-transformation survival cannot be safely assessed due to short follow up after HT.
Session topic: E-poster
Keyword(s): Rituximab, Splenic marginal zone lymphoma, Transformation
Type: Publication Only
Background
SMZL is an indolent lymphoma with long survival. The risk of HT is not well defined, ranging between <5% to >20% in various reports. Rituximab has shown significant activity in the treatment of SMZL. In the rituximab era there is no study assessing the incidence of HT in SMZL patients.
Aims
To analyze the incidence and risk factors for HT in a large series of SMZL patients homogeneously treated with rituximab.
Methods
The studied cohort included 89 SMZL patients diagnosed and treated between 2003 and 2015 exclusively with rituximab monotherapy as first line treatment. 41% were males with a median age of 65 years (range, 41-95). 6/89 (7%) presented with B-symptoms and 43% with elevated LDH. According to IPI, 31% were classified as intermediate high and high risk. No patient was HCV(+). The response rate to rituximab was 95%. HT was confirmed by detailed immunomorphologic study and defined by a biopsy-proven transformation of previous SMZL into an aggressive entity. Overall survival (OS) and progression free survival (PFS) were estimated by the Kaplan-Meier method.
Results
7-year PFS and OS of the whole population were 69% and 87%, respectively. After a median follow-up of ….years, HT was observed in 4(4%) patients. HT occurred at a median interval of 40 months (range: 32-114) after diagnosis. The main features at diagnosis of the patients who experienced HT are summarized in the Table. Transformation into diffuse large B cell lymphoma (DLBCL) was documented in all patients. In one of them a “double hit lymphoma” was reported due to the presence of the rearrangement of c-MYC, and BCL2. In one case a coexisting low-grade component was present in the context of the same specimen.Risk of HT was ?% at 5 and 10 years after diagnosis. At the time of HT 2 patients had high LDH and one B-symptoms. No patient had splenomegaly, while BM was infiltrated by HT in one patient (table). The site of transformation was the lymph nodes in all cases, and additionally BM in one case (the one with the double hit lymphoma). Immunohistochemistry showed positivity of CD30 in 3/4 cases. Treatment at the time of HT included RCHOP in 3 and R-Bendamustine in one case. Two patients achieved CR, one PR, while the fourth did not respond and is alive with progressive disease. At a median follow-up of 10 months (range, 5-13) after HT, 3 patients are alive, 2 in CR, 1 in PR and one with PD.
Conclusion
To our knowledge, this is one of the largest series of consecutive SMZL patients treated homogeneously with rituximab monotherapy, evaluating the incidence and risk factors for HT. HT occurred in 4% of the cases as a relatively early event during disease course. Post-transformation survival cannot be safely assessed due to short follow up after HT.
Session topic: E-poster
Keyword(s): Rituximab, Splenic marginal zone lymphoma, Transformation
{{ help_message }}
{{filter}}


