EARLY GOOD LATER BETTER. RELATIONSHIP OF BCR-ABL LEVEL AT 12 MONTHS OF TARGET THERAPY WITH INDIVIDUAL CHARACTERISTICS OF MOLECULAR RESPONSE IN EARLY TREATMENT PERIOD IN CHRONIC MYELOID LEUKEMIA
(Abstract release date: 05/19/16)
EHA Library. Fomin A. 06/09/16; 134733; PB1833

Dr. Aleksandr Fomin
Contributions
Contributions
Abstract
Abstract: PB1833
Type: Publication Only
Background
The search of surrogate prognostic markers for early detection of high risk disease progression still is actual problem in chronic myeloid leukemia (CML) management. The existing prognostic scales consider characteristics only at moment of diagnosis, whereas individual BCR-ABL level trend remains out of its vision.
Aims
The aim of this study was to evaluate the relationship between individual characteristics of early response to treatment and BCR-ABLIS level at 12 months.
Methods
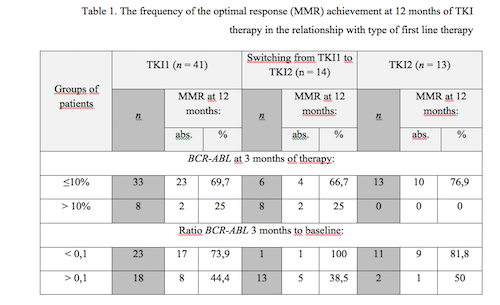
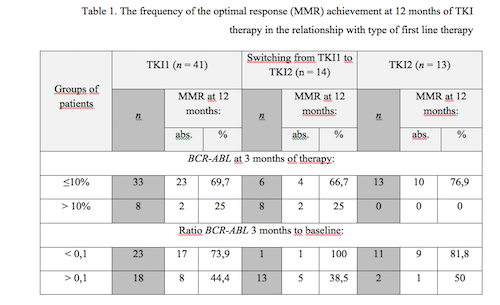
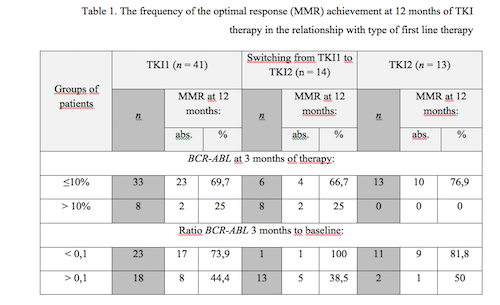
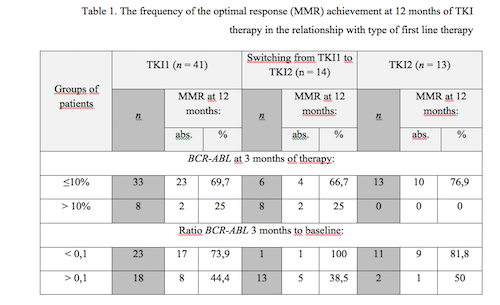
Fifty-four patients with chronic phase CML were included in the study. Forty-one patients started treatment with the first generation of tyrosine kinase inhibitors (TKI1) - Imatinib 400 mg QD. Twelve patients were treated with the second generation of tyrosine kinase inhibitors (TKI2) as first-line: Nilotinib 300 mg BID and 1 patient with Dasatinib 100 mg QD. Fourteen patients initially treated with TKI1 were subsequently switched to TKI2 (Table 1).We have conducted multivariate analysis of relationship between BCR-ABLIS levels at 12 months and early molecular response (EMR, BCR-ABLIS level ≤10% at 3 months) achievement, individual rates of BCR-ABL decline, type of first line therapy, fact of switching therapy from TKI1 to TKI2.
Results
The parameters that have statistical significance influence on BCR-ABLIS level at 12 months of therapy were as follows: individual rate of BCR-ABL decline from 3 months to baseline (<0,1/>0,1) – p=0.044, type of first-line therapy (TKI1/TKI2) – p=0.0002, switching of therapy from TKI1 to TKI2 (yes/no) – p<0.0001. Achievement of EMR did not reach statistical significance – p=0,51. In addition, we have revealed the fact, that timely switch to TKI2 for resistant CML patients led to the rates of MMR achievement at 1 year of therapy similar to the MMR rate in the remaining TKI1 treated patients, eliminating resistance to TKI1.
Conclusion
Individual characteristics of the early response to treatment, for example individual rate of BCR-ABL decline, might be used as predictors of achievement optimal treatment result in CML treatment. The adequate treatment switching from first to second generations can restore treatment efficacy in resistant patients.
Session topic: E-poster
Keyword(s): BCR-ABL, Chronic myeloid leukemia, Molecular response, Tyrosine kinase inhibitor
Type: Publication Only
Background
The search of surrogate prognostic markers for early detection of high risk disease progression still is actual problem in chronic myeloid leukemia (CML) management. The existing prognostic scales consider characteristics only at moment of diagnosis, whereas individual BCR-ABL level trend remains out of its vision.
Aims
The aim of this study was to evaluate the relationship between individual characteristics of early response to treatment and BCR-ABLIS level at 12 months.
Methods
Fifty-four patients with chronic phase CML were included in the study. Forty-one patients started treatment with the first generation of tyrosine kinase inhibitors (TKI1) - Imatinib 400 mg QD. Twelve patients were treated with the second generation of tyrosine kinase inhibitors (TKI2) as first-line: Nilotinib 300 mg BID and 1 patient with Dasatinib 100 mg QD. Fourteen patients initially treated with TKI1 were subsequently switched to TKI2 (Table 1).We have conducted multivariate analysis of relationship between BCR-ABLIS levels at 12 months and early molecular response (EMR, BCR-ABLIS level ≤10% at 3 months) achievement, individual rates of BCR-ABL decline, type of first line therapy, fact of switching therapy from TKI1 to TKI2.
Results
The parameters that have statistical significance influence on BCR-ABLIS level at 12 months of therapy were as follows: individual rate of BCR-ABL decline from 3 months to baseline (<0,1/>0,1) – p=0.044, type of first-line therapy (TKI1/TKI2) – p=0.0002, switching of therapy from TKI1 to TKI2 (yes/no) – p<0.0001. Achievement of EMR did not reach statistical significance – p=0,51. In addition, we have revealed the fact, that timely switch to TKI2 for resistant CML patients led to the rates of MMR achievement at 1 year of therapy similar to the MMR rate in the remaining TKI1 treated patients, eliminating resistance to TKI1.
Conclusion
Individual characteristics of the early response to treatment, for example individual rate of BCR-ABL decline, might be used as predictors of achievement optimal treatment result in CML treatment. The adequate treatment switching from first to second generations can restore treatment efficacy in resistant patients.
Session topic: E-poster
Keyword(s): BCR-ABL, Chronic myeloid leukemia, Molecular response, Tyrosine kinase inhibitor
Abstract: PB1833
Type: Publication Only
Background
The search of surrogate prognostic markers for early detection of high risk disease progression still is actual problem in chronic myeloid leukemia (CML) management. The existing prognostic scales consider characteristics only at moment of diagnosis, whereas individual BCR-ABL level trend remains out of its vision.
Aims
The aim of this study was to evaluate the relationship between individual characteristics of early response to treatment and BCR-ABLIS level at 12 months.
Methods
Fifty-four patients with chronic phase CML were included in the study. Forty-one patients started treatment with the first generation of tyrosine kinase inhibitors (TKI1) - Imatinib 400 mg QD. Twelve patients were treated with the second generation of tyrosine kinase inhibitors (TKI2) as first-line: Nilotinib 300 mg BID and 1 patient with Dasatinib 100 mg QD. Fourteen patients initially treated with TKI1 were subsequently switched to TKI2 (Table 1).We have conducted multivariate analysis of relationship between BCR-ABLIS levels at 12 months and early molecular response (EMR, BCR-ABLIS level ≤10% at 3 months) achievement, individual rates of BCR-ABL decline, type of first line therapy, fact of switching therapy from TKI1 to TKI2.
Results
The parameters that have statistical significance influence on BCR-ABLIS level at 12 months of therapy were as follows: individual rate of BCR-ABL decline from 3 months to baseline (<0,1/>0,1) – p=0.044, type of first-line therapy (TKI1/TKI2) – p=0.0002, switching of therapy from TKI1 to TKI2 (yes/no) – p<0.0001. Achievement of EMR did not reach statistical significance – p=0,51. In addition, we have revealed the fact, that timely switch to TKI2 for resistant CML patients led to the rates of MMR achievement at 1 year of therapy similar to the MMR rate in the remaining TKI1 treated patients, eliminating resistance to TKI1.
Conclusion
Individual characteristics of the early response to treatment, for example individual rate of BCR-ABL decline, might be used as predictors of achievement optimal treatment result in CML treatment. The adequate treatment switching from first to second generations can restore treatment efficacy in resistant patients.
Session topic: E-poster
Keyword(s): BCR-ABL, Chronic myeloid leukemia, Molecular response, Tyrosine kinase inhibitor
Type: Publication Only
Background
The search of surrogate prognostic markers for early detection of high risk disease progression still is actual problem in chronic myeloid leukemia (CML) management. The existing prognostic scales consider characteristics only at moment of diagnosis, whereas individual BCR-ABL level trend remains out of its vision.
Aims
The aim of this study was to evaluate the relationship between individual characteristics of early response to treatment and BCR-ABLIS level at 12 months.
Methods
Fifty-four patients with chronic phase CML were included in the study. Forty-one patients started treatment with the first generation of tyrosine kinase inhibitors (TKI1) - Imatinib 400 mg QD. Twelve patients were treated with the second generation of tyrosine kinase inhibitors (TKI2) as first-line: Nilotinib 300 mg BID and 1 patient with Dasatinib 100 mg QD. Fourteen patients initially treated with TKI1 were subsequently switched to TKI2 (Table 1).We have conducted multivariate analysis of relationship between BCR-ABLIS levels at 12 months and early molecular response (EMR, BCR-ABLIS level ≤10% at 3 months) achievement, individual rates of BCR-ABL decline, type of first line therapy, fact of switching therapy from TKI1 to TKI2.
Results
The parameters that have statistical significance influence on BCR-ABLIS level at 12 months of therapy were as follows: individual rate of BCR-ABL decline from 3 months to baseline (<0,1/>0,1) – p=0.044, type of first-line therapy (TKI1/TKI2) – p=0.0002, switching of therapy from TKI1 to TKI2 (yes/no) – p<0.0001. Achievement of EMR did not reach statistical significance – p=0,51. In addition, we have revealed the fact, that timely switch to TKI2 for resistant CML patients led to the rates of MMR achievement at 1 year of therapy similar to the MMR rate in the remaining TKI1 treated patients, eliminating resistance to TKI1.
Conclusion
Individual characteristics of the early response to treatment, for example individual rate of BCR-ABL decline, might be used as predictors of achievement optimal treatment result in CML treatment. The adequate treatment switching from first to second generations can restore treatment efficacy in resistant patients.
Session topic: E-poster
Keyword(s): BCR-ABL, Chronic myeloid leukemia, Molecular response, Tyrosine kinase inhibitor
{{ help_message }}
{{filter}}


