SECONDARY MALIGNANCIES IN CHRONIC LYMPHOCYTIC LEUKEMIA: A SINGLE CENTRE RETROSPECTIVE ANALYSIS
(Abstract release date: 05/19/16)
EHA Library. Reda G. 06/09/16; 134692; PB1792

Dr. Gianluigi Reda
Contributions
Contributions
Abstract
Abstract: PB1792
Type: Publication Only
Background
Chronic lymphocytic leukemia (CLL) is characterized by progressive immunodeficiency with high prevalence of infections, autoimmune phenomena and secondary malignancies. The immune deregulation may be due to the disease itself or it may be a consequence of the treatment performed.
Aims
To evaluate the occurrence of second cancers in CLL patients and their relationship with clinical and laboratory features as well as with therapy lines.
Methods
Clinical history of 514 CLL patients diagnosed and followed from 1983 until 2014 at our Institution were retrospectively evaluated and the diagnosis of a second cancer was collected. History of neoplasia preceding CLL diagnosis was also registered. Student t test for continuous variables, chi-square test for categorical ones and Log rank test for survival analysis were performed.
Results
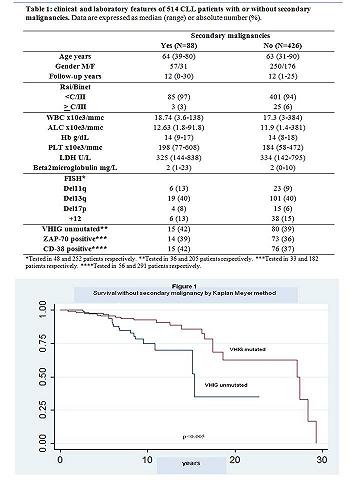
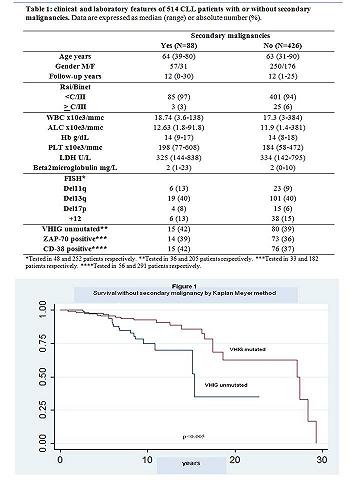
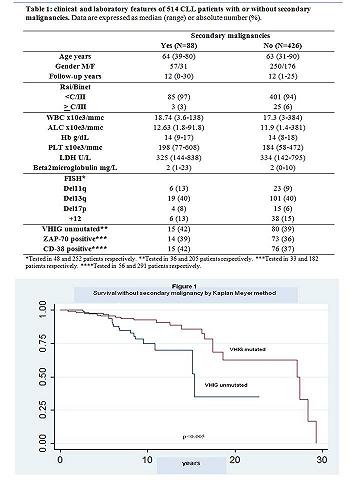
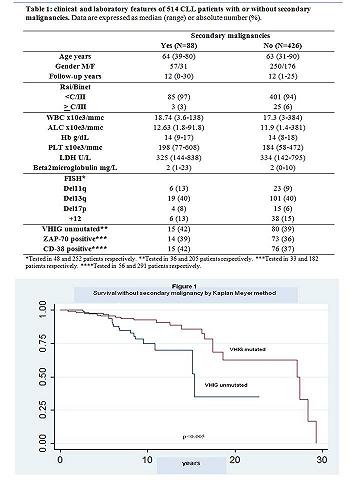
Clinical, hematological and biological characteristics are listed in Table 1. Secondary cancers were categorized according originating organ/tissue; skin cancers were divided into melanoma and non-melanoma. During the follow up 88 patients (17%) developed secondary cancers, with a mean time from diagnosis to secondary neoplasia of 9 years. Considering tumor histology, we observed 9 blood, 9 lung, 5 breast, 19 uro-genital tract (5 kidney, 10 prostate, 4 bladder, 2 uterus, and 2 ovarian), 15 gastro-enteric tract (12 colon, 2 gastric and 1 tongue), 4 pancreas, 3 melanoma and 15 skin cancers other than melanoma. No significant differences were observed according to age, gender, Rai/Binet stage and hematologic parameters in patients with or without secondary tumors (Table 1). Considering CLL prognostic features, the development of second cancers was associated with higher age (p<0.001) at diagnosis, increased beta2microglobuline levels (p=0.03) and un-mutated VHIG status (p<0.005; Figure 1). At variance, no association was found with 13q, 11q or 17p deletion, chromosome 12 trisomy, nor with ZAP-70 and CD-38 positivity (Table1). Past history was positive for malignancies in 70 patients (13%): 2 blood, 3 airways (2 lower and 1 upper), 3 breast, 6 uro-genital tract (3 bladder, 3 prostate, 2 uterus and 1 ovarian), 3 gastro-enteric tract, 3 skin cancers other than melanoma, and 3 melanoma. On the whole, 46/88 (52.3%) and 219/426 (51.4%) patients with or without secondary cancers, underwent at least one therapy line. More specifically, 86 patients were treated with fludarabine containing regimens, of whom 11 developed a secondary cancer; 180 with chlorambucil, of whom 34 developed a secondary tumor and 65 with alemtuzumab, of whom 10 were later diagnosed with a second cancer. During the follow up, 121 patients died, of whom 8 directly from secondary malignancies, 41 from CLL progression, 2 from thrombotic events, and 11 from infections.
Conclusion
Secondary malignancies are not infrequent in patients with CLL and patients with un-mutated VHIG status are at higher risk of developing a second cancer. As secondary neoplasia are not clearly related to biologic markers or to the treatment performed, a careful clinical follow up, encompassing sex and age adjusted tumors screening is advised.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Second malignancy
Type: Publication Only
Background
Chronic lymphocytic leukemia (CLL) is characterized by progressive immunodeficiency with high prevalence of infections, autoimmune phenomena and secondary malignancies. The immune deregulation may be due to the disease itself or it may be a consequence of the treatment performed.
Aims
To evaluate the occurrence of second cancers in CLL patients and their relationship with clinical and laboratory features as well as with therapy lines.
Methods
Clinical history of 514 CLL patients diagnosed and followed from 1983 until 2014 at our Institution were retrospectively evaluated and the diagnosis of a second cancer was collected. History of neoplasia preceding CLL diagnosis was also registered. Student t test for continuous variables, chi-square test for categorical ones and Log rank test for survival analysis were performed.
Results
Clinical, hematological and biological characteristics are listed in Table 1. Secondary cancers were categorized according originating organ/tissue; skin cancers were divided into melanoma and non-melanoma. During the follow up 88 patients (17%) developed secondary cancers, with a mean time from diagnosis to secondary neoplasia of 9 years. Considering tumor histology, we observed 9 blood, 9 lung, 5 breast, 19 uro-genital tract (5 kidney, 10 prostate, 4 bladder, 2 uterus, and 2 ovarian), 15 gastro-enteric tract (12 colon, 2 gastric and 1 tongue), 4 pancreas, 3 melanoma and 15 skin cancers other than melanoma. No significant differences were observed according to age, gender, Rai/Binet stage and hematologic parameters in patients with or without secondary tumors (Table 1). Considering CLL prognostic features, the development of second cancers was associated with higher age (p<0.001) at diagnosis, increased beta2microglobuline levels (p=0.03) and un-mutated VHIG status (p<0.005; Figure 1). At variance, no association was found with 13q, 11q or 17p deletion, chromosome 12 trisomy, nor with ZAP-70 and CD-38 positivity (Table1). Past history was positive for malignancies in 70 patients (13%): 2 blood, 3 airways (2 lower and 1 upper), 3 breast, 6 uro-genital tract (3 bladder, 3 prostate, 2 uterus and 1 ovarian), 3 gastro-enteric tract, 3 skin cancers other than melanoma, and 3 melanoma. On the whole, 46/88 (52.3%) and 219/426 (51.4%) patients with or without secondary cancers, underwent at least one therapy line. More specifically, 86 patients were treated with fludarabine containing regimens, of whom 11 developed a secondary cancer; 180 with chlorambucil, of whom 34 developed a secondary tumor and 65 with alemtuzumab, of whom 10 were later diagnosed with a second cancer. During the follow up, 121 patients died, of whom 8 directly from secondary malignancies, 41 from CLL progression, 2 from thrombotic events, and 11 from infections.
Conclusion
Secondary malignancies are not infrequent in patients with CLL and patients with un-mutated VHIG status are at higher risk of developing a second cancer. As secondary neoplasia are not clearly related to biologic markers or to the treatment performed, a careful clinical follow up, encompassing sex and age adjusted tumors screening is advised.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Second malignancy
Abstract: PB1792
Type: Publication Only
Background
Chronic lymphocytic leukemia (CLL) is characterized by progressive immunodeficiency with high prevalence of infections, autoimmune phenomena and secondary malignancies. The immune deregulation may be due to the disease itself or it may be a consequence of the treatment performed.
Aims
To evaluate the occurrence of second cancers in CLL patients and their relationship with clinical and laboratory features as well as with therapy lines.
Methods
Clinical history of 514 CLL patients diagnosed and followed from 1983 until 2014 at our Institution were retrospectively evaluated and the diagnosis of a second cancer was collected. History of neoplasia preceding CLL diagnosis was also registered. Student t test for continuous variables, chi-square test for categorical ones and Log rank test for survival analysis were performed.
Results
Clinical, hematological and biological characteristics are listed in Table 1. Secondary cancers were categorized according originating organ/tissue; skin cancers were divided into melanoma and non-melanoma. During the follow up 88 patients (17%) developed secondary cancers, with a mean time from diagnosis to secondary neoplasia of 9 years. Considering tumor histology, we observed 9 blood, 9 lung, 5 breast, 19 uro-genital tract (5 kidney, 10 prostate, 4 bladder, 2 uterus, and 2 ovarian), 15 gastro-enteric tract (12 colon, 2 gastric and 1 tongue), 4 pancreas, 3 melanoma and 15 skin cancers other than melanoma. No significant differences were observed according to age, gender, Rai/Binet stage and hematologic parameters in patients with or without secondary tumors (Table 1). Considering CLL prognostic features, the development of second cancers was associated with higher age (p<0.001) at diagnosis, increased beta2microglobuline levels (p=0.03) and un-mutated VHIG status (p<0.005; Figure 1). At variance, no association was found with 13q, 11q or 17p deletion, chromosome 12 trisomy, nor with ZAP-70 and CD-38 positivity (Table1). Past history was positive for malignancies in 70 patients (13%): 2 blood, 3 airways (2 lower and 1 upper), 3 breast, 6 uro-genital tract (3 bladder, 3 prostate, 2 uterus and 1 ovarian), 3 gastro-enteric tract, 3 skin cancers other than melanoma, and 3 melanoma. On the whole, 46/88 (52.3%) and 219/426 (51.4%) patients with or without secondary cancers, underwent at least one therapy line. More specifically, 86 patients were treated with fludarabine containing regimens, of whom 11 developed a secondary cancer; 180 with chlorambucil, of whom 34 developed a secondary tumor and 65 with alemtuzumab, of whom 10 were later diagnosed with a second cancer. During the follow up, 121 patients died, of whom 8 directly from secondary malignancies, 41 from CLL progression, 2 from thrombotic events, and 11 from infections.
Conclusion
Secondary malignancies are not infrequent in patients with CLL and patients with un-mutated VHIG status are at higher risk of developing a second cancer. As secondary neoplasia are not clearly related to biologic markers or to the treatment performed, a careful clinical follow up, encompassing sex and age adjusted tumors screening is advised.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Second malignancy
Type: Publication Only
Background
Chronic lymphocytic leukemia (CLL) is characterized by progressive immunodeficiency with high prevalence of infections, autoimmune phenomena and secondary malignancies. The immune deregulation may be due to the disease itself or it may be a consequence of the treatment performed.
Aims
To evaluate the occurrence of second cancers in CLL patients and their relationship with clinical and laboratory features as well as with therapy lines.
Methods
Clinical history of 514 CLL patients diagnosed and followed from 1983 until 2014 at our Institution were retrospectively evaluated and the diagnosis of a second cancer was collected. History of neoplasia preceding CLL diagnosis was also registered. Student t test for continuous variables, chi-square test for categorical ones and Log rank test for survival analysis were performed.
Results
Clinical, hematological and biological characteristics are listed in Table 1. Secondary cancers were categorized according originating organ/tissue; skin cancers were divided into melanoma and non-melanoma. During the follow up 88 patients (17%) developed secondary cancers, with a mean time from diagnosis to secondary neoplasia of 9 years. Considering tumor histology, we observed 9 blood, 9 lung, 5 breast, 19 uro-genital tract (5 kidney, 10 prostate, 4 bladder, 2 uterus, and 2 ovarian), 15 gastro-enteric tract (12 colon, 2 gastric and 1 tongue), 4 pancreas, 3 melanoma and 15 skin cancers other than melanoma. No significant differences were observed according to age, gender, Rai/Binet stage and hematologic parameters in patients with or without secondary tumors (Table 1). Considering CLL prognostic features, the development of second cancers was associated with higher age (p<0.001) at diagnosis, increased beta2microglobuline levels (p=0.03) and un-mutated VHIG status (p<0.005; Figure 1). At variance, no association was found with 13q, 11q or 17p deletion, chromosome 12 trisomy, nor with ZAP-70 and CD-38 positivity (Table1). Past history was positive for malignancies in 70 patients (13%): 2 blood, 3 airways (2 lower and 1 upper), 3 breast, 6 uro-genital tract (3 bladder, 3 prostate, 2 uterus and 1 ovarian), 3 gastro-enteric tract, 3 skin cancers other than melanoma, and 3 melanoma. On the whole, 46/88 (52.3%) and 219/426 (51.4%) patients with or without secondary cancers, underwent at least one therapy line. More specifically, 86 patients were treated with fludarabine containing regimens, of whom 11 developed a secondary cancer; 180 with chlorambucil, of whom 34 developed a secondary tumor and 65 with alemtuzumab, of whom 10 were later diagnosed with a second cancer. During the follow up, 121 patients died, of whom 8 directly from secondary malignancies, 41 from CLL progression, 2 from thrombotic events, and 11 from infections.
Conclusion
Secondary malignancies are not infrequent in patients with CLL and patients with un-mutated VHIG status are at higher risk of developing a second cancer. As secondary neoplasia are not clearly related to biologic markers or to the treatment performed, a careful clinical follow up, encompassing sex and age adjusted tumors screening is advised.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Second malignancy
{{ help_message }}
{{filter}}


