A NEW PROGNOSTIC SCORING SYSTEM FOR TTFT FOR PATIENTS WITH CLL IN CHINA
(Abstract release date: 05/19/16)
EHA Library. Lim L. 06/09/16; 134689; PB1789

Lay-Cheng Lim
Contributions
Contributions
Abstract
Abstract: PB1789
Type: Publication Only
Background
The established clinical staging systems (Rai/Binet) can not accurately discriminate among prognostic groups, especially for patients in early stages. Several prognostic factors have been identified to predict the outcome of patients with chronic lymphocytic leukemia (CLL), but only a few studies analyzed more markers together.
Aims
In this study, we identified the biologic prognostic markers and combined them in a new prognostic scoring system, the CLL prognostic index (CLL-PI) for predicting time to first treatment (TTFT) in patients with CLL in China.
Methods
Taking advantage of a population of 402 untreated Chinese patients with CLL at early and advanced stage of disease, we identified the strongest prognostic markers of TTFT and, subsequently, in a cohort of 173 patients we integrated data of traditional staging system, cytogenetic lesions and immunoglobulin heavy chain variable region (IGHV) mutational status in CLL-PI. The median follow-up time was 45 months (ms). Methods of multivariable statistics were applied, and the end point was TTFT.
Results
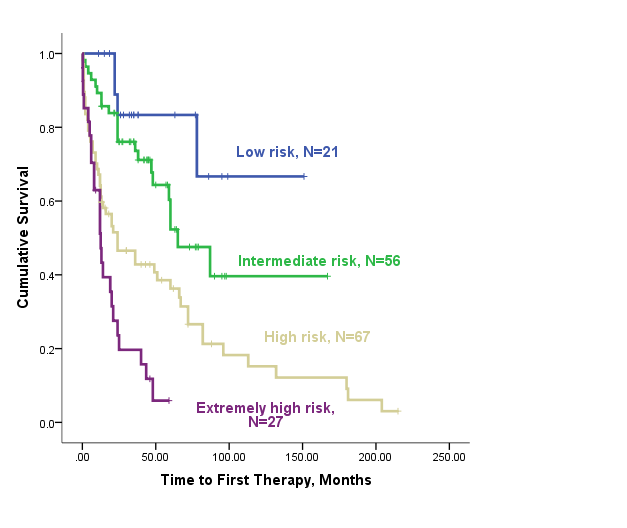
Based on multivariate Cox regression analysis, three independent factors for TTFT were identified: clinical stage (Rai risk group), del17p and IGHV mutation status. Applying weighted grading of these three independent factors based on regression parameters, a CLL-PI was constructed, which could categorize four different risk groups [low (score 1), intermediate (score 2), high (score 3) and extremely high risk (score 4-6)] with significantly different TTFT (median TTFT of NR, 65.0 ms, 24.0 ms and 12.5 ms, respectively, p<0.001). Further, this index provided accurate estimation regarding overall survival (OS) (median OS of NR, 210.0 ms, 97.0 ms and 43.0 ms, respectively, p<0.001].Table 1 Scores assignment to three independent factors of PI
Abbreviation: IGHV, mutated immunoglobulin heavy chain variable region; M, mutated; U, unmutated.Table 2. Survival data in each subgroup according to the scoring system
Abbreviation: CI, confidence interval; TTFT, time to first therapy; NR, not reached; NE, not evaluated.
Conclusion
This study developed a weighted, integrated CLL-PI which combines the most important genetic prognostic markers (IGHV mutation status, 17p deletion) with traditional clinical stage. This newly modified PI could be used to discriminate among groups and may help predict the TTFT and prognosis of patients with CLL.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia
Type: Publication Only
Background
The established clinical staging systems (Rai/Binet) can not accurately discriminate among prognostic groups, especially for patients in early stages. Several prognostic factors have been identified to predict the outcome of patients with chronic lymphocytic leukemia (CLL), but only a few studies analyzed more markers together.
Aims
In this study, we identified the biologic prognostic markers and combined them in a new prognostic scoring system, the CLL prognostic index (CLL-PI) for predicting time to first treatment (TTFT) in patients with CLL in China.
Methods
Taking advantage of a population of 402 untreated Chinese patients with CLL at early and advanced stage of disease, we identified the strongest prognostic markers of TTFT and, subsequently, in a cohort of 173 patients we integrated data of traditional staging system, cytogenetic lesions and immunoglobulin heavy chain variable region (IGHV) mutational status in CLL-PI. The median follow-up time was 45 months (ms). Methods of multivariable statistics were applied, and the end point was TTFT.
Results
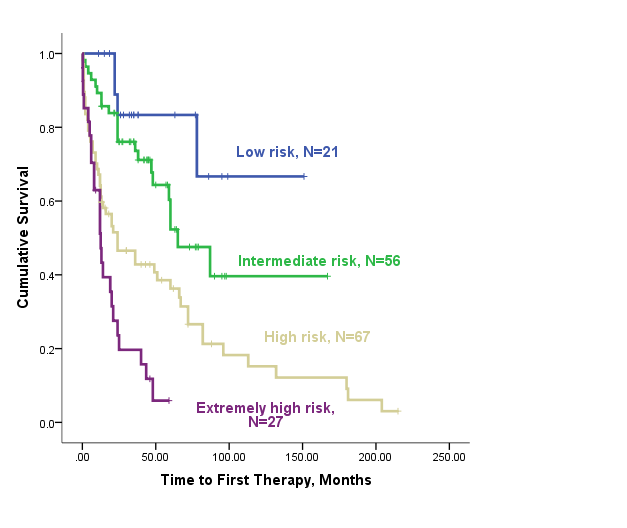
Based on multivariate Cox regression analysis, three independent factors for TTFT were identified: clinical stage (Rai risk group), del17p and IGHV mutation status. Applying weighted grading of these three independent factors based on regression parameters, a CLL-PI was constructed, which could categorize four different risk groups [low (score 1), intermediate (score 2), high (score 3) and extremely high risk (score 4-6)] with significantly different TTFT (median TTFT of NR, 65.0 ms, 24.0 ms and 12.5 ms, respectively, p<0.001). Further, this index provided accurate estimation regarding overall survival (OS) (median OS of NR, 210.0 ms, 97.0 ms and 43.0 ms, respectively, p<0.001].Table 1 Scores assignment to three independent factors of PI
| Rai risk group | Scores | IGHV status | Scores | 17p- | Scores |
| Low (Rai 0) | 1 | M-IGHV | 0 | Negative | 0 |
| Intermediate (Rai I-II) | 2 | U-IGHV | 1 | Positive | 2 |
| High (Rai III-IV) | 3 |
| Groups (PI scores) | N | Median TTFT(months) | 95% CI (months) | p-value |
| Low risk (=1) | 21 | NR | NE-NE | 0.000 |
| Intermediate risk (=2) | 56 | 65.0 | 40.9-89.1 | |
| High risk (=3) | 67 | 24.0 | 6.2-41.8 | |
| Extremely high risk (4-6) | 27 | 12.5 | 7.6-17.4 |
Conclusion
This study developed a weighted, integrated CLL-PI which combines the most important genetic prognostic markers (IGHV mutation status, 17p deletion) with traditional clinical stage. This newly modified PI could be used to discriminate among groups and may help predict the TTFT and prognosis of patients with CLL.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia
Abstract: PB1789
Type: Publication Only
Background
The established clinical staging systems (Rai/Binet) can not accurately discriminate among prognostic groups, especially for patients in early stages. Several prognostic factors have been identified to predict the outcome of patients with chronic lymphocytic leukemia (CLL), but only a few studies analyzed more markers together.
Aims
In this study, we identified the biologic prognostic markers and combined them in a new prognostic scoring system, the CLL prognostic index (CLL-PI) for predicting time to first treatment (TTFT) in patients with CLL in China.
Methods
Taking advantage of a population of 402 untreated Chinese patients with CLL at early and advanced stage of disease, we identified the strongest prognostic markers of TTFT and, subsequently, in a cohort of 173 patients we integrated data of traditional staging system, cytogenetic lesions and immunoglobulin heavy chain variable region (IGHV) mutational status in CLL-PI. The median follow-up time was 45 months (ms). Methods of multivariable statistics were applied, and the end point was TTFT.
Results
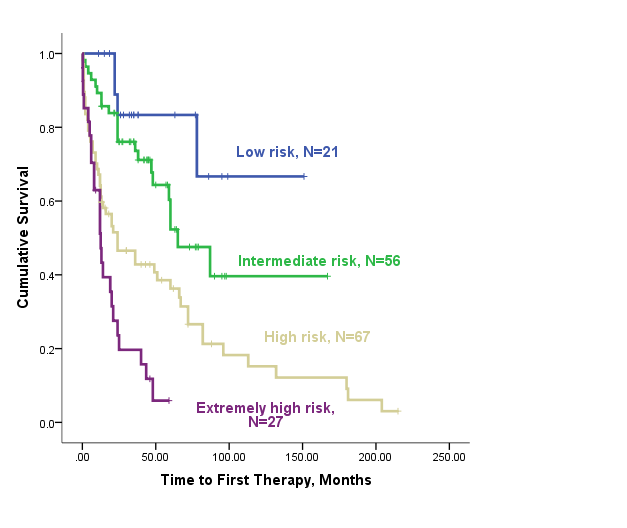
Based on multivariate Cox regression analysis, three independent factors for TTFT were identified: clinical stage (Rai risk group), del17p and IGHV mutation status. Applying weighted grading of these three independent factors based on regression parameters, a CLL-PI was constructed, which could categorize four different risk groups [low (score 1), intermediate (score 2), high (score 3) and extremely high risk (score 4-6)] with significantly different TTFT (median TTFT of NR, 65.0 ms, 24.0 ms and 12.5 ms, respectively, p<0.001). Further, this index provided accurate estimation regarding overall survival (OS) (median OS of NR, 210.0 ms, 97.0 ms and 43.0 ms, respectively, p<0.001].Table 1 Scores assignment to three independent factors of PI
Abbreviation: IGHV, mutated immunoglobulin heavy chain variable region; M, mutated; U, unmutated.Table 2. Survival data in each subgroup according to the scoring system
Abbreviation: CI, confidence interval; TTFT, time to first therapy; NR, not reached; NE, not evaluated.
Conclusion
This study developed a weighted, integrated CLL-PI which combines the most important genetic prognostic markers (IGHV mutation status, 17p deletion) with traditional clinical stage. This newly modified PI could be used to discriminate among groups and may help predict the TTFT and prognosis of patients with CLL.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia
Type: Publication Only
Background
The established clinical staging systems (Rai/Binet) can not accurately discriminate among prognostic groups, especially for patients in early stages. Several prognostic factors have been identified to predict the outcome of patients with chronic lymphocytic leukemia (CLL), but only a few studies analyzed more markers together.
Aims
In this study, we identified the biologic prognostic markers and combined them in a new prognostic scoring system, the CLL prognostic index (CLL-PI) for predicting time to first treatment (TTFT) in patients with CLL in China.
Methods
Taking advantage of a population of 402 untreated Chinese patients with CLL at early and advanced stage of disease, we identified the strongest prognostic markers of TTFT and, subsequently, in a cohort of 173 patients we integrated data of traditional staging system, cytogenetic lesions and immunoglobulin heavy chain variable region (IGHV) mutational status in CLL-PI. The median follow-up time was 45 months (ms). Methods of multivariable statistics were applied, and the end point was TTFT.
Results
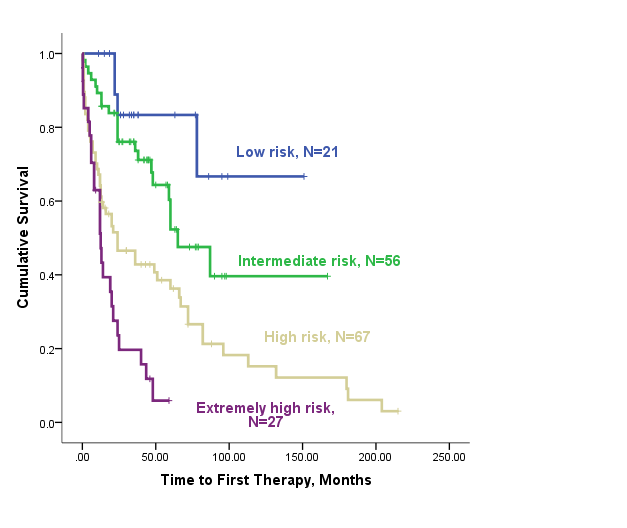
Based on multivariate Cox regression analysis, three independent factors for TTFT were identified: clinical stage (Rai risk group), del17p and IGHV mutation status. Applying weighted grading of these three independent factors based on regression parameters, a CLL-PI was constructed, which could categorize four different risk groups [low (score 1), intermediate (score 2), high (score 3) and extremely high risk (score 4-6)] with significantly different TTFT (median TTFT of NR, 65.0 ms, 24.0 ms and 12.5 ms, respectively, p<0.001). Further, this index provided accurate estimation regarding overall survival (OS) (median OS of NR, 210.0 ms, 97.0 ms and 43.0 ms, respectively, p<0.001].Table 1 Scores assignment to three independent factors of PI
| Rai risk group | Scores | IGHV status | Scores | 17p- | Scores |
| Low (Rai 0) | 1 | M-IGHV | 0 | Negative | 0 |
| Intermediate (Rai I-II) | 2 | U-IGHV | 1 | Positive | 2 |
| High (Rai III-IV) | 3 |
| Groups (PI scores) | N | Median TTFT(months) | 95% CI (months) | p-value |
| Low risk (=1) | 21 | NR | NE-NE | 0.000 |
| Intermediate risk (=2) | 56 | 65.0 | 40.9-89.1 | |
| High risk (=3) | 67 | 24.0 | 6.2-41.8 | |
| Extremely high risk (4-6) | 27 | 12.5 | 7.6-17.4 |
Conclusion
This study developed a weighted, integrated CLL-PI which combines the most important genetic prognostic markers (IGHV mutation status, 17p deletion) with traditional clinical stage. This newly modified PI could be used to discriminate among groups and may help predict the TTFT and prognosis of patients with CLL.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia
{{ help_message }}
{{filter}}


