VON WILLEBRAND DISEASE AND ACQUIRED VON WILLEBRAND SYNDROME - A DIAGNOSTIC ALGORITHM
(Abstract release date: 05/19/16)
EHA Library. Campos M. 06/09/16; 134654; PB1754

Dr. Maria Manuel Campos
Contributions
Contributions
Abstract
Abstract: PB1754
Type: Publication Only
Background
Von Willebrand disease (VWD) is a common inherited bleeding disorder (prevalence of 1:10000) but acquired von Willebrand syndrome (AVWS) is a very rare bleeding state associated with lymphoproliferative, myeloproliferative, cardiovascular and autoimmune conditions, hypothyroidism, uremia, liver cirrhosis, pancreatitis and the use of ciprofloxacin, griseofulvin, valproic acid and tetracycline. More than 60% of the few reported cases of AVWS correspond to lymphoma, multiple myeloma, monoclonal gammopathy of undetermined significance, essential thrombocythemia, polycythemia vera, chronic myeloid leukemia and primary myelofibrosis.
Aims
To establish a diagnostic algorithm for VWD and AWVS, differential diagnosis must be done including other coagulopathies. Factor VIII:C (FVIII:C) and von Willebrand factor (VWF) are endothelium injury markers and their levels may increase in inflammatory diseases. Individuals with blood group O exhibit lower levels of VWF but there is a general raise of VWF with ageing.
Methods
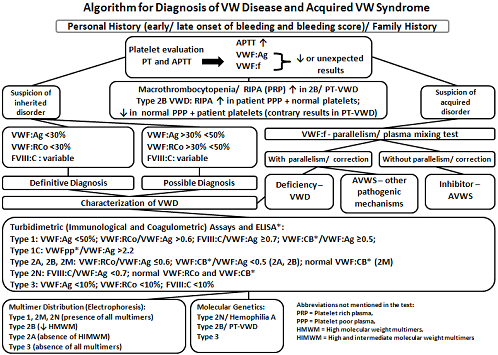
The prothrombin time (PT) and the activated partial thromboplastin time (APTT) are not reliable tests in screening for diagnosis of VWD. Optional tests as thrombin time or fibrinogen are not relevant. So, a basic approach with PT, APTT, and an evaluation of platelet count, morphology and function, must be followed by WVF-specific tests, like a profile with VWF antigen (VWF:Ag), functional VWF (VWF:f) that corresponds to VWF activity (VWF:Act) or VWF ristocetin cofactor (VWF:RCo) and FVIII:C. For inhibitor screening the VWF:f is carried out with several dilutions of patient plasma with factor diluent (the parallelism loss suggests an inhibitor, which can be present in AWVS). Another procedure is the plasma mixing test with patient plasma and normal plasma. Low-dose ristocetin-induced platelet aggregation (RIPA), multimer analysis by agarose gel electrophoresis, molecular genetics, VWF binding to collagen (VWF:CB) and VWF propeptide (VWFpp) by enzyme-linked immunosorbent assay (ELISA) are other resources for specialized laboratories.
Results
The diagnostic algorithm (figure) summarizes our methodology. The table shows our laboratory results of different types of VWD, AVWS and low VWF.Table - Laboratory results of different types of VWD, AVWS and low VWF (levels in %)
Conclusion
1) We propose an algorithm for the diagnostic approach of mucocutaneous bleeding with high clinical suspicion of VWD, platelet type pseudo-VWD (PT-VWD) and AVWS. 2) The main goal is to create a multistep screening based in threshold values. 3) The differentiation between type 2B VWD and PT-VWD is essential to avoid misdiagnoses and provide adequate therapy. 4) The clarification between type 1 VWD and low level of VWF:Ag and/or VWF:RCo (30-50%) is controversial: asymptomatic individuals don’t need an extensive testing, only those with a past severe hemorrhages (a good predictor of recurrence) or presenting relatives with similar levels require an advanced assessment. 5) If VWFpp is available it may be helpful in the identification of type 1C VWD.
Session topic: E-poster
Keyword(s): Acquired von Willebrand syndrome, Diagnosis, Von Willebrand factor (vWF), Von Willebrand's disease
Type: Publication Only
Background
Von Willebrand disease (VWD) is a common inherited bleeding disorder (prevalence of 1:10000) but acquired von Willebrand syndrome (AVWS) is a very rare bleeding state associated with lymphoproliferative, myeloproliferative, cardiovascular and autoimmune conditions, hypothyroidism, uremia, liver cirrhosis, pancreatitis and the use of ciprofloxacin, griseofulvin, valproic acid and tetracycline. More than 60% of the few reported cases of AVWS correspond to lymphoma, multiple myeloma, monoclonal gammopathy of undetermined significance, essential thrombocythemia, polycythemia vera, chronic myeloid leukemia and primary myelofibrosis.
Aims
To establish a diagnostic algorithm for VWD and AWVS, differential diagnosis must be done including other coagulopathies. Factor VIII:C (FVIII:C) and von Willebrand factor (VWF) are endothelium injury markers and their levels may increase in inflammatory diseases. Individuals with blood group O exhibit lower levels of VWF but there is a general raise of VWF with ageing.
Methods
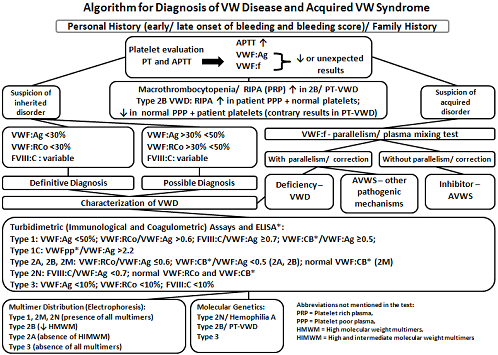
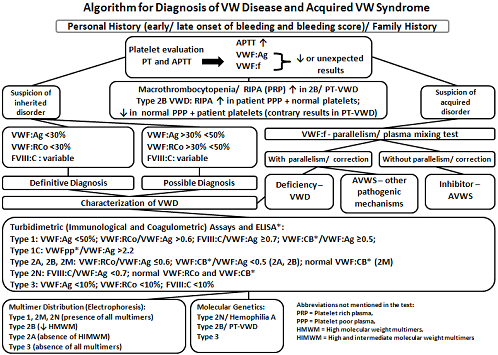
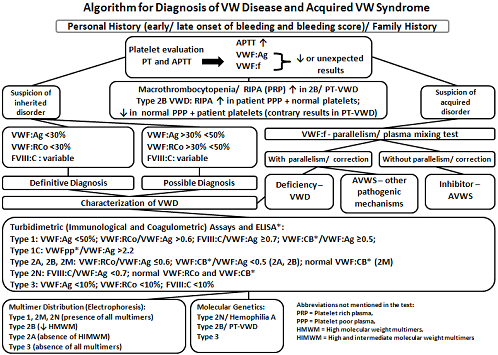
The prothrombin time (PT) and the activated partial thromboplastin time (APTT) are not reliable tests in screening for diagnosis of VWD. Optional tests as thrombin time or fibrinogen are not relevant. So, a basic approach with PT, APTT, and an evaluation of platelet count, morphology and function, must be followed by WVF-specific tests, like a profile with VWF antigen (VWF:Ag), functional VWF (VWF:f) that corresponds to VWF activity (VWF:Act) or VWF ristocetin cofactor (VWF:RCo) and FVIII:C. For inhibitor screening the VWF:f is carried out with several dilutions of patient plasma with factor diluent (the parallelism loss suggests an inhibitor, which can be present in AWVS). Another procedure is the plasma mixing test with patient plasma and normal plasma. Low-dose ristocetin-induced platelet aggregation (RIPA), multimer analysis by agarose gel electrophoresis, molecular genetics, VWF binding to collagen (VWF:CB) and VWF propeptide (VWFpp) by enzyme-linked immunosorbent assay (ELISA) are other resources for specialized laboratories.
Results
The diagnostic algorithm (figure) summarizes our methodology. The table shows our laboratory results of different types of VWD, AVWS and low VWF.Table - Laboratory results of different types of VWD, AVWS and low VWF (levels in %)
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | |
| VWF:Ag | 35.0 | 34.0 | 30.2 | 9.0 | 49.1 | 53.4 | 13.4 |
| VWF:RCo | 33.0 | 8.0 | <7.0 (4.8) | - | 45.4 | 39.1 | 8.2 |
| VWF:Act | 36.0 | <19.0 (10.0) | - | <19.0 (1.0) | 40.9 | - | <19.0 (3.2) |
| FVIII:C | 64.0 | 53.0 | 37.7 | 4.0 | 54.8 | 53.5 | 18.1 |
| VWF:CB | 27.2 | 8.1 | - | 8.1 | - | - | - |
| RIPA | - | ↓ | - | Absent | - | - | - |
| Multimers | Normal | ↓ HIMWM | - | All absent | - | - | - |
| Genetics (mutations) | - | - | R1374H | - | - | - | - |
| VWF:f parallelism | - | - | - | - | - | - | Inhibitor |
| Defects | Type 1 | Type 2A | Type 2M | Type 3 | Low VWF | Low VWF | AWVS |
| Gender (M/F) | F | F | M | F | F | M | F |
| Age (years) | 42 | 33 | 34 | 34 | 35 | 18 | 74 |
Conclusion
1) We propose an algorithm for the diagnostic approach of mucocutaneous bleeding with high clinical suspicion of VWD, platelet type pseudo-VWD (PT-VWD) and AVWS. 2) The main goal is to create a multistep screening based in threshold values. 3) The differentiation between type 2B VWD and PT-VWD is essential to avoid misdiagnoses and provide adequate therapy. 4) The clarification between type 1 VWD and low level of VWF:Ag and/or VWF:RCo (30-50%) is controversial: asymptomatic individuals don’t need an extensive testing, only those with a past severe hemorrhages (a good predictor of recurrence) or presenting relatives with similar levels require an advanced assessment. 5) If VWFpp is available it may be helpful in the identification of type 1C VWD.
Session topic: E-poster
Keyword(s): Acquired von Willebrand syndrome, Diagnosis, Von Willebrand factor (vWF), Von Willebrand's disease
Abstract: PB1754
Type: Publication Only
Background
Von Willebrand disease (VWD) is a common inherited bleeding disorder (prevalence of 1:10000) but acquired von Willebrand syndrome (AVWS) is a very rare bleeding state associated with lymphoproliferative, myeloproliferative, cardiovascular and autoimmune conditions, hypothyroidism, uremia, liver cirrhosis, pancreatitis and the use of ciprofloxacin, griseofulvin, valproic acid and tetracycline. More than 60% of the few reported cases of AVWS correspond to lymphoma, multiple myeloma, monoclonal gammopathy of undetermined significance, essential thrombocythemia, polycythemia vera, chronic myeloid leukemia and primary myelofibrosis.
Aims
To establish a diagnostic algorithm for VWD and AWVS, differential diagnosis must be done including other coagulopathies. Factor VIII:C (FVIII:C) and von Willebrand factor (VWF) are endothelium injury markers and their levels may increase in inflammatory diseases. Individuals with blood group O exhibit lower levels of VWF but there is a general raise of VWF with ageing.
Methods
The prothrombin time (PT) and the activated partial thromboplastin time (APTT) are not reliable tests in screening for diagnosis of VWD. Optional tests as thrombin time or fibrinogen are not relevant. So, a basic approach with PT, APTT, and an evaluation of platelet count, morphology and function, must be followed by WVF-specific tests, like a profile with VWF antigen (VWF:Ag), functional VWF (VWF:f) that corresponds to VWF activity (VWF:Act) or VWF ristocetin cofactor (VWF:RCo) and FVIII:C. For inhibitor screening the VWF:f is carried out with several dilutions of patient plasma with factor diluent (the parallelism loss suggests an inhibitor, which can be present in AWVS). Another procedure is the plasma mixing test with patient plasma and normal plasma. Low-dose ristocetin-induced platelet aggregation (RIPA), multimer analysis by agarose gel electrophoresis, molecular genetics, VWF binding to collagen (VWF:CB) and VWF propeptide (VWFpp) by enzyme-linked immunosorbent assay (ELISA) are other resources for specialized laboratories.
Results
The diagnostic algorithm (figure) summarizes our methodology. The table shows our laboratory results of different types of VWD, AVWS and low VWF.Table - Laboratory results of different types of VWD, AVWS and low VWF (levels in %)
Conclusion
1) We propose an algorithm for the diagnostic approach of mucocutaneous bleeding with high clinical suspicion of VWD, platelet type pseudo-VWD (PT-VWD) and AVWS. 2) The main goal is to create a multistep screening based in threshold values. 3) The differentiation between type 2B VWD and PT-VWD is essential to avoid misdiagnoses and provide adequate therapy. 4) The clarification between type 1 VWD and low level of VWF:Ag and/or VWF:RCo (30-50%) is controversial: asymptomatic individuals don’t need an extensive testing, only those with a past severe hemorrhages (a good predictor of recurrence) or presenting relatives with similar levels require an advanced assessment. 5) If VWFpp is available it may be helpful in the identification of type 1C VWD.
Session topic: E-poster
Keyword(s): Acquired von Willebrand syndrome, Diagnosis, Von Willebrand factor (vWF), Von Willebrand's disease
Type: Publication Only
Background
Von Willebrand disease (VWD) is a common inherited bleeding disorder (prevalence of 1:10000) but acquired von Willebrand syndrome (AVWS) is a very rare bleeding state associated with lymphoproliferative, myeloproliferative, cardiovascular and autoimmune conditions, hypothyroidism, uremia, liver cirrhosis, pancreatitis and the use of ciprofloxacin, griseofulvin, valproic acid and tetracycline. More than 60% of the few reported cases of AVWS correspond to lymphoma, multiple myeloma, monoclonal gammopathy of undetermined significance, essential thrombocythemia, polycythemia vera, chronic myeloid leukemia and primary myelofibrosis.
Aims
To establish a diagnostic algorithm for VWD and AWVS, differential diagnosis must be done including other coagulopathies. Factor VIII:C (FVIII:C) and von Willebrand factor (VWF) are endothelium injury markers and their levels may increase in inflammatory diseases. Individuals with blood group O exhibit lower levels of VWF but there is a general raise of VWF with ageing.
Methods
The prothrombin time (PT) and the activated partial thromboplastin time (APTT) are not reliable tests in screening for diagnosis of VWD. Optional tests as thrombin time or fibrinogen are not relevant. So, a basic approach with PT, APTT, and an evaluation of platelet count, morphology and function, must be followed by WVF-specific tests, like a profile with VWF antigen (VWF:Ag), functional VWF (VWF:f) that corresponds to VWF activity (VWF:Act) or VWF ristocetin cofactor (VWF:RCo) and FVIII:C. For inhibitor screening the VWF:f is carried out with several dilutions of patient plasma with factor diluent (the parallelism loss suggests an inhibitor, which can be present in AWVS). Another procedure is the plasma mixing test with patient plasma and normal plasma. Low-dose ristocetin-induced platelet aggregation (RIPA), multimer analysis by agarose gel electrophoresis, molecular genetics, VWF binding to collagen (VWF:CB) and VWF propeptide (VWFpp) by enzyme-linked immunosorbent assay (ELISA) are other resources for specialized laboratories.
Results
The diagnostic algorithm (figure) summarizes our methodology. The table shows our laboratory results of different types of VWD, AVWS and low VWF.Table - Laboratory results of different types of VWD, AVWS and low VWF (levels in %)
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | |
| VWF:Ag | 35.0 | 34.0 | 30.2 | 9.0 | 49.1 | 53.4 | 13.4 |
| VWF:RCo | 33.0 | 8.0 | <7.0 (4.8) | - | 45.4 | 39.1 | 8.2 |
| VWF:Act | 36.0 | <19.0 (10.0) | - | <19.0 (1.0) | 40.9 | - | <19.0 (3.2) |
| FVIII:C | 64.0 | 53.0 | 37.7 | 4.0 | 54.8 | 53.5 | 18.1 |
| VWF:CB | 27.2 | 8.1 | - | 8.1 | - | - | - |
| RIPA | - | ↓ | - | Absent | - | - | - |
| Multimers | Normal | ↓ HIMWM | - | All absent | - | - | - |
| Genetics (mutations) | - | - | R1374H | - | - | - | - |
| VWF:f parallelism | - | - | - | - | - | - | Inhibitor |
| Defects | Type 1 | Type 2A | Type 2M | Type 3 | Low VWF | Low VWF | AWVS |
| Gender (M/F) | F | F | M | F | F | M | F |
| Age (years) | 42 | 33 | 34 | 34 | 35 | 18 | 74 |
Conclusion
1) We propose an algorithm for the diagnostic approach of mucocutaneous bleeding with high clinical suspicion of VWD, platelet type pseudo-VWD (PT-VWD) and AVWS. 2) The main goal is to create a multistep screening based in threshold values. 3) The differentiation between type 2B VWD and PT-VWD is essential to avoid misdiagnoses and provide adequate therapy. 4) The clarification between type 1 VWD and low level of VWF:Ag and/or VWF:RCo (30-50%) is controversial: asymptomatic individuals don’t need an extensive testing, only those with a past severe hemorrhages (a good predictor of recurrence) or presenting relatives with similar levels require an advanced assessment. 5) If VWFpp is available it may be helpful in the identification of type 1C VWD.
Session topic: E-poster
Keyword(s): Acquired von Willebrand syndrome, Diagnosis, Von Willebrand factor (vWF), Von Willebrand's disease
{{ help_message }}
{{filter}}


