OUTCOME AND PROGNOSTIC FACTORS IN DIFFUSE LARGE B-CELL LYMPHOMA: AN INSTITUTIONAL EXPERIENCE OF A TERTIARY CARE CENTRE FROM INDIA
(Abstract release date: 05/19/16)
EHA Library. Mahajan R. 06/09/16; 134640; PB1740

Dr. Rohit Mahajan
Contributions
Contributions
Abstract
Abstract: PB1740
Type: Publication Only
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin’s lymphoma(NHL), accounting for approximately 30% of all new diagnoses. We conducted the retrospective study in our institution to analyze the main clinical features at diagnosis, response to therapy and the outcome of patients diagnosed with DLBCL.
Aims
To analyze the prognostic factors, response to therapy and the outcome of patients with DLBCL.
Methods
This study enrolled 74 patients with histologically confirmed diagnosis of DLBCL treated from January 2003 to December 2014. Complete clinical patient and disease related details were recorded. All patients were treated with chemotherapy with or without radiotherapy. Clinical features, treatment response and impact of different prognostic factors on clinical outcome were analyzed. Bulky disease was defined as any mass greater than 10cm in diameter.
Results
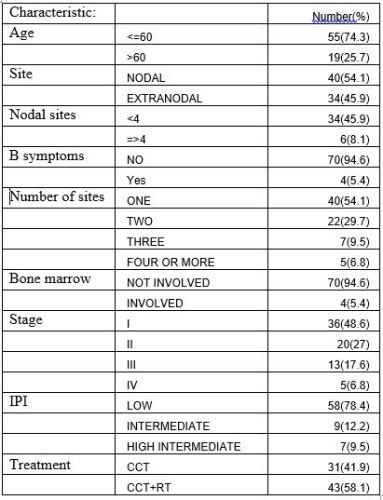
Median age of presentation was 50 years (range 18-85 years). 55(74.3%) of the patients were <60 years age and 19(25.7%) were >60 years age. Out of 74 patients, 53 were males and 21 were females. Ann Arbor clinical stage at diagnosis was 36(48.6%) stage I, 20(27%) stage II, 13 (17.6%) stage III, and 5(6.8%) stage IV respectively. Bulky disease was present in 6 patients (8.1%). Nodal disease was present in 40(54.1%) patients and 34(45.9%) had extranodal disease presentation. Supradiaphragmatic disease was seen in 44(59.5%) and 15(20.3%) had infradiaphragmatic as well as disease on both sides of the diaphragm. Most of the patients (93.2%) received either CHOP or R-CHOP chemotherapy. 43(58.1%) patients received consolidative radiotherapy. The median follow-up period was 22 months (range, 2 to 147 months). Complete response was seen in 51(68.9%) patients.With addition of radiation 9.4% improvement in local control was seen. Relapses was seen in 10(13.5%) patients, out of which 5(6.8%) had nodal and 5(6.8%) had visceral relapse. At 22 months, disease free survival (DFS) and overall survival (OS) was 66% and 81.5% respectively. Stage, International prognostic index (IPI), supradiaphragmatic disease, number of sites, extranodal diasease and number of nodal sites involvement were important prognostic factors having significant impact on response, DFS and OS.
Conclusion
This study represents the largest Indian experience to treat DLBCL. Stage, IPI, supradiaphragmatic disease, number of sites, extranodal disease and number of nodal sites were the important prognostic factors for response, DFS and OS.
Session topic: E-poster
Keyword(s): Clinical outcome, Diffuse large B cell lymphoma
Type: Publication Only
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin’s lymphoma(NHL), accounting for approximately 30% of all new diagnoses. We conducted the retrospective study in our institution to analyze the main clinical features at diagnosis, response to therapy and the outcome of patients diagnosed with DLBCL.
Aims
To analyze the prognostic factors, response to therapy and the outcome of patients with DLBCL.
Methods
This study enrolled 74 patients with histologically confirmed diagnosis of DLBCL treated from January 2003 to December 2014. Complete clinical patient and disease related details were recorded. All patients were treated with chemotherapy with or without radiotherapy. Clinical features, treatment response and impact of different prognostic factors on clinical outcome were analyzed. Bulky disease was defined as any mass greater than 10cm in diameter.
Results
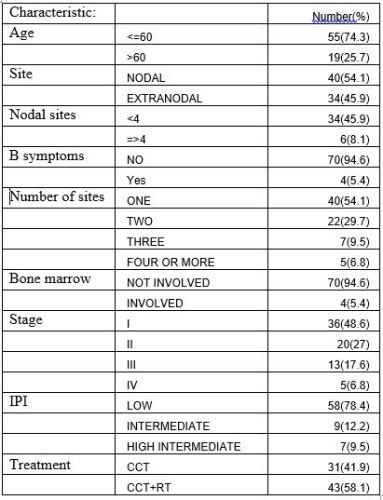
Median age of presentation was 50 years (range 18-85 years). 55(74.3%) of the patients were <60 years age and 19(25.7%) were >60 years age. Out of 74 patients, 53 were males and 21 were females. Ann Arbor clinical stage at diagnosis was 36(48.6%) stage I, 20(27%) stage II, 13 (17.6%) stage III, and 5(6.8%) stage IV respectively. Bulky disease was present in 6 patients (8.1%). Nodal disease was present in 40(54.1%) patients and 34(45.9%) had extranodal disease presentation. Supradiaphragmatic disease was seen in 44(59.5%) and 15(20.3%) had infradiaphragmatic as well as disease on both sides of the diaphragm. Most of the patients (93.2%) received either CHOP or R-CHOP chemotherapy. 43(58.1%) patients received consolidative radiotherapy. The median follow-up period was 22 months (range, 2 to 147 months). Complete response was seen in 51(68.9%) patients.With addition of radiation 9.4% improvement in local control was seen. Relapses was seen in 10(13.5%) patients, out of which 5(6.8%) had nodal and 5(6.8%) had visceral relapse. At 22 months, disease free survival (DFS) and overall survival (OS) was 66% and 81.5% respectively. Stage, International prognostic index (IPI), supradiaphragmatic disease, number of sites, extranodal diasease and number of nodal sites involvement were important prognostic factors having significant impact on response, DFS and OS.
Conclusion
This study represents the largest Indian experience to treat DLBCL. Stage, IPI, supradiaphragmatic disease, number of sites, extranodal disease and number of nodal sites were the important prognostic factors for response, DFS and OS.
Session topic: E-poster
Keyword(s): Clinical outcome, Diffuse large B cell lymphoma
Abstract: PB1740
Type: Publication Only
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin’s lymphoma(NHL), accounting for approximately 30% of all new diagnoses. We conducted the retrospective study in our institution to analyze the main clinical features at diagnosis, response to therapy and the outcome of patients diagnosed with DLBCL.
Aims
To analyze the prognostic factors, response to therapy and the outcome of patients with DLBCL.
Methods
This study enrolled 74 patients with histologically confirmed diagnosis of DLBCL treated from January 2003 to December 2014. Complete clinical patient and disease related details were recorded. All patients were treated with chemotherapy with or without radiotherapy. Clinical features, treatment response and impact of different prognostic factors on clinical outcome were analyzed. Bulky disease was defined as any mass greater than 10cm in diameter.
Results
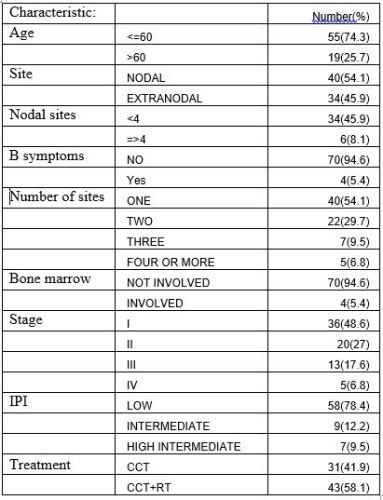
Median age of presentation was 50 years (range 18-85 years). 55(74.3%) of the patients were <60 years age and 19(25.7%) were >60 years age. Out of 74 patients, 53 were males and 21 were females. Ann Arbor clinical stage at diagnosis was 36(48.6%) stage I, 20(27%) stage II, 13 (17.6%) stage III, and 5(6.8%) stage IV respectively. Bulky disease was present in 6 patients (8.1%). Nodal disease was present in 40(54.1%) patients and 34(45.9%) had extranodal disease presentation. Supradiaphragmatic disease was seen in 44(59.5%) and 15(20.3%) had infradiaphragmatic as well as disease on both sides of the diaphragm. Most of the patients (93.2%) received either CHOP or R-CHOP chemotherapy. 43(58.1%) patients received consolidative radiotherapy. The median follow-up period was 22 months (range, 2 to 147 months). Complete response was seen in 51(68.9%) patients.With addition of radiation 9.4% improvement in local control was seen. Relapses was seen in 10(13.5%) patients, out of which 5(6.8%) had nodal and 5(6.8%) had visceral relapse. At 22 months, disease free survival (DFS) and overall survival (OS) was 66% and 81.5% respectively. Stage, International prognostic index (IPI), supradiaphragmatic disease, number of sites, extranodal diasease and number of nodal sites involvement were important prognostic factors having significant impact on response, DFS and OS.
Conclusion
This study represents the largest Indian experience to treat DLBCL. Stage, IPI, supradiaphragmatic disease, number of sites, extranodal disease and number of nodal sites were the important prognostic factors for response, DFS and OS.
Session topic: E-poster
Keyword(s): Clinical outcome, Diffuse large B cell lymphoma
Type: Publication Only
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin’s lymphoma(NHL), accounting for approximately 30% of all new diagnoses. We conducted the retrospective study in our institution to analyze the main clinical features at diagnosis, response to therapy and the outcome of patients diagnosed with DLBCL.
Aims
To analyze the prognostic factors, response to therapy and the outcome of patients with DLBCL.
Methods
This study enrolled 74 patients with histologically confirmed diagnosis of DLBCL treated from January 2003 to December 2014. Complete clinical patient and disease related details were recorded. All patients were treated with chemotherapy with or without radiotherapy. Clinical features, treatment response and impact of different prognostic factors on clinical outcome were analyzed. Bulky disease was defined as any mass greater than 10cm in diameter.
Results
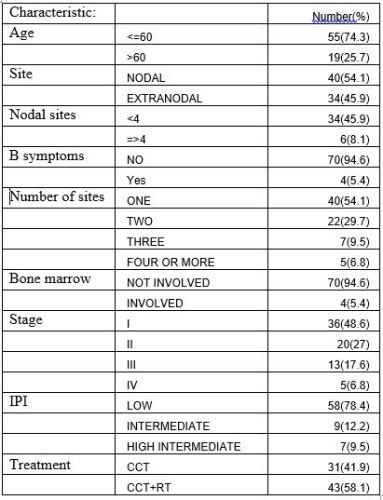
Median age of presentation was 50 years (range 18-85 years). 55(74.3%) of the patients were <60 years age and 19(25.7%) were >60 years age. Out of 74 patients, 53 were males and 21 were females. Ann Arbor clinical stage at diagnosis was 36(48.6%) stage I, 20(27%) stage II, 13 (17.6%) stage III, and 5(6.8%) stage IV respectively. Bulky disease was present in 6 patients (8.1%). Nodal disease was present in 40(54.1%) patients and 34(45.9%) had extranodal disease presentation. Supradiaphragmatic disease was seen in 44(59.5%) and 15(20.3%) had infradiaphragmatic as well as disease on both sides of the diaphragm. Most of the patients (93.2%) received either CHOP or R-CHOP chemotherapy. 43(58.1%) patients received consolidative radiotherapy. The median follow-up period was 22 months (range, 2 to 147 months). Complete response was seen in 51(68.9%) patients.With addition of radiation 9.4% improvement in local control was seen. Relapses was seen in 10(13.5%) patients, out of which 5(6.8%) had nodal and 5(6.8%) had visceral relapse. At 22 months, disease free survival (DFS) and overall survival (OS) was 66% and 81.5% respectively. Stage, International prognostic index (IPI), supradiaphragmatic disease, number of sites, extranodal diasease and number of nodal sites involvement were important prognostic factors having significant impact on response, DFS and OS.
Conclusion
This study represents the largest Indian experience to treat DLBCL. Stage, IPI, supradiaphragmatic disease, number of sites, extranodal disease and number of nodal sites were the important prognostic factors for response, DFS and OS.
Session topic: E-poster
Keyword(s): Clinical outcome, Diffuse large B cell lymphoma
{{ help_message }}
{{filter}}


