THE COMPARISON OF THE PROGNOSIS SCORING SYSTEMS BETWEEN EVENT-FREE SURVIVAL AT FIRST 24 MONTHS AND OVERALL SURVIVAL IN PATIENTS WITH DIFFUSE LARGE B-CELL LYMPHOMA
(Abstract release date: 05/19/16)
EHA Library. Maden M. 06/09/16; 134621; PB1721

Dr. Muhammet Maden
Contributions
Contributions
Abstract
Abstract: PB1721
Type: Publication Only
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma (NHL). R-CHOP (Rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) is curative in the majority of DLBCL patients. However, about one-third of patients will have refractory disease or relapse following the therapy. Therefore, risk stratification at diagnosis for patients with DLBCL is of great clinical interest. Recently, it is shown that event-free survival (EFS) at first 24 months from the time of diagnosis in patients who received rituximab-based chemotherapy onwards the similar survival rates with healthy patients in their own age group and gender. Recently, the scoring system for prognosis called IPI24 is effective to predict the first 24-month EFS (EFS24) in DLBCL patients.
Aims
In this study, we aimed to compare the risk stratification anticipated by IPI24, IPI and NCCN-IPI for patients treated with RCHOP in the first EFS24 and overall survival in Trakya University Medical Faculty Hematology department and identify the prognosis scoring system which makes best risk stratification.
Methods
Clinical and laboratory data of 284 patients who have been diagnosed with NHL in our center since 2004 were retrospectively analyzed. The patients who were under the age of 50 and over the age of 85 and also receiving chemotherapy except for R-CHOP, apart from DLBCL were subtracted from the study and 103 patients (57 M, 46 F) were enrolled in the study. Clinical and laboratory data of the patients were obtained by scanning files. According to IPI and NCCN-IPI, patients were analyzed depending on 4 risk groups (low, low-intermediate, high-intermediate, high) which are created on using age, LDH, ECOG score, extranodal organ involvement and Ann Arbor stage. But the risk of events on the first 24 months calculated by IPI24 were calculated with the QX calculator using age, sex, absolute lymphocyte count, bulky lymph node masses (> 10cm), LDH, ECOG score and Ann Arbor stage. Data were analyzed with SPSS statistical software. Whether the prognostic scores were independent indicators or not in terms of survival and event-free survival was examined using Cox regression analysis. P<0.05 was considered significantly.
Results
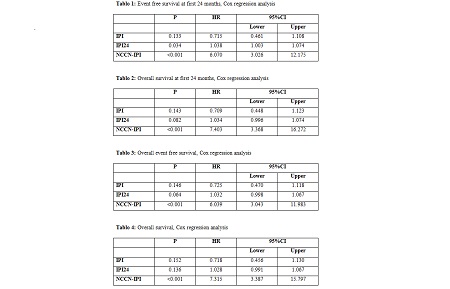
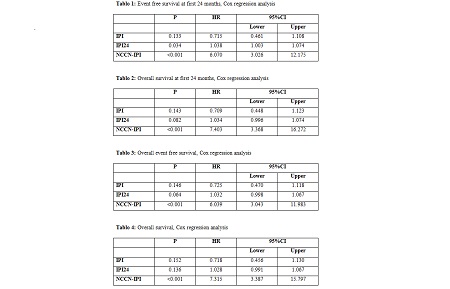
The mean age of 103 patients in our study was 60±9 years and in %48 of them had extranodal disease, %64 of the patients had advanced disease, %24 of the patients had solid disease. In %37 of the patients ECOG score was ≥2. %38 of the cases were dead. NCCN-IPI was the most successful prognostic model to predict EFS24 in the patients (p<0.001). While IPI24 was statistically significant to predict EFS24 (p=0.03), IPI was not sufficient (p=0.13) (Table 1). While the best prognostic model was NCCN-IPI to predict the overall survival in 24 months (p<0.001), IPI and IPI24 were insufficient (with order p=0.08, p=0.7) (Table 2). To predict the overall EFS and overall survival in the patients, the best prognostic model was NCCN-IPI (p<0.001), but IPI and IPI24 were insufficient (p>0.05) (with order Table 3 and 4).
Conclusion
In DLBCL patients before treatment, while NCCN-IPI was superior to IPI 24 as a prognostic scoring system to predict EFS24, IPI was insufficient. Similarly to predict overall survival, NCCN-IPI was the best prognostic model. Due to the mean age of our patients was high and the number of the patients was not enough IPI24 could be insufficient when compared to NCCN-IPI to predict EFS24 and overall survival. It would be useful to do more studies to show the effectiveness of IPI24 for determining the risk factors before the treatment on DLBCL patients.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, International prognostic index, Survival prediction
Type: Publication Only
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma (NHL). R-CHOP (Rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) is curative in the majority of DLBCL patients. However, about one-third of patients will have refractory disease or relapse following the therapy. Therefore, risk stratification at diagnosis for patients with DLBCL is of great clinical interest. Recently, it is shown that event-free survival (EFS) at first 24 months from the time of diagnosis in patients who received rituximab-based chemotherapy onwards the similar survival rates with healthy patients in their own age group and gender. Recently, the scoring system for prognosis called IPI24 is effective to predict the first 24-month EFS (EFS24) in DLBCL patients.
Aims
In this study, we aimed to compare the risk stratification anticipated by IPI24, IPI and NCCN-IPI for patients treated with RCHOP in the first EFS24 and overall survival in Trakya University Medical Faculty Hematology department and identify the prognosis scoring system which makes best risk stratification.
Methods
Clinical and laboratory data of 284 patients who have been diagnosed with NHL in our center since 2004 were retrospectively analyzed. The patients who were under the age of 50 and over the age of 85 and also receiving chemotherapy except for R-CHOP, apart from DLBCL were subtracted from the study and 103 patients (57 M, 46 F) were enrolled in the study. Clinical and laboratory data of the patients were obtained by scanning files. According to IPI and NCCN-IPI, patients were analyzed depending on 4 risk groups (low, low-intermediate, high-intermediate, high) which are created on using age, LDH, ECOG score, extranodal organ involvement and Ann Arbor stage. But the risk of events on the first 24 months calculated by IPI24 were calculated with the QX calculator using age, sex, absolute lymphocyte count, bulky lymph node masses (> 10cm), LDH, ECOG score and Ann Arbor stage. Data were analyzed with SPSS statistical software. Whether the prognostic scores were independent indicators or not in terms of survival and event-free survival was examined using Cox regression analysis. P<0.05 was considered significantly.
Results
The mean age of 103 patients in our study was 60±9 years and in %48 of them had extranodal disease, %64 of the patients had advanced disease, %24 of the patients had solid disease. In %37 of the patients ECOG score was ≥2. %38 of the cases were dead. NCCN-IPI was the most successful prognostic model to predict EFS24 in the patients (p<0.001). While IPI24 was statistically significant to predict EFS24 (p=0.03), IPI was not sufficient (p=0.13) (Table 1). While the best prognostic model was NCCN-IPI to predict the overall survival in 24 months (p<0.001), IPI and IPI24 were insufficient (with order p=0.08, p=0.7) (Table 2). To predict the overall EFS and overall survival in the patients, the best prognostic model was NCCN-IPI (p<0.001), but IPI and IPI24 were insufficient (p>0.05) (with order Table 3 and 4).
Conclusion
In DLBCL patients before treatment, while NCCN-IPI was superior to IPI 24 as a prognostic scoring system to predict EFS24, IPI was insufficient. Similarly to predict overall survival, NCCN-IPI was the best prognostic model. Due to the mean age of our patients was high and the number of the patients was not enough IPI24 could be insufficient when compared to NCCN-IPI to predict EFS24 and overall survival. It would be useful to do more studies to show the effectiveness of IPI24 for determining the risk factors before the treatment on DLBCL patients.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, International prognostic index, Survival prediction
Abstract: PB1721
Type: Publication Only
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma (NHL). R-CHOP (Rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) is curative in the majority of DLBCL patients. However, about one-third of patients will have refractory disease or relapse following the therapy. Therefore, risk stratification at diagnosis for patients with DLBCL is of great clinical interest. Recently, it is shown that event-free survival (EFS) at first 24 months from the time of diagnosis in patients who received rituximab-based chemotherapy onwards the similar survival rates with healthy patients in their own age group and gender. Recently, the scoring system for prognosis called IPI24 is effective to predict the first 24-month EFS (EFS24) in DLBCL patients.
Aims
In this study, we aimed to compare the risk stratification anticipated by IPI24, IPI and NCCN-IPI for patients treated with RCHOP in the first EFS24 and overall survival in Trakya University Medical Faculty Hematology department and identify the prognosis scoring system which makes best risk stratification.
Methods
Clinical and laboratory data of 284 patients who have been diagnosed with NHL in our center since 2004 were retrospectively analyzed. The patients who were under the age of 50 and over the age of 85 and also receiving chemotherapy except for R-CHOP, apart from DLBCL were subtracted from the study and 103 patients (57 M, 46 F) were enrolled in the study. Clinical and laboratory data of the patients were obtained by scanning files. According to IPI and NCCN-IPI, patients were analyzed depending on 4 risk groups (low, low-intermediate, high-intermediate, high) which are created on using age, LDH, ECOG score, extranodal organ involvement and Ann Arbor stage. But the risk of events on the first 24 months calculated by IPI24 were calculated with the QX calculator using age, sex, absolute lymphocyte count, bulky lymph node masses (> 10cm), LDH, ECOG score and Ann Arbor stage. Data were analyzed with SPSS statistical software. Whether the prognostic scores were independent indicators or not in terms of survival and event-free survival was examined using Cox regression analysis. P<0.05 was considered significantly.
Results
The mean age of 103 patients in our study was 60±9 years and in %48 of them had extranodal disease, %64 of the patients had advanced disease, %24 of the patients had solid disease. In %37 of the patients ECOG score was ≥2. %38 of the cases were dead. NCCN-IPI was the most successful prognostic model to predict EFS24 in the patients (p<0.001). While IPI24 was statistically significant to predict EFS24 (p=0.03), IPI was not sufficient (p=0.13) (Table 1). While the best prognostic model was NCCN-IPI to predict the overall survival in 24 months (p<0.001), IPI and IPI24 were insufficient (with order p=0.08, p=0.7) (Table 2). To predict the overall EFS and overall survival in the patients, the best prognostic model was NCCN-IPI (p<0.001), but IPI and IPI24 were insufficient (p>0.05) (with order Table 3 and 4).
Conclusion
In DLBCL patients before treatment, while NCCN-IPI was superior to IPI 24 as a prognostic scoring system to predict EFS24, IPI was insufficient. Similarly to predict overall survival, NCCN-IPI was the best prognostic model. Due to the mean age of our patients was high and the number of the patients was not enough IPI24 could be insufficient when compared to NCCN-IPI to predict EFS24 and overall survival. It would be useful to do more studies to show the effectiveness of IPI24 for determining the risk factors before the treatment on DLBCL patients.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, International prognostic index, Survival prediction
Type: Publication Only
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma (NHL). R-CHOP (Rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) is curative in the majority of DLBCL patients. However, about one-third of patients will have refractory disease or relapse following the therapy. Therefore, risk stratification at diagnosis for patients with DLBCL is of great clinical interest. Recently, it is shown that event-free survival (EFS) at first 24 months from the time of diagnosis in patients who received rituximab-based chemotherapy onwards the similar survival rates with healthy patients in their own age group and gender. Recently, the scoring system for prognosis called IPI24 is effective to predict the first 24-month EFS (EFS24) in DLBCL patients.
Aims
In this study, we aimed to compare the risk stratification anticipated by IPI24, IPI and NCCN-IPI for patients treated with RCHOP in the first EFS24 and overall survival in Trakya University Medical Faculty Hematology department and identify the prognosis scoring system which makes best risk stratification.
Methods
Clinical and laboratory data of 284 patients who have been diagnosed with NHL in our center since 2004 were retrospectively analyzed. The patients who were under the age of 50 and over the age of 85 and also receiving chemotherapy except for R-CHOP, apart from DLBCL were subtracted from the study and 103 patients (57 M, 46 F) were enrolled in the study. Clinical and laboratory data of the patients were obtained by scanning files. According to IPI and NCCN-IPI, patients were analyzed depending on 4 risk groups (low, low-intermediate, high-intermediate, high) which are created on using age, LDH, ECOG score, extranodal organ involvement and Ann Arbor stage. But the risk of events on the first 24 months calculated by IPI24 were calculated with the QX calculator using age, sex, absolute lymphocyte count, bulky lymph node masses (> 10cm), LDH, ECOG score and Ann Arbor stage. Data were analyzed with SPSS statistical software. Whether the prognostic scores were independent indicators or not in terms of survival and event-free survival was examined using Cox regression analysis. P<0.05 was considered significantly.
Results
The mean age of 103 patients in our study was 60±9 years and in %48 of them had extranodal disease, %64 of the patients had advanced disease, %24 of the patients had solid disease. In %37 of the patients ECOG score was ≥2. %38 of the cases were dead. NCCN-IPI was the most successful prognostic model to predict EFS24 in the patients (p<0.001). While IPI24 was statistically significant to predict EFS24 (p=0.03), IPI was not sufficient (p=0.13) (Table 1). While the best prognostic model was NCCN-IPI to predict the overall survival in 24 months (p<0.001), IPI and IPI24 were insufficient (with order p=0.08, p=0.7) (Table 2). To predict the overall EFS and overall survival in the patients, the best prognostic model was NCCN-IPI (p<0.001), but IPI and IPI24 were insufficient (p>0.05) (with order Table 3 and 4).
Conclusion
In DLBCL patients before treatment, while NCCN-IPI was superior to IPI 24 as a prognostic scoring system to predict EFS24, IPI was insufficient. Similarly to predict overall survival, NCCN-IPI was the best prognostic model. Due to the mean age of our patients was high and the number of the patients was not enough IPI24 could be insufficient when compared to NCCN-IPI to predict EFS24 and overall survival. It would be useful to do more studies to show the effectiveness of IPI24 for determining the risk factors before the treatment on DLBCL patients.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, International prognostic index, Survival prediction
{{ help_message }}
{{filter}}


