TWENTY YEARS? EXPERIENCE OF TREATMENT OF ADOLESCENTS AND YOUNG ADULTS WITH NON-HODGKIN LYMPHOMA ? A SINGLE CENTER EXPERIENCE
(Abstract release date: 05/19/16)
EHA Library. Ratzon R. 06/09/16; 134606; PB1706

Mr. Roy Ratzon
Contributions
Contributions
Abstract
Abstract: PB1706
Type: Publication Only
Background
Adolescents and young adults (AYAs) with non-Hodgkin lymphomas (NHL) comprise a unique group of patients, under-represented in clinical trials. Furthermore, the prognosis of these patients is inferior to that of younger patients with hematological malignancies. Therefore, many questions regarding the biology and treatment strategies of this group remain unanswered.
Aims
We aimed to determine the characteristics of AYA NHL patients in the last 20 years in a single tertiary center. Also, we intended to identify risk factors for poor prognosis in this population.
Methods
We reviewed retrospectively the database of our NHL patients at the Rabin Medical Center between the years 1995-2014 and identified patients who met the following criteria: age 18-40 years old, a confirmed histological diagnosis of NHL and treatment in our institution, with at least one year follow-up.In order to define prognostic factors we used the Mann-Whitney U test to compare between the group of patients with poor outcome and those with better outcome. 3-year event free (EFS) and overall survival (OS) were calculated according to the Kaplan-Meier analysis.
Results
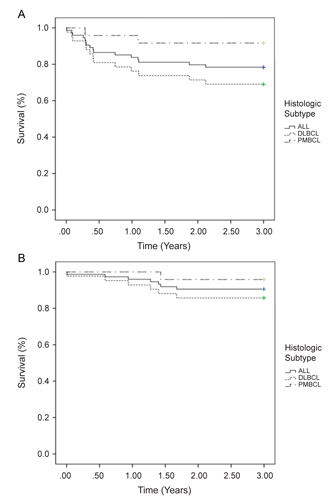
A total of 85 patients with confirmed diagnosis of NHL were included in this study. Median age was 32 (range, 18-40) years with 42% male. 74 patients (87%) were diagnosed with aggressive lymphoma and 11 (13%) with indolent lymphoma.The histologic subtypes included diffuse large B-cell lymphoma - 50%, primary mediastinal B-cell lymphoma - 28%, Burkitt lymphoma - 9%, follicular lymphoma - 12%, marginal zone lymphoma - 1%. Due to the small number of patients with indolent lymphoma, this group of patients was not analyzed.B symptoms were present in 32 patients (43%) and 48 had bulky disease (68%). More than half of the patients had advanced stage disease. The IPI score was low (0-1) in 40 patients (56%), low-intermediate (2) in 12 patients (17%) and intermediate-high (3) in 19 patients (27%). Half of the patients were treated with CHOP like regimen (CHOP, R-CHOP, CHOEP), 30% were treated with MACOP\VACOP-B with or without rituximab and 16% received intensive regimens (hyper-CVAD & GMALL). Most patients (74%) received rituximab as part of their treatment regimen.92% of the patients achieved complete remission (CR), 19% of them relapsed. 14 patients (19%) underwent stem cell transplantation: 12 autologous and 2 allogeneic. Overall, 7 patients died during follow - up, 6 of them with DLBCL and 1 with PMBCL. All died due to progressive disease. 3-year EFS and 3-year OS for the whole group was 74% and 90%, respectively, for patients with DLBCL-67% and 86%, respectively and for patients with PMBCL- 90% and 96%, respectively (Figure 1).The results of Mann-Whitney U test revealed that the group of patients with worse outcome had higher IPI (p=0.03), higher aaIPI (p=0.03) and lower use of rituximab in the treatment regimen compared to those with better outcome (p=0.05).
Conclusion
In our cohort of AYA patients with NHL, DLBCL was the most frequent subtype of lymphoma followed by PMBCL. This is in accordance with previous reports. The 3 year EFS and OS of AYA patients with DLBCL in our cohort were lower or similar to other studies of AYA patients while results for patients with PMBCL were superior to those in the literature. The aaIPI/IPI score was validated in our cohort as a reliable prognostic index. As in adults, the inclusion of rituximab in a combined regimen was associated with better outcomes than chemotherapy alone.
Session topic: E-poster
Keyword(s): Adolescents, DLBCL, NHL, Young adult
Type: Publication Only
Background
Adolescents and young adults (AYAs) with non-Hodgkin lymphomas (NHL) comprise a unique group of patients, under-represented in clinical trials. Furthermore, the prognosis of these patients is inferior to that of younger patients with hematological malignancies. Therefore, many questions regarding the biology and treatment strategies of this group remain unanswered.
Aims
We aimed to determine the characteristics of AYA NHL patients in the last 20 years in a single tertiary center. Also, we intended to identify risk factors for poor prognosis in this population.
Methods
We reviewed retrospectively the database of our NHL patients at the Rabin Medical Center between the years 1995-2014 and identified patients who met the following criteria: age 18-40 years old, a confirmed histological diagnosis of NHL and treatment in our institution, with at least one year follow-up.In order to define prognostic factors we used the Mann-Whitney U test to compare between the group of patients with poor outcome and those with better outcome. 3-year event free (EFS) and overall survival (OS) were calculated according to the Kaplan-Meier analysis.
Results
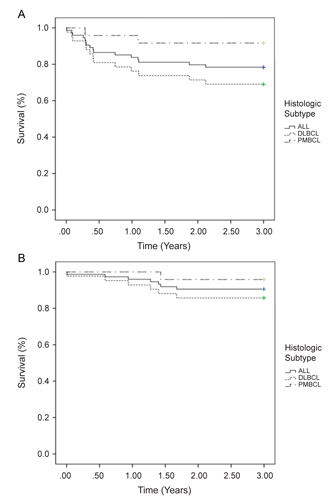
A total of 85 patients with confirmed diagnosis of NHL were included in this study. Median age was 32 (range, 18-40) years with 42% male. 74 patients (87%) were diagnosed with aggressive lymphoma and 11 (13%) with indolent lymphoma.The histologic subtypes included diffuse large B-cell lymphoma - 50%, primary mediastinal B-cell lymphoma - 28%, Burkitt lymphoma - 9%, follicular lymphoma - 12%, marginal zone lymphoma - 1%. Due to the small number of patients with indolent lymphoma, this group of patients was not analyzed.B symptoms were present in 32 patients (43%) and 48 had bulky disease (68%). More than half of the patients had advanced stage disease. The IPI score was low (0-1) in 40 patients (56%), low-intermediate (2) in 12 patients (17%) and intermediate-high (3) in 19 patients (27%). Half of the patients were treated with CHOP like regimen (CHOP, R-CHOP, CHOEP), 30% were treated with MACOP\VACOP-B with or without rituximab and 16% received intensive regimens (hyper-CVAD & GMALL). Most patients (74%) received rituximab as part of their treatment regimen.92% of the patients achieved complete remission (CR), 19% of them relapsed. 14 patients (19%) underwent stem cell transplantation: 12 autologous and 2 allogeneic. Overall, 7 patients died during follow - up, 6 of them with DLBCL and 1 with PMBCL. All died due to progressive disease. 3-year EFS and 3-year OS for the whole group was 74% and 90%, respectively, for patients with DLBCL-67% and 86%, respectively and for patients with PMBCL- 90% and 96%, respectively (Figure 1).The results of Mann-Whitney U test revealed that the group of patients with worse outcome had higher IPI (p=0.03), higher aaIPI (p=0.03) and lower use of rituximab in the treatment regimen compared to those with better outcome (p=0.05).
Conclusion
In our cohort of AYA patients with NHL, DLBCL was the most frequent subtype of lymphoma followed by PMBCL. This is in accordance with previous reports. The 3 year EFS and OS of AYA patients with DLBCL in our cohort were lower or similar to other studies of AYA patients while results for patients with PMBCL were superior to those in the literature. The aaIPI/IPI score was validated in our cohort as a reliable prognostic index. As in adults, the inclusion of rituximab in a combined regimen was associated with better outcomes than chemotherapy alone.
Session topic: E-poster
Keyword(s): Adolescents, DLBCL, NHL, Young adult
Abstract: PB1706
Type: Publication Only
Background
Adolescents and young adults (AYAs) with non-Hodgkin lymphomas (NHL) comprise a unique group of patients, under-represented in clinical trials. Furthermore, the prognosis of these patients is inferior to that of younger patients with hematological malignancies. Therefore, many questions regarding the biology and treatment strategies of this group remain unanswered.
Aims
We aimed to determine the characteristics of AYA NHL patients in the last 20 years in a single tertiary center. Also, we intended to identify risk factors for poor prognosis in this population.
Methods
We reviewed retrospectively the database of our NHL patients at the Rabin Medical Center between the years 1995-2014 and identified patients who met the following criteria: age 18-40 years old, a confirmed histological diagnosis of NHL and treatment in our institution, with at least one year follow-up.In order to define prognostic factors we used the Mann-Whitney U test to compare between the group of patients with poor outcome and those with better outcome. 3-year event free (EFS) and overall survival (OS) were calculated according to the Kaplan-Meier analysis.
Results
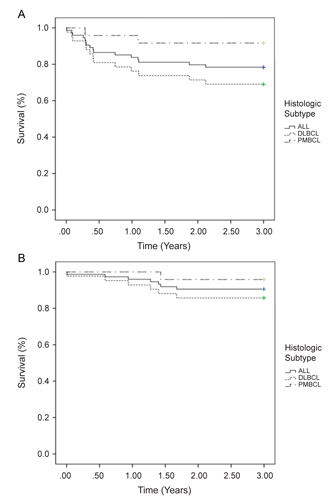
A total of 85 patients with confirmed diagnosis of NHL were included in this study. Median age was 32 (range, 18-40) years with 42% male. 74 patients (87%) were diagnosed with aggressive lymphoma and 11 (13%) with indolent lymphoma.The histologic subtypes included diffuse large B-cell lymphoma - 50%, primary mediastinal B-cell lymphoma - 28%, Burkitt lymphoma - 9%, follicular lymphoma - 12%, marginal zone lymphoma - 1%. Due to the small number of patients with indolent lymphoma, this group of patients was not analyzed.B symptoms were present in 32 patients (43%) and 48 had bulky disease (68%). More than half of the patients had advanced stage disease. The IPI score was low (0-1) in 40 patients (56%), low-intermediate (2) in 12 patients (17%) and intermediate-high (3) in 19 patients (27%). Half of the patients were treated with CHOP like regimen (CHOP, R-CHOP, CHOEP), 30% were treated with MACOP\VACOP-B with or without rituximab and 16% received intensive regimens (hyper-CVAD & GMALL). Most patients (74%) received rituximab as part of their treatment regimen.92% of the patients achieved complete remission (CR), 19% of them relapsed. 14 patients (19%) underwent stem cell transplantation: 12 autologous and 2 allogeneic. Overall, 7 patients died during follow - up, 6 of them with DLBCL and 1 with PMBCL. All died due to progressive disease. 3-year EFS and 3-year OS for the whole group was 74% and 90%, respectively, for patients with DLBCL-67% and 86%, respectively and for patients with PMBCL- 90% and 96%, respectively (Figure 1).The results of Mann-Whitney U test revealed that the group of patients with worse outcome had higher IPI (p=0.03), higher aaIPI (p=0.03) and lower use of rituximab in the treatment regimen compared to those with better outcome (p=0.05).
Conclusion
In our cohort of AYA patients with NHL, DLBCL was the most frequent subtype of lymphoma followed by PMBCL. This is in accordance with previous reports. The 3 year EFS and OS of AYA patients with DLBCL in our cohort were lower or similar to other studies of AYA patients while results for patients with PMBCL were superior to those in the literature. The aaIPI/IPI score was validated in our cohort as a reliable prognostic index. As in adults, the inclusion of rituximab in a combined regimen was associated with better outcomes than chemotherapy alone.
Session topic: E-poster
Keyword(s): Adolescents, DLBCL, NHL, Young adult
Type: Publication Only
Background
Adolescents and young adults (AYAs) with non-Hodgkin lymphomas (NHL) comprise a unique group of patients, under-represented in clinical trials. Furthermore, the prognosis of these patients is inferior to that of younger patients with hematological malignancies. Therefore, many questions regarding the biology and treatment strategies of this group remain unanswered.
Aims
We aimed to determine the characteristics of AYA NHL patients in the last 20 years in a single tertiary center. Also, we intended to identify risk factors for poor prognosis in this population.
Methods
We reviewed retrospectively the database of our NHL patients at the Rabin Medical Center between the years 1995-2014 and identified patients who met the following criteria: age 18-40 years old, a confirmed histological diagnosis of NHL and treatment in our institution, with at least one year follow-up.In order to define prognostic factors we used the Mann-Whitney U test to compare between the group of patients with poor outcome and those with better outcome. 3-year event free (EFS) and overall survival (OS) were calculated according to the Kaplan-Meier analysis.
Results
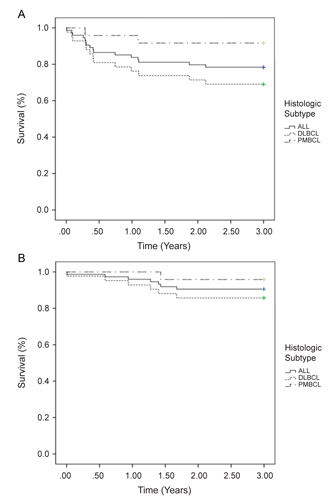
A total of 85 patients with confirmed diagnosis of NHL were included in this study. Median age was 32 (range, 18-40) years with 42% male. 74 patients (87%) were diagnosed with aggressive lymphoma and 11 (13%) with indolent lymphoma.The histologic subtypes included diffuse large B-cell lymphoma - 50%, primary mediastinal B-cell lymphoma - 28%, Burkitt lymphoma - 9%, follicular lymphoma - 12%, marginal zone lymphoma - 1%. Due to the small number of patients with indolent lymphoma, this group of patients was not analyzed.B symptoms were present in 32 patients (43%) and 48 had bulky disease (68%). More than half of the patients had advanced stage disease. The IPI score was low (0-1) in 40 patients (56%), low-intermediate (2) in 12 patients (17%) and intermediate-high (3) in 19 patients (27%). Half of the patients were treated with CHOP like regimen (CHOP, R-CHOP, CHOEP), 30% were treated with MACOP\VACOP-B with or without rituximab and 16% received intensive regimens (hyper-CVAD & GMALL). Most patients (74%) received rituximab as part of their treatment regimen.92% of the patients achieved complete remission (CR), 19% of them relapsed. 14 patients (19%) underwent stem cell transplantation: 12 autologous and 2 allogeneic. Overall, 7 patients died during follow - up, 6 of them with DLBCL and 1 with PMBCL. All died due to progressive disease. 3-year EFS and 3-year OS for the whole group was 74% and 90%, respectively, for patients with DLBCL-67% and 86%, respectively and for patients with PMBCL- 90% and 96%, respectively (Figure 1).The results of Mann-Whitney U test revealed that the group of patients with worse outcome had higher IPI (p=0.03), higher aaIPI (p=0.03) and lower use of rituximab in the treatment regimen compared to those with better outcome (p=0.05).
Conclusion
In our cohort of AYA patients with NHL, DLBCL was the most frequent subtype of lymphoma followed by PMBCL. This is in accordance with previous reports. The 3 year EFS and OS of AYA patients with DLBCL in our cohort were lower or similar to other studies of AYA patients while results for patients with PMBCL were superior to those in the literature. The aaIPI/IPI score was validated in our cohort as a reliable prognostic index. As in adults, the inclusion of rituximab in a combined regimen was associated with better outcomes than chemotherapy alone.
Session topic: E-poster
Keyword(s): Adolescents, DLBCL, NHL, Young adult
{{ help_message }}
{{filter}}


