BASELINE RENAL FUNCTION AS A PROGNOSTIC INDICATOR IN PATIENTS WITH DIFFUSE LARGE B-CELL LYMPHOMA TREATED WITH R-CHOP IMMUNOCHEMOTHERAPY
(Abstract release date: 05/19/16)
EHA Library. Hong J. 06/09/16; 134594; PB1694

Dr. Junshik Hong
Contributions
Contributions
Abstract
Abstract: PB1694
Type: Publication Only
Background
Recently the prognostic value of baseline renal impairment (RI) has been evaluated in patients with newly diagnosed cancers: baseline RI assessed by blood urea nitrogen showed significant relationship to overall survival (OS) of patients with advanced non-small cell lung cancer (Zhang et al, Int J Cancer 2015;136:382) or to early mortality among patients with resectable pancreatic adenocarcinoma (Sohal, et al, Cancer 2015;121:1779).
Aims
In this study, we evaluated the prognostic value of baseline RI in patients with diffuse large B-cell lymphoma (DLBCL) uniformly treated with conventional three-weekly rituximab plus cyclophosphamide, adriamycin, vincristine, and prednisolone (R-CHOP21) immunochemotherapy in single institution.
Methods
Patients with newly diagnosed de novo DLBCL treated with ≥ 1 cycle of R-CHOP21 were included. Glomerular filtration rate (GFR) was calculated using serum ceratinine level from pre-treatment serum chemistry data and other clinical information. RI was defined as a GFR of < 60 mL/min/1.73 m2according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.
Results
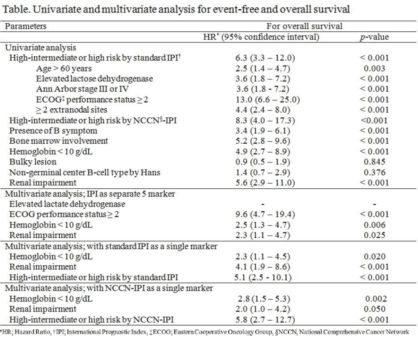
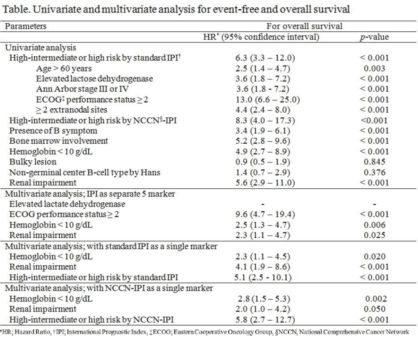
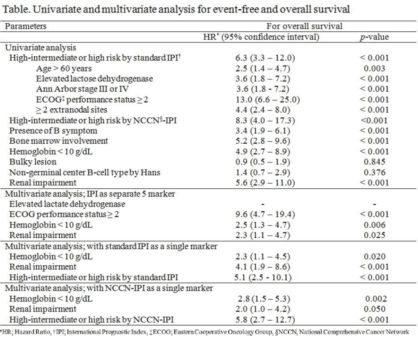
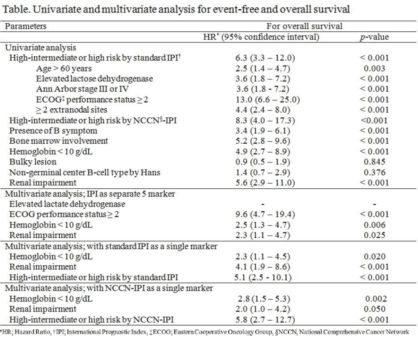
185 patients treated from Mar. 2006 to Jan. 2015 were included and analyzed. For the median follow up period of 44.1 months (95% CI, 37.5 - 50.7), 53 patients (28.6%) underwent any event and 44 (23.8%) died. 3-year Event-free (EFS) and OS were 71.1% and 76.5%, respectively. Both standard and the NCCN-IPI showed good prognostication. However, NCCN-IPI more efficiently separated patients of low-intermediate vs. high-intermediate risk compared to standard IPI, and the patients of high risk group according to NCCN-IPI showed poorer OS compared to those according to standard IPI.19 patients had RI according to CKD-EPI formula: 5 patients had pre-existing CKD, 2 had post-renal acute kidney injury (AKI) caused by DLBCL, and another 2 had hypercalcemia and/or hyperuricemia, suggesting AKI due to the electrolyte imbalance due to lymphoma. We could not define the reason of RI of the other 10 patients: they were aged ≥ 70 years (range 71 – 89) except 2 patients with 49 and 69 years, respectively. Patients with RI showed inferior OS compared to those without RI (3-yr OS 26.7% vs. 81.8%, p < 0.001). There was no difference of OS between patients with a GFR of ≥ 90 vs. ≥ 60 - 89 mL/min/1.73 m2 (3-yr OS 82.4% vs. 76.7%, p = 0.436), suggesting that only RI defined by GFR below 60 mL/min/1.73 m2 is a meaningful prognostic indicator of OS. In multivariate analysis, RI was an IPI-independent prognostic biomarker (Table).Among patients with high or high-intermediate risk according to standard IPI, patients with neither anemia of Hb < 10 g/dL nor RI had superior OS vs. patients who had one of them or vs. those with both of them. These findings were maintained when the analysis was restricted to patients with high risk according to standard IPI. Use of NCCN-IPI instead of standard IPI showed same result.
Conclusion
Patients with baseline RI had inferior OS compared to those without RI. Because RI was an independent prognostic factor for OS in multivariate analysis whereas age >60 years (or ≥ 70 or even ≥ 75 years instead) was not, RI might have a role of the biological age-indicator of patients with DLBCL and therefore affect to OS. In combination with Hb < 10 g/dL, RI enhanced prognostication in patients classified as higher risk group according to either standard or NCCN-IPI.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, Prognosis, Renal impairment
Type: Publication Only
Background
Recently the prognostic value of baseline renal impairment (RI) has been evaluated in patients with newly diagnosed cancers: baseline RI assessed by blood urea nitrogen showed significant relationship to overall survival (OS) of patients with advanced non-small cell lung cancer (Zhang et al, Int J Cancer 2015;136:382) or to early mortality among patients with resectable pancreatic adenocarcinoma (Sohal, et al, Cancer 2015;121:1779).
Aims
In this study, we evaluated the prognostic value of baseline RI in patients with diffuse large B-cell lymphoma (DLBCL) uniformly treated with conventional three-weekly rituximab plus cyclophosphamide, adriamycin, vincristine, and prednisolone (R-CHOP21) immunochemotherapy in single institution.
Methods
Patients with newly diagnosed de novo DLBCL treated with ≥ 1 cycle of R-CHOP21 were included. Glomerular filtration rate (GFR) was calculated using serum ceratinine level from pre-treatment serum chemistry data and other clinical information. RI was defined as a GFR of < 60 mL/min/1.73 m2according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.
Results
185 patients treated from Mar. 2006 to Jan. 2015 were included and analyzed. For the median follow up period of 44.1 months (95% CI, 37.5 - 50.7), 53 patients (28.6%) underwent any event and 44 (23.8%) died. 3-year Event-free (EFS) and OS were 71.1% and 76.5%, respectively. Both standard and the NCCN-IPI showed good prognostication. However, NCCN-IPI more efficiently separated patients of low-intermediate vs. high-intermediate risk compared to standard IPI, and the patients of high risk group according to NCCN-IPI showed poorer OS compared to those according to standard IPI.19 patients had RI according to CKD-EPI formula: 5 patients had pre-existing CKD, 2 had post-renal acute kidney injury (AKI) caused by DLBCL, and another 2 had hypercalcemia and/or hyperuricemia, suggesting AKI due to the electrolyte imbalance due to lymphoma. We could not define the reason of RI of the other 10 patients: they were aged ≥ 70 years (range 71 – 89) except 2 patients with 49 and 69 years, respectively. Patients with RI showed inferior OS compared to those without RI (3-yr OS 26.7% vs. 81.8%, p < 0.001). There was no difference of OS between patients with a GFR of ≥ 90 vs. ≥ 60 - 89 mL/min/1.73 m2 (3-yr OS 82.4% vs. 76.7%, p = 0.436), suggesting that only RI defined by GFR below 60 mL/min/1.73 m2 is a meaningful prognostic indicator of OS. In multivariate analysis, RI was an IPI-independent prognostic biomarker (Table).Among patients with high or high-intermediate risk according to standard IPI, patients with neither anemia of Hb < 10 g/dL nor RI had superior OS vs. patients who had one of them or vs. those with both of them. These findings were maintained when the analysis was restricted to patients with high risk according to standard IPI. Use of NCCN-IPI instead of standard IPI showed same result.
Conclusion
Patients with baseline RI had inferior OS compared to those without RI. Because RI was an independent prognostic factor for OS in multivariate analysis whereas age >60 years (or ≥ 70 or even ≥ 75 years instead) was not, RI might have a role of the biological age-indicator of patients with DLBCL and therefore affect to OS. In combination with Hb < 10 g/dL, RI enhanced prognostication in patients classified as higher risk group according to either standard or NCCN-IPI.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, Prognosis, Renal impairment
Abstract: PB1694
Type: Publication Only
Background
Recently the prognostic value of baseline renal impairment (RI) has been evaluated in patients with newly diagnosed cancers: baseline RI assessed by blood urea nitrogen showed significant relationship to overall survival (OS) of patients with advanced non-small cell lung cancer (Zhang et al, Int J Cancer 2015;136:382) or to early mortality among patients with resectable pancreatic adenocarcinoma (Sohal, et al, Cancer 2015;121:1779).
Aims
In this study, we evaluated the prognostic value of baseline RI in patients with diffuse large B-cell lymphoma (DLBCL) uniformly treated with conventional three-weekly rituximab plus cyclophosphamide, adriamycin, vincristine, and prednisolone (R-CHOP21) immunochemotherapy in single institution.
Methods
Patients with newly diagnosed de novo DLBCL treated with ≥ 1 cycle of R-CHOP21 were included. Glomerular filtration rate (GFR) was calculated using serum ceratinine level from pre-treatment serum chemistry data and other clinical information. RI was defined as a GFR of < 60 mL/min/1.73 m2according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.
Results
185 patients treated from Mar. 2006 to Jan. 2015 were included and analyzed. For the median follow up period of 44.1 months (95% CI, 37.5 - 50.7), 53 patients (28.6%) underwent any event and 44 (23.8%) died. 3-year Event-free (EFS) and OS were 71.1% and 76.5%, respectively. Both standard and the NCCN-IPI showed good prognostication. However, NCCN-IPI more efficiently separated patients of low-intermediate vs. high-intermediate risk compared to standard IPI, and the patients of high risk group according to NCCN-IPI showed poorer OS compared to those according to standard IPI.19 patients had RI according to CKD-EPI formula: 5 patients had pre-existing CKD, 2 had post-renal acute kidney injury (AKI) caused by DLBCL, and another 2 had hypercalcemia and/or hyperuricemia, suggesting AKI due to the electrolyte imbalance due to lymphoma. We could not define the reason of RI of the other 10 patients: they were aged ≥ 70 years (range 71 – 89) except 2 patients with 49 and 69 years, respectively. Patients with RI showed inferior OS compared to those without RI (3-yr OS 26.7% vs. 81.8%, p < 0.001). There was no difference of OS between patients with a GFR of ≥ 90 vs. ≥ 60 - 89 mL/min/1.73 m2 (3-yr OS 82.4% vs. 76.7%, p = 0.436), suggesting that only RI defined by GFR below 60 mL/min/1.73 m2 is a meaningful prognostic indicator of OS. In multivariate analysis, RI was an IPI-independent prognostic biomarker (Table).Among patients with high or high-intermediate risk according to standard IPI, patients with neither anemia of Hb < 10 g/dL nor RI had superior OS vs. patients who had one of them or vs. those with both of them. These findings were maintained when the analysis was restricted to patients with high risk according to standard IPI. Use of NCCN-IPI instead of standard IPI showed same result.
Conclusion
Patients with baseline RI had inferior OS compared to those without RI. Because RI was an independent prognostic factor for OS in multivariate analysis whereas age >60 years (or ≥ 70 or even ≥ 75 years instead) was not, RI might have a role of the biological age-indicator of patients with DLBCL and therefore affect to OS. In combination with Hb < 10 g/dL, RI enhanced prognostication in patients classified as higher risk group according to either standard or NCCN-IPI.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, Prognosis, Renal impairment
Type: Publication Only
Background
Recently the prognostic value of baseline renal impairment (RI) has been evaluated in patients with newly diagnosed cancers: baseline RI assessed by blood urea nitrogen showed significant relationship to overall survival (OS) of patients with advanced non-small cell lung cancer (Zhang et al, Int J Cancer 2015;136:382) or to early mortality among patients with resectable pancreatic adenocarcinoma (Sohal, et al, Cancer 2015;121:1779).
Aims
In this study, we evaluated the prognostic value of baseline RI in patients with diffuse large B-cell lymphoma (DLBCL) uniformly treated with conventional three-weekly rituximab plus cyclophosphamide, adriamycin, vincristine, and prednisolone (R-CHOP21) immunochemotherapy in single institution.
Methods
Patients with newly diagnosed de novo DLBCL treated with ≥ 1 cycle of R-CHOP21 were included. Glomerular filtration rate (GFR) was calculated using serum ceratinine level from pre-treatment serum chemistry data and other clinical information. RI was defined as a GFR of < 60 mL/min/1.73 m2according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.
Results
185 patients treated from Mar. 2006 to Jan. 2015 were included and analyzed. For the median follow up period of 44.1 months (95% CI, 37.5 - 50.7), 53 patients (28.6%) underwent any event and 44 (23.8%) died. 3-year Event-free (EFS) and OS were 71.1% and 76.5%, respectively. Both standard and the NCCN-IPI showed good prognostication. However, NCCN-IPI more efficiently separated patients of low-intermediate vs. high-intermediate risk compared to standard IPI, and the patients of high risk group according to NCCN-IPI showed poorer OS compared to those according to standard IPI.19 patients had RI according to CKD-EPI formula: 5 patients had pre-existing CKD, 2 had post-renal acute kidney injury (AKI) caused by DLBCL, and another 2 had hypercalcemia and/or hyperuricemia, suggesting AKI due to the electrolyte imbalance due to lymphoma. We could not define the reason of RI of the other 10 patients: they were aged ≥ 70 years (range 71 – 89) except 2 patients with 49 and 69 years, respectively. Patients with RI showed inferior OS compared to those without RI (3-yr OS 26.7% vs. 81.8%, p < 0.001). There was no difference of OS between patients with a GFR of ≥ 90 vs. ≥ 60 - 89 mL/min/1.73 m2 (3-yr OS 82.4% vs. 76.7%, p = 0.436), suggesting that only RI defined by GFR below 60 mL/min/1.73 m2 is a meaningful prognostic indicator of OS. In multivariate analysis, RI was an IPI-independent prognostic biomarker (Table).Among patients with high or high-intermediate risk according to standard IPI, patients with neither anemia of Hb < 10 g/dL nor RI had superior OS vs. patients who had one of them or vs. those with both of them. These findings were maintained when the analysis was restricted to patients with high risk according to standard IPI. Use of NCCN-IPI instead of standard IPI showed same result.
Conclusion
Patients with baseline RI had inferior OS compared to those without RI. Because RI was an independent prognostic factor for OS in multivariate analysis whereas age >60 years (or ≥ 70 or even ≥ 75 years instead) was not, RI might have a role of the biological age-indicator of patients with DLBCL and therefore affect to OS. In combination with Hb < 10 g/dL, RI enhanced prognostication in patients classified as higher risk group according to either standard or NCCN-IPI.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, Prognosis, Renal impairment
{{ help_message }}
{{filter}}


