CLINICAL CHARACTERISTICS AND OUTCOME OF PATIENTS WITH PRIMARY MEDIASTINAL LARGE B-CELL LYMPHOMA TREATED WITH INTENSE SHORT-PULSE CHEMOTHERAPY, R-CHOP OR R-DA-EPOCH. A RETROSPECTIVE OBSERVATIONAL STUDY
(Abstract release date: 05/19/16)
EHA Library. Mors K. 06/09/16; 134589; PB1689

Dr. Katja Mors
Contributions
Contributions
Abstract
Abstract: PB1689
Type: Publication Only
Background
Primary mediastinal large B-cell lymphoma (PMBL) is a locally highly aggressive tumour and accounts for approximately 2.4% of adult non-Hodgkin’s lymphoma (NHL). Overall survival rates (OS) between 46 – 79% have been reported but optimal treatment regimens remain to be defined.
Aims
Retrospective, longitudinal assessment of clinical risk factors and outcome of three different treatment regimens for patients with primary mediastinal large B-cell lymphoma.
Methods
We performed a longterm longitudinal retrospective study to analyze the clinical characteristics and the treatment outcome of 63 adult patients with primary mediastinal large B-cell lymphoma in two large hematology departments in Berlin. The study was approved by the Charité Ethic Committee. Between 1996 and 2016 patients were registered at the time of treatment start and data on demographics, clinical features and laboratory parameters were recorded during treatment and follow up. The prognostic impact of IPI-value, pleural or pericardial effusion, LDH, gender and presence of bulky disease was analyzed with univariate analysis with respect to overall survival (OS) and event-free survival (EFS). Survival analyses were performed with the Kaplan-Meyer method and the log-rank test for comparison using SPSSÒ.
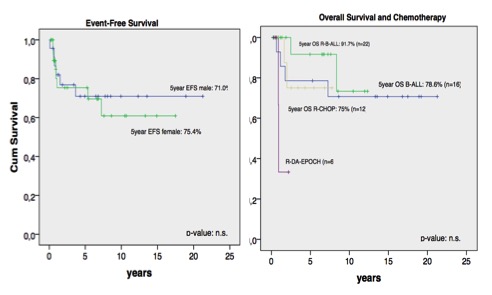
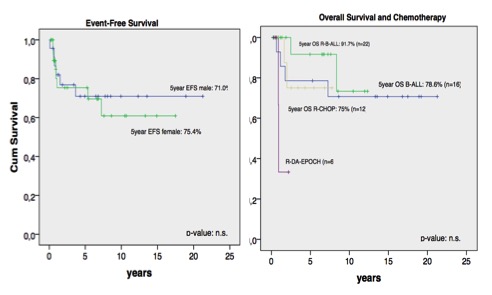
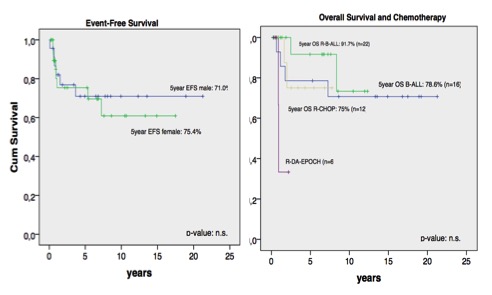
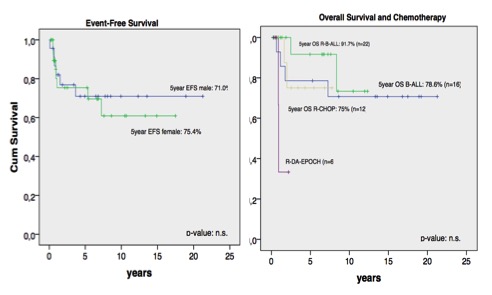
Results
Between 1996 and 2016 37 female patients with a median age of 31 years and 26 male patients with a median age of 36 years were registered. Initial presentation in Ann Arbor stage I: 22%, stage II: 41%, stage III: 9% and stage IV: 28%. B-symptoms: 42%. Bulky disease with a tumor > 10cm was present in 36.2% of all patients. Extranodal manifestations were detected in 30% and either pleural or pericardial effusions was present in 56% of all patients. 16 pts. (26%) were treated according to an intensive short-pulse B-NHL type chemotherapy protocol without Rituximab (B-NHL) and 22 patients (36%) with Rituximab (R-B-NHL), respectively. R-CHOP and R-DA-EPOCH was administered in 12 pts. (20%) and 6 pts. (10%), respectively. 4 pts. received either CHOP without Rituximab or R-ACVBP. Almost all patients received adjuvant involved field radiotherapy after completion of chemotherapy, usually with a total dose of 36 Gy. The probability of event-free survival (pEFS) and OS at 5 years for all patients was 73.5 ± 6.7% and 81.3 ± 6.0%, respectively. For 16 pts. treated with a short-pulse B-NHL type protocol without Rituximab 5-year EFS and OS was 64.3 ± 12.8% and 78.7 ± 11.0%, respectively. With the addition of Rituximab the 5-year EFS and OS (22 pts.) increased with this therapy to 79.4 ± 10.7% and 91.7 ± 8.0%, respectively. Treatment with R-CHOP for 12 pts. led to a 5year EFS and OS of 77.1 ± 14.4% and 75.0 ± 15.3%, respectively. 5-year survival analysis for the 6 pts. treated with R-DA-EPOCH was not calculated due to short follow up (Fig.1). Except for IPI-value there was no significant prognostic impact of pleural or pericardial effusion, LDH, gender or presence of bulky disease.
Conclusion
The addition of Rituximab to the intensive short-pulse B-NHL type chemotherapy protocol led to an improved 5 year EFS and OS. Treatment with R-CHOP seems to be slightly inferior with respect to clinical outcome. We did not find a higher predilection of young female patients and there was no significant prognostic impact of bulky disease, pleural or pericardial effusion, elevated LDH or gender. The best treatment regimen for this rare entity of B-cell lymphoma remains be determined in a randomized multicenter trial.
Session topic: E-poster
Keyword(s): B cell lymphoma, Lymphoma, Therapy
Type: Publication Only
Background
Primary mediastinal large B-cell lymphoma (PMBL) is a locally highly aggressive tumour and accounts for approximately 2.4% of adult non-Hodgkin’s lymphoma (NHL). Overall survival rates (OS) between 46 – 79% have been reported but optimal treatment regimens remain to be defined.
Aims
Retrospective, longitudinal assessment of clinical risk factors and outcome of three different treatment regimens for patients with primary mediastinal large B-cell lymphoma.
Methods
We performed a longterm longitudinal retrospective study to analyze the clinical characteristics and the treatment outcome of 63 adult patients with primary mediastinal large B-cell lymphoma in two large hematology departments in Berlin. The study was approved by the Charité Ethic Committee. Between 1996 and 2016 patients were registered at the time of treatment start and data on demographics, clinical features and laboratory parameters were recorded during treatment and follow up. The prognostic impact of IPI-value, pleural or pericardial effusion, LDH, gender and presence of bulky disease was analyzed with univariate analysis with respect to overall survival (OS) and event-free survival (EFS). Survival analyses were performed with the Kaplan-Meyer method and the log-rank test for comparison using SPSSÒ.
Results
Between 1996 and 2016 37 female patients with a median age of 31 years and 26 male patients with a median age of 36 years were registered. Initial presentation in Ann Arbor stage I: 22%, stage II: 41%, stage III: 9% and stage IV: 28%. B-symptoms: 42%. Bulky disease with a tumor > 10cm was present in 36.2% of all patients. Extranodal manifestations were detected in 30% and either pleural or pericardial effusions was present in 56% of all patients. 16 pts. (26%) were treated according to an intensive short-pulse B-NHL type chemotherapy protocol without Rituximab (B-NHL) and 22 patients (36%) with Rituximab (R-B-NHL), respectively. R-CHOP and R-DA-EPOCH was administered in 12 pts. (20%) and 6 pts. (10%), respectively. 4 pts. received either CHOP without Rituximab or R-ACVBP. Almost all patients received adjuvant involved field radiotherapy after completion of chemotherapy, usually with a total dose of 36 Gy. The probability of event-free survival (pEFS) and OS at 5 years for all patients was 73.5 ± 6.7% and 81.3 ± 6.0%, respectively. For 16 pts. treated with a short-pulse B-NHL type protocol without Rituximab 5-year EFS and OS was 64.3 ± 12.8% and 78.7 ± 11.0%, respectively. With the addition of Rituximab the 5-year EFS and OS (22 pts.) increased with this therapy to 79.4 ± 10.7% and 91.7 ± 8.0%, respectively. Treatment with R-CHOP for 12 pts. led to a 5year EFS and OS of 77.1 ± 14.4% and 75.0 ± 15.3%, respectively. 5-year survival analysis for the 6 pts. treated with R-DA-EPOCH was not calculated due to short follow up (Fig.1). Except for IPI-value there was no significant prognostic impact of pleural or pericardial effusion, LDH, gender or presence of bulky disease.
Conclusion
The addition of Rituximab to the intensive short-pulse B-NHL type chemotherapy protocol led to an improved 5 year EFS and OS. Treatment with R-CHOP seems to be slightly inferior with respect to clinical outcome. We did not find a higher predilection of young female patients and there was no significant prognostic impact of bulky disease, pleural or pericardial effusion, elevated LDH or gender. The best treatment regimen for this rare entity of B-cell lymphoma remains be determined in a randomized multicenter trial.
Session topic: E-poster
Keyword(s): B cell lymphoma, Lymphoma, Therapy
Abstract: PB1689
Type: Publication Only
Background
Primary mediastinal large B-cell lymphoma (PMBL) is a locally highly aggressive tumour and accounts for approximately 2.4% of adult non-Hodgkin’s lymphoma (NHL). Overall survival rates (OS) between 46 – 79% have been reported but optimal treatment regimens remain to be defined.
Aims
Retrospective, longitudinal assessment of clinical risk factors and outcome of three different treatment regimens for patients with primary mediastinal large B-cell lymphoma.
Methods
We performed a longterm longitudinal retrospective study to analyze the clinical characteristics and the treatment outcome of 63 adult patients with primary mediastinal large B-cell lymphoma in two large hematology departments in Berlin. The study was approved by the Charité Ethic Committee. Between 1996 and 2016 patients were registered at the time of treatment start and data on demographics, clinical features and laboratory parameters were recorded during treatment and follow up. The prognostic impact of IPI-value, pleural or pericardial effusion, LDH, gender and presence of bulky disease was analyzed with univariate analysis with respect to overall survival (OS) and event-free survival (EFS). Survival analyses were performed with the Kaplan-Meyer method and the log-rank test for comparison using SPSSÒ.
Results
Between 1996 and 2016 37 female patients with a median age of 31 years and 26 male patients with a median age of 36 years were registered. Initial presentation in Ann Arbor stage I: 22%, stage II: 41%, stage III: 9% and stage IV: 28%. B-symptoms: 42%. Bulky disease with a tumor > 10cm was present in 36.2% of all patients. Extranodal manifestations were detected in 30% and either pleural or pericardial effusions was present in 56% of all patients. 16 pts. (26%) were treated according to an intensive short-pulse B-NHL type chemotherapy protocol without Rituximab (B-NHL) and 22 patients (36%) with Rituximab (R-B-NHL), respectively. R-CHOP and R-DA-EPOCH was administered in 12 pts. (20%) and 6 pts. (10%), respectively. 4 pts. received either CHOP without Rituximab or R-ACVBP. Almost all patients received adjuvant involved field radiotherapy after completion of chemotherapy, usually with a total dose of 36 Gy. The probability of event-free survival (pEFS) and OS at 5 years for all patients was 73.5 ± 6.7% and 81.3 ± 6.0%, respectively. For 16 pts. treated with a short-pulse B-NHL type protocol without Rituximab 5-year EFS and OS was 64.3 ± 12.8% and 78.7 ± 11.0%, respectively. With the addition of Rituximab the 5-year EFS and OS (22 pts.) increased with this therapy to 79.4 ± 10.7% and 91.7 ± 8.0%, respectively. Treatment with R-CHOP for 12 pts. led to a 5year EFS and OS of 77.1 ± 14.4% and 75.0 ± 15.3%, respectively. 5-year survival analysis for the 6 pts. treated with R-DA-EPOCH was not calculated due to short follow up (Fig.1). Except for IPI-value there was no significant prognostic impact of pleural or pericardial effusion, LDH, gender or presence of bulky disease.
Conclusion
The addition of Rituximab to the intensive short-pulse B-NHL type chemotherapy protocol led to an improved 5 year EFS and OS. Treatment with R-CHOP seems to be slightly inferior with respect to clinical outcome. We did not find a higher predilection of young female patients and there was no significant prognostic impact of bulky disease, pleural or pericardial effusion, elevated LDH or gender. The best treatment regimen for this rare entity of B-cell lymphoma remains be determined in a randomized multicenter trial.
Session topic: E-poster
Keyword(s): B cell lymphoma, Lymphoma, Therapy
Type: Publication Only
Background
Primary mediastinal large B-cell lymphoma (PMBL) is a locally highly aggressive tumour and accounts for approximately 2.4% of adult non-Hodgkin’s lymphoma (NHL). Overall survival rates (OS) between 46 – 79% have been reported but optimal treatment regimens remain to be defined.
Aims
Retrospective, longitudinal assessment of clinical risk factors and outcome of three different treatment regimens for patients with primary mediastinal large B-cell lymphoma.
Methods
We performed a longterm longitudinal retrospective study to analyze the clinical characteristics and the treatment outcome of 63 adult patients with primary mediastinal large B-cell lymphoma in two large hematology departments in Berlin. The study was approved by the Charité Ethic Committee. Between 1996 and 2016 patients were registered at the time of treatment start and data on demographics, clinical features and laboratory parameters were recorded during treatment and follow up. The prognostic impact of IPI-value, pleural or pericardial effusion, LDH, gender and presence of bulky disease was analyzed with univariate analysis with respect to overall survival (OS) and event-free survival (EFS). Survival analyses were performed with the Kaplan-Meyer method and the log-rank test for comparison using SPSSÒ.
Results
Between 1996 and 2016 37 female patients with a median age of 31 years and 26 male patients with a median age of 36 years were registered. Initial presentation in Ann Arbor stage I: 22%, stage II: 41%, stage III: 9% and stage IV: 28%. B-symptoms: 42%. Bulky disease with a tumor > 10cm was present in 36.2% of all patients. Extranodal manifestations were detected in 30% and either pleural or pericardial effusions was present in 56% of all patients. 16 pts. (26%) were treated according to an intensive short-pulse B-NHL type chemotherapy protocol without Rituximab (B-NHL) and 22 patients (36%) with Rituximab (R-B-NHL), respectively. R-CHOP and R-DA-EPOCH was administered in 12 pts. (20%) and 6 pts. (10%), respectively. 4 pts. received either CHOP without Rituximab or R-ACVBP. Almost all patients received adjuvant involved field radiotherapy after completion of chemotherapy, usually with a total dose of 36 Gy. The probability of event-free survival (pEFS) and OS at 5 years for all patients was 73.5 ± 6.7% and 81.3 ± 6.0%, respectively. For 16 pts. treated with a short-pulse B-NHL type protocol without Rituximab 5-year EFS and OS was 64.3 ± 12.8% and 78.7 ± 11.0%, respectively. With the addition of Rituximab the 5-year EFS and OS (22 pts.) increased with this therapy to 79.4 ± 10.7% and 91.7 ± 8.0%, respectively. Treatment with R-CHOP for 12 pts. led to a 5year EFS and OS of 77.1 ± 14.4% and 75.0 ± 15.3%, respectively. 5-year survival analysis for the 6 pts. treated with R-DA-EPOCH was not calculated due to short follow up (Fig.1). Except for IPI-value there was no significant prognostic impact of pleural or pericardial effusion, LDH, gender or presence of bulky disease.
Conclusion
The addition of Rituximab to the intensive short-pulse B-NHL type chemotherapy protocol led to an improved 5 year EFS and OS. Treatment with R-CHOP seems to be slightly inferior with respect to clinical outcome. We did not find a higher predilection of young female patients and there was no significant prognostic impact of bulky disease, pleural or pericardial effusion, elevated LDH or gender. The best treatment regimen for this rare entity of B-cell lymphoma remains be determined in a randomized multicenter trial.
Session topic: E-poster
Keyword(s): B cell lymphoma, Lymphoma, Therapy
{{ help_message }}
{{filter}}


