HIGH DOSE THERAPY WITH AUTOLOGOUS STEM CELL TRANSPLANTATION RESULTS IN EXCELLENT LONG TERM SURVIVAL IN PRIMARY MEDIASTINAL B CELL LYMPHOMA
(Abstract release date: 05/19/16)
EHA Library. Struessmann T. 06/09/16; 134578; PB1678

Dr. Tim Struessmann
Contributions
Contributions
Abstract
Abstract: PB1678
Type: Publication Only
Background
Primary mediastinal B cell lymphoma (PMBL) is a rare subtype of diffuse large B cell lymphoma and has some clinical and pathologic features of classical nodular sclerosing Hodgkin lymphoma. Patients are predominantly young women and often present with a locally invasive anterior mediastinal mass. The optimal treatment of PMBL is unknown and differs in clinical practice. Standard immunochemotherapy alone is inadequate and has resulted in routine consolidation with mediastinal radiation. There is only a paucity of prospective data and best results were achieved with rituximab based regimens combined with radiotherapy or dose intensified therapy (DA-EPOCH-R) without radiation. Here we present a single center 10 year retrospective survey indicating that high dose therapy with autologous stem cell support (HDT/ASCT) results in excellent long term outcome.
Aims
Aim of this study is to investigate the infrequent population of PMBL patients, as a single center survey, regarding treatment strategies and long-term outcome.
Methods
All patients with PMBL who presented at Freiburg University Medical Center since 2005 were evaluated according to their baseline characteristics, treatment modality and treatment outcome. From 2005 on patients were treated with upfront HDT/ASCT after R-CHOP induction and R-VCPE (rituximab, epirubicin, etoposide, cisplatin, cyclophosphamide) intensification. Conditioning regimen was BEAM (group A). From 2011 onwards patients were treated with an early intensified protocol: Dense R-MTX/CHOP-14 (6 cycles CHOP-14, dose dense rituximab on days 0, 1, 4, 8, 15, 22, 29, 47, 61 and 75. High-dose MTX was administered on days 30 and 76 right before standard CHOP). Patients who did not achieve a complete metabolic response were intensified as described above (group B). Radiotherapy consolidation was not routinely performed in both treatment groups.
Results
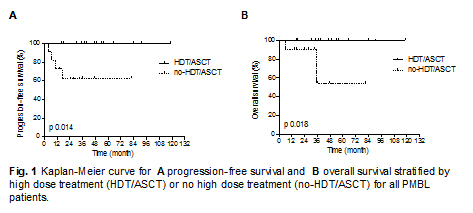
25 patients were identified. Median age was 32 y (range 19-57y), with predominantly females (64%). Disease stage was mostly III/IV (76%). All patients presented with bulky disease and elevated LDH. 36% had an ECOG-Score of ≥2. 72% of patients presented with more than one extranodal site involvement. 88% presented with high-intermediate or high risk aaIPI. Nine patients were intended to receive upfront HDT/ASCT (group A). Of these patients one was primary refractory to R-CHOP-21 and died early in the course of disease. Three patients received consolidating radiotherapy. 2-year PFS and OS were 88.9%, respectively. 14 patients were treated with upfront dense R-MTX/CHOP-14 (group B). Six patients achieved only partial remission and received HDT/ASCT as consolidation. Five patients received additional mediastinal radiotherapy. 2-year PFS and OS were 85.7% and 100%. In addition to both groups, two patients were treated with six cycles of R-CHOP-21 + 2xR (group C). With a median follow-up of 35.9 months estimated 3-year progression-free and overall survival for all patients were 83.2% and 83.6%, respectively. Despite a complete metabolic response after R-MTX/CHOP-14 induction two relapses were observed in this group. One relapse was observed after six cycles R-CHOP-21 and mediastinal radiation. Patients who underwent upfront HDT/ASCT or received HDT/ASCT consolidation in addition to dense R-MTX/CHOP-14 induction had an excellent long-term outcome with a 3-year PFS and OS of 100%, respectively. According HDT/ASCT or no-HDT/ASCT survival curves do significantly differ (Fig. 1). There was no transplant related mortality. No second malignancies were observed yet.
Conclusion
Our results support that dose intensification is necessary in PMBL patients. Regarding the role of HDT/ASCT our data suggest that an approach using upfront HDT/ASCT (group A) or as intensification for patients failing complete metabolic response after induction (group B) is safe and results in excellent long term survival.
Session topic: E-poster
Keyword(s): Autologous peripheral blood stem cell tansplantati, Chemotherapy, Diffuse large B cell lymphoma, Non-Hodgkin's lymphoma
Type: Publication Only
Background
Primary mediastinal B cell lymphoma (PMBL) is a rare subtype of diffuse large B cell lymphoma and has some clinical and pathologic features of classical nodular sclerosing Hodgkin lymphoma. Patients are predominantly young women and often present with a locally invasive anterior mediastinal mass. The optimal treatment of PMBL is unknown and differs in clinical practice. Standard immunochemotherapy alone is inadequate and has resulted in routine consolidation with mediastinal radiation. There is only a paucity of prospective data and best results were achieved with rituximab based regimens combined with radiotherapy or dose intensified therapy (DA-EPOCH-R) without radiation. Here we present a single center 10 year retrospective survey indicating that high dose therapy with autologous stem cell support (HDT/ASCT) results in excellent long term outcome.
Aims
Aim of this study is to investigate the infrequent population of PMBL patients, as a single center survey, regarding treatment strategies and long-term outcome.
Methods
All patients with PMBL who presented at Freiburg University Medical Center since 2005 were evaluated according to their baseline characteristics, treatment modality and treatment outcome. From 2005 on patients were treated with upfront HDT/ASCT after R-CHOP induction and R-VCPE (rituximab, epirubicin, etoposide, cisplatin, cyclophosphamide) intensification. Conditioning regimen was BEAM (group A). From 2011 onwards patients were treated with an early intensified protocol: Dense R-MTX/CHOP-14 (6 cycles CHOP-14, dose dense rituximab on days 0, 1, 4, 8, 15, 22, 29, 47, 61 and 75. High-dose MTX was administered on days 30 and 76 right before standard CHOP). Patients who did not achieve a complete metabolic response were intensified as described above (group B). Radiotherapy consolidation was not routinely performed in both treatment groups.
Results
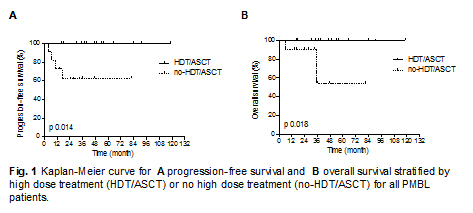
25 patients were identified. Median age was 32 y (range 19-57y), with predominantly females (64%). Disease stage was mostly III/IV (76%). All patients presented with bulky disease and elevated LDH. 36% had an ECOG-Score of ≥2. 72% of patients presented with more than one extranodal site involvement. 88% presented with high-intermediate or high risk aaIPI. Nine patients were intended to receive upfront HDT/ASCT (group A). Of these patients one was primary refractory to R-CHOP-21 and died early in the course of disease. Three patients received consolidating radiotherapy. 2-year PFS and OS were 88.9%, respectively. 14 patients were treated with upfront dense R-MTX/CHOP-14 (group B). Six patients achieved only partial remission and received HDT/ASCT as consolidation. Five patients received additional mediastinal radiotherapy. 2-year PFS and OS were 85.7% and 100%. In addition to both groups, two patients were treated with six cycles of R-CHOP-21 + 2xR (group C). With a median follow-up of 35.9 months estimated 3-year progression-free and overall survival for all patients were 83.2% and 83.6%, respectively. Despite a complete metabolic response after R-MTX/CHOP-14 induction two relapses were observed in this group. One relapse was observed after six cycles R-CHOP-21 and mediastinal radiation. Patients who underwent upfront HDT/ASCT or received HDT/ASCT consolidation in addition to dense R-MTX/CHOP-14 induction had an excellent long-term outcome with a 3-year PFS and OS of 100%, respectively. According HDT/ASCT or no-HDT/ASCT survival curves do significantly differ (Fig. 1). There was no transplant related mortality. No second malignancies were observed yet.
Conclusion
Our results support that dose intensification is necessary in PMBL patients. Regarding the role of HDT/ASCT our data suggest that an approach using upfront HDT/ASCT (group A) or as intensification for patients failing complete metabolic response after induction (group B) is safe and results in excellent long term survival.
Session topic: E-poster
Keyword(s): Autologous peripheral blood stem cell tansplantati, Chemotherapy, Diffuse large B cell lymphoma, Non-Hodgkin's lymphoma
Abstract: PB1678
Type: Publication Only
Background
Primary mediastinal B cell lymphoma (PMBL) is a rare subtype of diffuse large B cell lymphoma and has some clinical and pathologic features of classical nodular sclerosing Hodgkin lymphoma. Patients are predominantly young women and often present with a locally invasive anterior mediastinal mass. The optimal treatment of PMBL is unknown and differs in clinical practice. Standard immunochemotherapy alone is inadequate and has resulted in routine consolidation with mediastinal radiation. There is only a paucity of prospective data and best results were achieved with rituximab based regimens combined with radiotherapy or dose intensified therapy (DA-EPOCH-R) without radiation. Here we present a single center 10 year retrospective survey indicating that high dose therapy with autologous stem cell support (HDT/ASCT) results in excellent long term outcome.
Aims
Aim of this study is to investigate the infrequent population of PMBL patients, as a single center survey, regarding treatment strategies and long-term outcome.
Methods
All patients with PMBL who presented at Freiburg University Medical Center since 2005 were evaluated according to their baseline characteristics, treatment modality and treatment outcome. From 2005 on patients were treated with upfront HDT/ASCT after R-CHOP induction and R-VCPE (rituximab, epirubicin, etoposide, cisplatin, cyclophosphamide) intensification. Conditioning regimen was BEAM (group A). From 2011 onwards patients were treated with an early intensified protocol: Dense R-MTX/CHOP-14 (6 cycles CHOP-14, dose dense rituximab on days 0, 1, 4, 8, 15, 22, 29, 47, 61 and 75. High-dose MTX was administered on days 30 and 76 right before standard CHOP). Patients who did not achieve a complete metabolic response were intensified as described above (group B). Radiotherapy consolidation was not routinely performed in both treatment groups.
Results
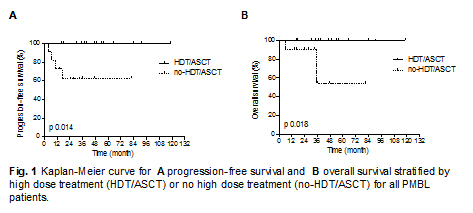
25 patients were identified. Median age was 32 y (range 19-57y), with predominantly females (64%). Disease stage was mostly III/IV (76%). All patients presented with bulky disease and elevated LDH. 36% had an ECOG-Score of ≥2. 72% of patients presented with more than one extranodal site involvement. 88% presented with high-intermediate or high risk aaIPI. Nine patients were intended to receive upfront HDT/ASCT (group A). Of these patients one was primary refractory to R-CHOP-21 and died early in the course of disease. Three patients received consolidating radiotherapy. 2-year PFS and OS were 88.9%, respectively. 14 patients were treated with upfront dense R-MTX/CHOP-14 (group B). Six patients achieved only partial remission and received HDT/ASCT as consolidation. Five patients received additional mediastinal radiotherapy. 2-year PFS and OS were 85.7% and 100%. In addition to both groups, two patients were treated with six cycles of R-CHOP-21 + 2xR (group C). With a median follow-up of 35.9 months estimated 3-year progression-free and overall survival for all patients were 83.2% and 83.6%, respectively. Despite a complete metabolic response after R-MTX/CHOP-14 induction two relapses were observed in this group. One relapse was observed after six cycles R-CHOP-21 and mediastinal radiation. Patients who underwent upfront HDT/ASCT or received HDT/ASCT consolidation in addition to dense R-MTX/CHOP-14 induction had an excellent long-term outcome with a 3-year PFS and OS of 100%, respectively. According HDT/ASCT or no-HDT/ASCT survival curves do significantly differ (Fig. 1). There was no transplant related mortality. No second malignancies were observed yet.
Conclusion
Our results support that dose intensification is necessary in PMBL patients. Regarding the role of HDT/ASCT our data suggest that an approach using upfront HDT/ASCT (group A) or as intensification for patients failing complete metabolic response after induction (group B) is safe and results in excellent long term survival.
Session topic: E-poster
Keyword(s): Autologous peripheral blood stem cell tansplantati, Chemotherapy, Diffuse large B cell lymphoma, Non-Hodgkin's lymphoma
Type: Publication Only
Background
Primary mediastinal B cell lymphoma (PMBL) is a rare subtype of diffuse large B cell lymphoma and has some clinical and pathologic features of classical nodular sclerosing Hodgkin lymphoma. Patients are predominantly young women and often present with a locally invasive anterior mediastinal mass. The optimal treatment of PMBL is unknown and differs in clinical practice. Standard immunochemotherapy alone is inadequate and has resulted in routine consolidation with mediastinal radiation. There is only a paucity of prospective data and best results were achieved with rituximab based regimens combined with radiotherapy or dose intensified therapy (DA-EPOCH-R) without radiation. Here we present a single center 10 year retrospective survey indicating that high dose therapy with autologous stem cell support (HDT/ASCT) results in excellent long term outcome.
Aims
Aim of this study is to investigate the infrequent population of PMBL patients, as a single center survey, regarding treatment strategies and long-term outcome.
Methods
All patients with PMBL who presented at Freiburg University Medical Center since 2005 were evaluated according to their baseline characteristics, treatment modality and treatment outcome. From 2005 on patients were treated with upfront HDT/ASCT after R-CHOP induction and R-VCPE (rituximab, epirubicin, etoposide, cisplatin, cyclophosphamide) intensification. Conditioning regimen was BEAM (group A). From 2011 onwards patients were treated with an early intensified protocol: Dense R-MTX/CHOP-14 (6 cycles CHOP-14, dose dense rituximab on days 0, 1, 4, 8, 15, 22, 29, 47, 61 and 75. High-dose MTX was administered on days 30 and 76 right before standard CHOP). Patients who did not achieve a complete metabolic response were intensified as described above (group B). Radiotherapy consolidation was not routinely performed in both treatment groups.
Results
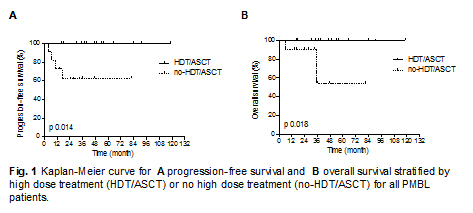
25 patients were identified. Median age was 32 y (range 19-57y), with predominantly females (64%). Disease stage was mostly III/IV (76%). All patients presented with bulky disease and elevated LDH. 36% had an ECOG-Score of ≥2. 72% of patients presented with more than one extranodal site involvement. 88% presented with high-intermediate or high risk aaIPI. Nine patients were intended to receive upfront HDT/ASCT (group A). Of these patients one was primary refractory to R-CHOP-21 and died early in the course of disease. Three patients received consolidating radiotherapy. 2-year PFS and OS were 88.9%, respectively. 14 patients were treated with upfront dense R-MTX/CHOP-14 (group B). Six patients achieved only partial remission and received HDT/ASCT as consolidation. Five patients received additional mediastinal radiotherapy. 2-year PFS and OS were 85.7% and 100%. In addition to both groups, two patients were treated with six cycles of R-CHOP-21 + 2xR (group C). With a median follow-up of 35.9 months estimated 3-year progression-free and overall survival for all patients were 83.2% and 83.6%, respectively. Despite a complete metabolic response after R-MTX/CHOP-14 induction two relapses were observed in this group. One relapse was observed after six cycles R-CHOP-21 and mediastinal radiation. Patients who underwent upfront HDT/ASCT or received HDT/ASCT consolidation in addition to dense R-MTX/CHOP-14 induction had an excellent long-term outcome with a 3-year PFS and OS of 100%, respectively. According HDT/ASCT or no-HDT/ASCT survival curves do significantly differ (Fig. 1). There was no transplant related mortality. No second malignancies were observed yet.
Conclusion
Our results support that dose intensification is necessary in PMBL patients. Regarding the role of HDT/ASCT our data suggest that an approach using upfront HDT/ASCT (group A) or as intensification for patients failing complete metabolic response after induction (group B) is safe and results in excellent long term survival.
Session topic: E-poster
Keyword(s): Autologous peripheral blood stem cell tansplantati, Chemotherapy, Diffuse large B cell lymphoma, Non-Hodgkin's lymphoma
{{ help_message }}
{{filter}}


