IMPACT OF GRANULOCYTE COLONY STIMULATING FACTOR FOR OUTCOMES OF NON-M3 AML PATIENTS TREATED WITH ANTHRACYCLINE-BASED INDUCTION (7+3 REGIMEN) CHEMOTHERAPIES
(Abstract release date: 05/19/16)
EHA Library. Kang K. 06/09/16; 134565; PB1665

Ms. Ka-Won Kang
Contributions
Contributions
Abstract
Abstract: PB1665
Type: Publication Only
Background
Currently most guidelines recommend primary granulocyte colony-stimulating factor (G-CSF) prophylaxis in patients with solid cancer who have an approximately 20% or higher risk for febrile neutropenia. However, these recommendations are not as clear for patients with acute myelogenous leukemia (AML).
Aims
To identify the role of G-CSF in induction treatment in patients with newly diagnosed AML, we analyzed the efficacies of administration based on clinical situations such as the development of neutropenia or fever, and investigated the impact of G-CSF exposure on the anti-leukemic efficacies of induction chemotherapy.
Methods
A total of 285 patients enrolled in the Korea University AML registry from September 2001 to March 2015 were analyzed and classified based on G-CSF administration: (1) no G-CSF exposure during induction (no G-CSF group), (2) administration initiated immediately after the development of neutropenia (absolute neutrophil counts, <1000/μL) but before the development of febrile neutropenia (preemptive group), and (3) administration initiated after the development of febrile neutropenia (therapeutic group).
Results
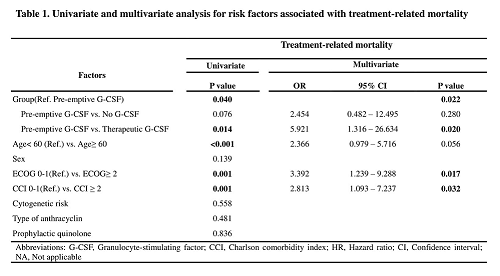
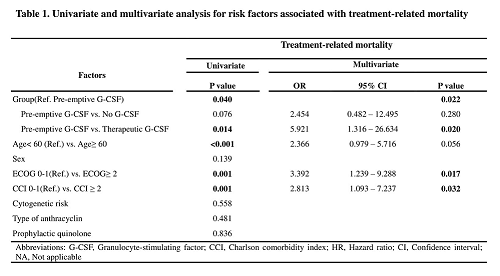
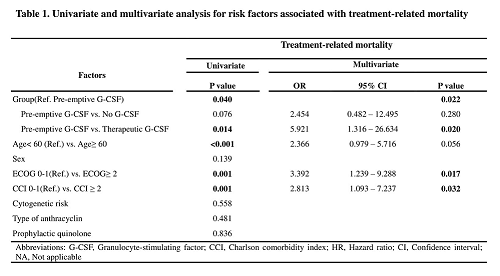
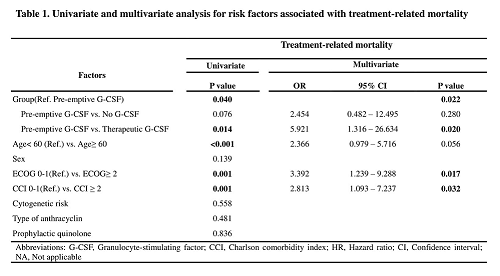
G-CSF administration resulted in faster ANC recovery compared to that in the no G-CSF group (p < 0.001), but did not significantly affect the duration of neutropenia or chemotherapy-induced febrile neutropenia (CIFN) in both the preemptive and therapeutic group. In treatment-related mortality (TRM) multivariate analysis, the therapeutic group had higher TRM than the preemptive group (OR 5.921, 95% confidence interval 1.316–26.634, p = 0.020), with no significant difference between the preemptive and no G-CSF groups (OR 2.454, 95% CI 0.482-12.495, p = 0.280). Only quinolone prophylaxis was shown to be effective in reducing the incidence of CIFN (p = 0.001). There were no significant differences in remission rate, cumulative incidence of relapse, overall survival, and relapse-free survival among the groups.
Conclusion
G-CSF administration during induction chemotherapy in non-M3 AML patients can accelerate neutrophil recovery without affecting treatment outcomes. It is best administered at least before the development of febrile neutropenia in order to prevent TRM. Quinolone prophylaxis might be effective in reducing CIFN.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Granulocyte colony-stimulating factor (G-CSF), Neutropenia, Treatment-related mortality
Type: Publication Only
Background
Currently most guidelines recommend primary granulocyte colony-stimulating factor (G-CSF) prophylaxis in patients with solid cancer who have an approximately 20% or higher risk for febrile neutropenia. However, these recommendations are not as clear for patients with acute myelogenous leukemia (AML).
Aims
To identify the role of G-CSF in induction treatment in patients with newly diagnosed AML, we analyzed the efficacies of administration based on clinical situations such as the development of neutropenia or fever, and investigated the impact of G-CSF exposure on the anti-leukemic efficacies of induction chemotherapy.
Methods
A total of 285 patients enrolled in the Korea University AML registry from September 2001 to March 2015 were analyzed and classified based on G-CSF administration: (1) no G-CSF exposure during induction (no G-CSF group), (2) administration initiated immediately after the development of neutropenia (absolute neutrophil counts, <1000/μL) but before the development of febrile neutropenia (preemptive group), and (3) administration initiated after the development of febrile neutropenia (therapeutic group).
Results
G-CSF administration resulted in faster ANC recovery compared to that in the no G-CSF group (p < 0.001), but did not significantly affect the duration of neutropenia or chemotherapy-induced febrile neutropenia (CIFN) in both the preemptive and therapeutic group. In treatment-related mortality (TRM) multivariate analysis, the therapeutic group had higher TRM than the preemptive group (OR 5.921, 95% confidence interval 1.316–26.634, p = 0.020), with no significant difference between the preemptive and no G-CSF groups (OR 2.454, 95% CI 0.482-12.495, p = 0.280). Only quinolone prophylaxis was shown to be effective in reducing the incidence of CIFN (p = 0.001). There were no significant differences in remission rate, cumulative incidence of relapse, overall survival, and relapse-free survival among the groups.
Conclusion
G-CSF administration during induction chemotherapy in non-M3 AML patients can accelerate neutrophil recovery without affecting treatment outcomes. It is best administered at least before the development of febrile neutropenia in order to prevent TRM. Quinolone prophylaxis might be effective in reducing CIFN.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Granulocyte colony-stimulating factor (G-CSF), Neutropenia, Treatment-related mortality
Abstract: PB1665
Type: Publication Only
Background
Currently most guidelines recommend primary granulocyte colony-stimulating factor (G-CSF) prophylaxis in patients with solid cancer who have an approximately 20% or higher risk for febrile neutropenia. However, these recommendations are not as clear for patients with acute myelogenous leukemia (AML).
Aims
To identify the role of G-CSF in induction treatment in patients with newly diagnosed AML, we analyzed the efficacies of administration based on clinical situations such as the development of neutropenia or fever, and investigated the impact of G-CSF exposure on the anti-leukemic efficacies of induction chemotherapy.
Methods
A total of 285 patients enrolled in the Korea University AML registry from September 2001 to March 2015 were analyzed and classified based on G-CSF administration: (1) no G-CSF exposure during induction (no G-CSF group), (2) administration initiated immediately after the development of neutropenia (absolute neutrophil counts, <1000/μL) but before the development of febrile neutropenia (preemptive group), and (3) administration initiated after the development of febrile neutropenia (therapeutic group).
Results
G-CSF administration resulted in faster ANC recovery compared to that in the no G-CSF group (p < 0.001), but did not significantly affect the duration of neutropenia or chemotherapy-induced febrile neutropenia (CIFN) in both the preemptive and therapeutic group. In treatment-related mortality (TRM) multivariate analysis, the therapeutic group had higher TRM than the preemptive group (OR 5.921, 95% confidence interval 1.316–26.634, p = 0.020), with no significant difference between the preemptive and no G-CSF groups (OR 2.454, 95% CI 0.482-12.495, p = 0.280). Only quinolone prophylaxis was shown to be effective in reducing the incidence of CIFN (p = 0.001). There were no significant differences in remission rate, cumulative incidence of relapse, overall survival, and relapse-free survival among the groups.
Conclusion
G-CSF administration during induction chemotherapy in non-M3 AML patients can accelerate neutrophil recovery without affecting treatment outcomes. It is best administered at least before the development of febrile neutropenia in order to prevent TRM. Quinolone prophylaxis might be effective in reducing CIFN.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Granulocyte colony-stimulating factor (G-CSF), Neutropenia, Treatment-related mortality
Type: Publication Only
Background
Currently most guidelines recommend primary granulocyte colony-stimulating factor (G-CSF) prophylaxis in patients with solid cancer who have an approximately 20% or higher risk for febrile neutropenia. However, these recommendations are not as clear for patients with acute myelogenous leukemia (AML).
Aims
To identify the role of G-CSF in induction treatment in patients with newly diagnosed AML, we analyzed the efficacies of administration based on clinical situations such as the development of neutropenia or fever, and investigated the impact of G-CSF exposure on the anti-leukemic efficacies of induction chemotherapy.
Methods
A total of 285 patients enrolled in the Korea University AML registry from September 2001 to March 2015 were analyzed and classified based on G-CSF administration: (1) no G-CSF exposure during induction (no G-CSF group), (2) administration initiated immediately after the development of neutropenia (absolute neutrophil counts, <1000/μL) but before the development of febrile neutropenia (preemptive group), and (3) administration initiated after the development of febrile neutropenia (therapeutic group).
Results
G-CSF administration resulted in faster ANC recovery compared to that in the no G-CSF group (p < 0.001), but did not significantly affect the duration of neutropenia or chemotherapy-induced febrile neutropenia (CIFN) in both the preemptive and therapeutic group. In treatment-related mortality (TRM) multivariate analysis, the therapeutic group had higher TRM than the preemptive group (OR 5.921, 95% confidence interval 1.316–26.634, p = 0.020), with no significant difference between the preemptive and no G-CSF groups (OR 2.454, 95% CI 0.482-12.495, p = 0.280). Only quinolone prophylaxis was shown to be effective in reducing the incidence of CIFN (p = 0.001). There were no significant differences in remission rate, cumulative incidence of relapse, overall survival, and relapse-free survival among the groups.
Conclusion
G-CSF administration during induction chemotherapy in non-M3 AML patients can accelerate neutrophil recovery without affecting treatment outcomes. It is best administered at least before the development of febrile neutropenia in order to prevent TRM. Quinolone prophylaxis might be effective in reducing CIFN.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Granulocyte colony-stimulating factor (G-CSF), Neutropenia, Treatment-related mortality
{{ help_message }}
{{filter}}


