HIGH FREQUENCY OF OCCULT CENTRAL NERVOUS SYSTEM INVOLVEMENT IN BLASTIC PLASMACYTOID DENDRITIC CELL NEOPLASM AT DIAGNOSIS: ROLE FOR INTRATHECAL PROPHYLAXIS?
(Abstract release date: 05/19/16)
EHA Library. Martin L. 06/09/16; 134555; PB1655

Ms. Lourdes Martin
Contributions
Contributions
Abstract
Abstract: PB1655
Type: Publication Only
Background
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare aggressive myeloid neoplasm which shows a high rate of central nervous system (CNS) recurrence (≈30%) and a short overall survival (OS), usually <1 year. Despite this, screening for CNS involvement is not routinely performed at diagnosis and intrathecal (IT) prophylaxis is not regularly administered in BPDCN patients.
Aims
To analyse the incidence of CNS involvement in BPDCN patients at diagnosis and to evaluate the potential benefit of intrathecal prophylaxis administration.
Methods
Forty-one stabilized cerebrospinal fluid (CSF) samples from 13 consecutive BPDCN patients were evaluated for the presence of CNS involvement by next generation flow cytometry immunophenotypic studies. Cases were evaluated at diagnosis (n=10) or at relapse (n=3) and subsequently, after IT therapy. The 10 patients studied at diagnosis received high-risk acute lymphoblastic leukaemia (ALL)-type treatment, including one dose of triple intrathecal therapy (TIT), as CNS prophylaxis at each treatment phase. For CSF-positive cases, additional IT treatment was given until two consecutive CSF-negative samples were obtained. In order to validate the impact of CNS involvement and CNS-directed therapy on patient outcome, an independent validation cohort of 23 BPDCN was retrospectively analysed. Informed consent was obtained from all patients.
Results
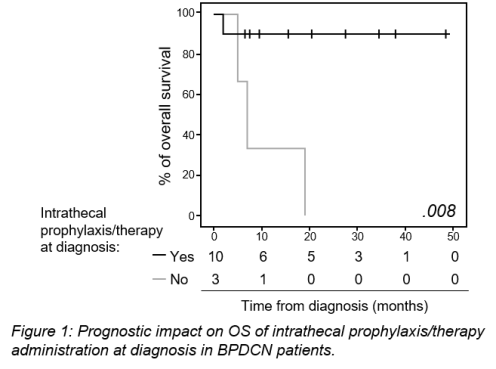
Despite none of the patients presented with neurological symptoms at disease staging, occult CNS involvement was detected in 6/10 cases evaluated at diagnosis and 3/3 studied at relapse/progression. Detection of tumour cells in CSF at diagnosis was associated with a ≥20% bone marrow infiltration by tumour cells. BPDCN patients evaluated at diagnosis received IT treatment -either CNS prophylaxis (n=4) or active therapy (n=6)- and all but one remain alive (median follow-up of 20 months). In contrast, all three patients assessed at relapse/progression died (Fig. 1). Follow-up CSF samples obtained after TIT showed absence of tumour cells in 6/6 CSF+ cases studied at diagnosis, either after one -5/6 cases- or 4 doses of therapy (6/6 cases). The potential benefit of IT treatment administered early at diagnosis on OS and CNS recurrence-free survival (RFS) of BPDCN was further confirmed in a retrospective cohort of another 23 BPDCN patients. Univariate analysis of prognostic factors performed in the whole patient cohort (n=36) showed a favourable impact on CNS-RFS and/or OS for children, patients receiving ALL-type therapy, allogeneic hematopoietic stem cell transplant and IT prophylaxis/treatment at diagnosis, the later variable emerging as the only independent (favourable) prognostic factor for CNS-RFS (p=.02, hazard ratio [HR]=11.2, 95% confidence interval [CI]: 1.4 – 88.8) and OS (p=.001, HR=7.6, 95% CI: 2.2 – 25.9).
Conclusion
Our findings show that BPDCN patients studied at diagnosis frequently display occult CNS involvement; moreover, these data also indicate that treatment of occult CNS disease might lead to an improved outcome for BPDCN. These results suggest that the CNS could be a persistent blast-cell sanctuary in BPDCN patients with leukemic presentation, due to the limited power of cytostatic drugs to cross the blood-brain barrier into the CSF and brain parenchyma. This reservoir of leukemic cells may also contribute to the high rate of bone marrow/systemic disease recurrence observed in these patients.
Session topic: E-poster
Keyword(s): Acute leukemia, CNS, Cytometry, Prophylaxis
Type: Publication Only
Background
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare aggressive myeloid neoplasm which shows a high rate of central nervous system (CNS) recurrence (≈30%) and a short overall survival (OS), usually <1 year. Despite this, screening for CNS involvement is not routinely performed at diagnosis and intrathecal (IT) prophylaxis is not regularly administered in BPDCN patients.
Aims
To analyse the incidence of CNS involvement in BPDCN patients at diagnosis and to evaluate the potential benefit of intrathecal prophylaxis administration.
Methods
Forty-one stabilized cerebrospinal fluid (CSF) samples from 13 consecutive BPDCN patients were evaluated for the presence of CNS involvement by next generation flow cytometry immunophenotypic studies. Cases were evaluated at diagnosis (n=10) or at relapse (n=3) and subsequently, after IT therapy. The 10 patients studied at diagnosis received high-risk acute lymphoblastic leukaemia (ALL)-type treatment, including one dose of triple intrathecal therapy (TIT), as CNS prophylaxis at each treatment phase. For CSF-positive cases, additional IT treatment was given until two consecutive CSF-negative samples were obtained. In order to validate the impact of CNS involvement and CNS-directed therapy on patient outcome, an independent validation cohort of 23 BPDCN was retrospectively analysed. Informed consent was obtained from all patients.
Results
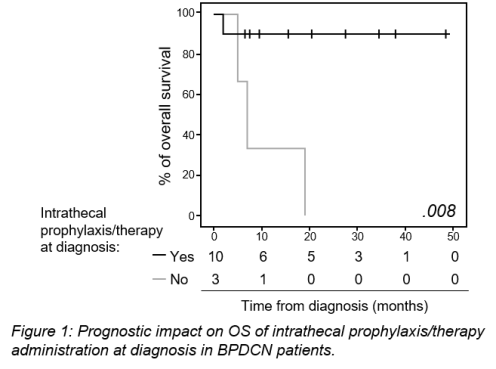
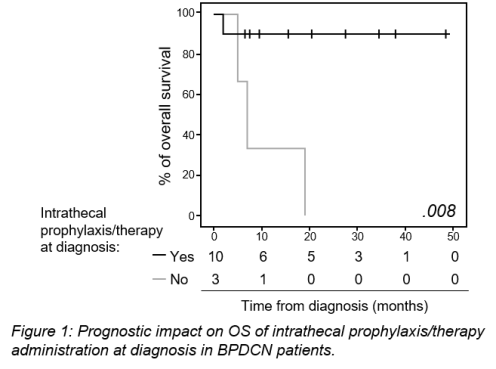
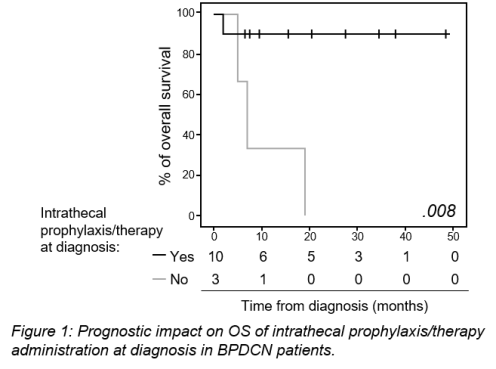
Despite none of the patients presented with neurological symptoms at disease staging, occult CNS involvement was detected in 6/10 cases evaluated at diagnosis and 3/3 studied at relapse/progression. Detection of tumour cells in CSF at diagnosis was associated with a ≥20% bone marrow infiltration by tumour cells. BPDCN patients evaluated at diagnosis received IT treatment -either CNS prophylaxis (n=4) or active therapy (n=6)- and all but one remain alive (median follow-up of 20 months). In contrast, all three patients assessed at relapse/progression died (Fig. 1). Follow-up CSF samples obtained after TIT showed absence of tumour cells in 6/6 CSF+ cases studied at diagnosis, either after one -5/6 cases- or 4 doses of therapy (6/6 cases). The potential benefit of IT treatment administered early at diagnosis on OS and CNS recurrence-free survival (RFS) of BPDCN was further confirmed in a retrospective cohort of another 23 BPDCN patients. Univariate analysis of prognostic factors performed in the whole patient cohort (n=36) showed a favourable impact on CNS-RFS and/or OS for children, patients receiving ALL-type therapy, allogeneic hematopoietic stem cell transplant and IT prophylaxis/treatment at diagnosis, the later variable emerging as the only independent (favourable) prognostic factor for CNS-RFS (p=.02, hazard ratio [HR]=11.2, 95% confidence interval [CI]: 1.4 – 88.8) and OS (p=.001, HR=7.6, 95% CI: 2.2 – 25.9).
Conclusion
Our findings show that BPDCN patients studied at diagnosis frequently display occult CNS involvement; moreover, these data also indicate that treatment of occult CNS disease might lead to an improved outcome for BPDCN. These results suggest that the CNS could be a persistent blast-cell sanctuary in BPDCN patients with leukemic presentation, due to the limited power of cytostatic drugs to cross the blood-brain barrier into the CSF and brain parenchyma. This reservoir of leukemic cells may also contribute to the high rate of bone marrow/systemic disease recurrence observed in these patients.
Session topic: E-poster
Keyword(s): Acute leukemia, CNS, Cytometry, Prophylaxis
Abstract: PB1655
Type: Publication Only
Background
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare aggressive myeloid neoplasm which shows a high rate of central nervous system (CNS) recurrence (≈30%) and a short overall survival (OS), usually <1 year. Despite this, screening for CNS involvement is not routinely performed at diagnosis and intrathecal (IT) prophylaxis is not regularly administered in BPDCN patients.
Aims
To analyse the incidence of CNS involvement in BPDCN patients at diagnosis and to evaluate the potential benefit of intrathecal prophylaxis administration.
Methods
Forty-one stabilized cerebrospinal fluid (CSF) samples from 13 consecutive BPDCN patients were evaluated for the presence of CNS involvement by next generation flow cytometry immunophenotypic studies. Cases were evaluated at diagnosis (n=10) or at relapse (n=3) and subsequently, after IT therapy. The 10 patients studied at diagnosis received high-risk acute lymphoblastic leukaemia (ALL)-type treatment, including one dose of triple intrathecal therapy (TIT), as CNS prophylaxis at each treatment phase. For CSF-positive cases, additional IT treatment was given until two consecutive CSF-negative samples were obtained. In order to validate the impact of CNS involvement and CNS-directed therapy on patient outcome, an independent validation cohort of 23 BPDCN was retrospectively analysed. Informed consent was obtained from all patients.
Results
Despite none of the patients presented with neurological symptoms at disease staging, occult CNS involvement was detected in 6/10 cases evaluated at diagnosis and 3/3 studied at relapse/progression. Detection of tumour cells in CSF at diagnosis was associated with a ≥20% bone marrow infiltration by tumour cells. BPDCN patients evaluated at diagnosis received IT treatment -either CNS prophylaxis (n=4) or active therapy (n=6)- and all but one remain alive (median follow-up of 20 months). In contrast, all three patients assessed at relapse/progression died (Fig. 1). Follow-up CSF samples obtained after TIT showed absence of tumour cells in 6/6 CSF+ cases studied at diagnosis, either after one -5/6 cases- or 4 doses of therapy (6/6 cases). The potential benefit of IT treatment administered early at diagnosis on OS and CNS recurrence-free survival (RFS) of BPDCN was further confirmed in a retrospective cohort of another 23 BPDCN patients. Univariate analysis of prognostic factors performed in the whole patient cohort (n=36) showed a favourable impact on CNS-RFS and/or OS for children, patients receiving ALL-type therapy, allogeneic hematopoietic stem cell transplant and IT prophylaxis/treatment at diagnosis, the later variable emerging as the only independent (favourable) prognostic factor for CNS-RFS (p=.02, hazard ratio [HR]=11.2, 95% confidence interval [CI]: 1.4 – 88.8) and OS (p=.001, HR=7.6, 95% CI: 2.2 – 25.9).
Conclusion
Our findings show that BPDCN patients studied at diagnosis frequently display occult CNS involvement; moreover, these data also indicate that treatment of occult CNS disease might lead to an improved outcome for BPDCN. These results suggest that the CNS could be a persistent blast-cell sanctuary in BPDCN patients with leukemic presentation, due to the limited power of cytostatic drugs to cross the blood-brain barrier into the CSF and brain parenchyma. This reservoir of leukemic cells may also contribute to the high rate of bone marrow/systemic disease recurrence observed in these patients.
Session topic: E-poster
Keyword(s): Acute leukemia, CNS, Cytometry, Prophylaxis
Type: Publication Only
Background
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare aggressive myeloid neoplasm which shows a high rate of central nervous system (CNS) recurrence (≈30%) and a short overall survival (OS), usually <1 year. Despite this, screening for CNS involvement is not routinely performed at diagnosis and intrathecal (IT) prophylaxis is not regularly administered in BPDCN patients.
Aims
To analyse the incidence of CNS involvement in BPDCN patients at diagnosis and to evaluate the potential benefit of intrathecal prophylaxis administration.
Methods
Forty-one stabilized cerebrospinal fluid (CSF) samples from 13 consecutive BPDCN patients were evaluated for the presence of CNS involvement by next generation flow cytometry immunophenotypic studies. Cases were evaluated at diagnosis (n=10) or at relapse (n=3) and subsequently, after IT therapy. The 10 patients studied at diagnosis received high-risk acute lymphoblastic leukaemia (ALL)-type treatment, including one dose of triple intrathecal therapy (TIT), as CNS prophylaxis at each treatment phase. For CSF-positive cases, additional IT treatment was given until two consecutive CSF-negative samples were obtained. In order to validate the impact of CNS involvement and CNS-directed therapy on patient outcome, an independent validation cohort of 23 BPDCN was retrospectively analysed. Informed consent was obtained from all patients.
Results
Despite none of the patients presented with neurological symptoms at disease staging, occult CNS involvement was detected in 6/10 cases evaluated at diagnosis and 3/3 studied at relapse/progression. Detection of tumour cells in CSF at diagnosis was associated with a ≥20% bone marrow infiltration by tumour cells. BPDCN patients evaluated at diagnosis received IT treatment -either CNS prophylaxis (n=4) or active therapy (n=6)- and all but one remain alive (median follow-up of 20 months). In contrast, all three patients assessed at relapse/progression died (Fig. 1). Follow-up CSF samples obtained after TIT showed absence of tumour cells in 6/6 CSF+ cases studied at diagnosis, either after one -5/6 cases- or 4 doses of therapy (6/6 cases). The potential benefit of IT treatment administered early at diagnosis on OS and CNS recurrence-free survival (RFS) of BPDCN was further confirmed in a retrospective cohort of another 23 BPDCN patients. Univariate analysis of prognostic factors performed in the whole patient cohort (n=36) showed a favourable impact on CNS-RFS and/or OS for children, patients receiving ALL-type therapy, allogeneic hematopoietic stem cell transplant and IT prophylaxis/treatment at diagnosis, the later variable emerging as the only independent (favourable) prognostic factor for CNS-RFS (p=.02, hazard ratio [HR]=11.2, 95% confidence interval [CI]: 1.4 – 88.8) and OS (p=.001, HR=7.6, 95% CI: 2.2 – 25.9).
Conclusion
Our findings show that BPDCN patients studied at diagnosis frequently display occult CNS involvement; moreover, these data also indicate that treatment of occult CNS disease might lead to an improved outcome for BPDCN. These results suggest that the CNS could be a persistent blast-cell sanctuary in BPDCN patients with leukemic presentation, due to the limited power of cytostatic drugs to cross the blood-brain barrier into the CSF and brain parenchyma. This reservoir of leukemic cells may also contribute to the high rate of bone marrow/systemic disease recurrence observed in these patients.
Session topic: E-poster
Keyword(s): Acute leukemia, CNS, Cytometry, Prophylaxis
{{ help_message }}
{{filter}}


