INCREASED RISK OF TUBERCULOSIS IN PATIENTS WITH ACUTE MYELOID LEUKEMIA IN AN ENDEMIC AREA: A NATIONWIDE POPULATION-BASED STUDY
(Abstract release date: 05/19/16)
EHA Library. Liu C. 06/09/16; 134552; PB1652

Dr. Chia-Jen Liu
Contributions
Contributions
Abstract
Abstract: PB1652
Type: Publication Only
Background
To date, few studies have investigated the association between tuberculosis (TB) and acute myeloid leukemia (AML).
Aims
We therefore aim to assess the impact and the risk factors of TB in patients with AML for a better risk stratification strategy.
Methods
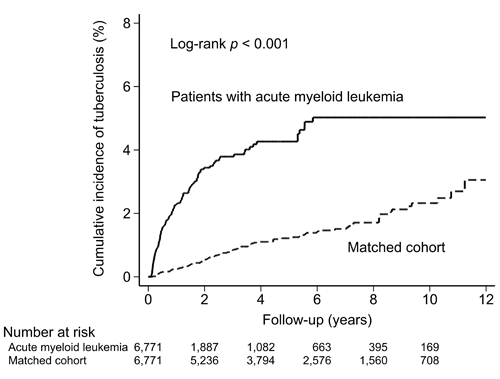
We conducted a nationwide population-based study using data retrieved from Taiwan’s National Health Insurance Research Database to determine the incidence of TB and to analyze the risk factors for TB in patients with newly diagnosed AML. From 2000 to 2011, we identified 6,771 AML patients and the same number of subjects without AML matched for sex, age, and comorbidities. Cox proportional hazards models were applied for further analysis. AML-related therapies were assessed as time-dependent covariates to avoid immortal time bias.
Results
Compared with the matched cohort, AML patients exhibited a higher risk for TB (adjusted hazard ratio [HR] 4.31, 95% confidence interval [CI] 3.27–5.67, p < 0.001), with an increased risk for both pulmonary (adjusted HR 4.22, 95% CI 3.13–5.69, p < 0·001) and extrapulmonary (adjusted HR 4.86, 95% CI 2.40–9.84, p < 0.001) TB. Adjusted HRs of TB occurrence for follow-up periods of < 1, 1–2, 2–5, and ≥ 5 years were 9.61 (95% CI 5.69–16.25), 5.40 (95% CI 2.88–10.13), 1.89 (95% CI 0.94–3.79), and 1.81 (95% CI 0.71–4.63), respectively. Multivariate analysis showed that being male (adjusted HR 1.47, 95% CI 1.06–2.04, p = 0.020) and having liver cirrhosis (adjusted HR 2.08, 95% CI 1.17–3.70, p = 0.012) were identified as independent risk factors for developing TB in AML patients. However, treatment with idarubicin, daunorubicin, high-dose cytarabine, or hematopoietic stem cell transplantation did not increase the risk of TB development. AML patients who developed TB had a higher mortality rate than those who did not (adjusted HR 1.63, 95% CI 1.33–1.99, p < 0.001).
Conclusion
Patients with AML had a higher risk of TB, especially within two years of diagnosis. Being male and having liver cirrhosis were independent risk factors for TB in AML patients. Physicians should be aware of the TB situation among their respective populations, particularly those in endemic areas.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Epidemiology, Infection, Tuberculosis
Type: Publication Only
Background
To date, few studies have investigated the association between tuberculosis (TB) and acute myeloid leukemia (AML).
Aims
We therefore aim to assess the impact and the risk factors of TB in patients with AML for a better risk stratification strategy.
Methods
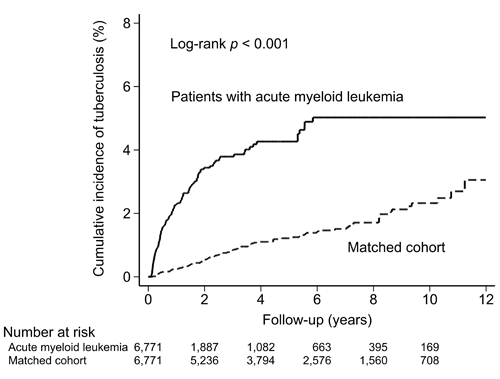
We conducted a nationwide population-based study using data retrieved from Taiwan’s National Health Insurance Research Database to determine the incidence of TB and to analyze the risk factors for TB in patients with newly diagnosed AML. From 2000 to 2011, we identified 6,771 AML patients and the same number of subjects without AML matched for sex, age, and comorbidities. Cox proportional hazards models were applied for further analysis. AML-related therapies were assessed as time-dependent covariates to avoid immortal time bias.
Results
Compared with the matched cohort, AML patients exhibited a higher risk for TB (adjusted hazard ratio [HR] 4.31, 95% confidence interval [CI] 3.27–5.67, p < 0.001), with an increased risk for both pulmonary (adjusted HR 4.22, 95% CI 3.13–5.69, p < 0·001) and extrapulmonary (adjusted HR 4.86, 95% CI 2.40–9.84, p < 0.001) TB. Adjusted HRs of TB occurrence for follow-up periods of < 1, 1–2, 2–5, and ≥ 5 years were 9.61 (95% CI 5.69–16.25), 5.40 (95% CI 2.88–10.13), 1.89 (95% CI 0.94–3.79), and 1.81 (95% CI 0.71–4.63), respectively. Multivariate analysis showed that being male (adjusted HR 1.47, 95% CI 1.06–2.04, p = 0.020) and having liver cirrhosis (adjusted HR 2.08, 95% CI 1.17–3.70, p = 0.012) were identified as independent risk factors for developing TB in AML patients. However, treatment with idarubicin, daunorubicin, high-dose cytarabine, or hematopoietic stem cell transplantation did not increase the risk of TB development. AML patients who developed TB had a higher mortality rate than those who did not (adjusted HR 1.63, 95% CI 1.33–1.99, p < 0.001).
Conclusion
Patients with AML had a higher risk of TB, especially within two years of diagnosis. Being male and having liver cirrhosis were independent risk factors for TB in AML patients. Physicians should be aware of the TB situation among their respective populations, particularly those in endemic areas.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Epidemiology, Infection, Tuberculosis
Abstract: PB1652
Type: Publication Only
Background
To date, few studies have investigated the association between tuberculosis (TB) and acute myeloid leukemia (AML).
Aims
We therefore aim to assess the impact and the risk factors of TB in patients with AML for a better risk stratification strategy.
Methods
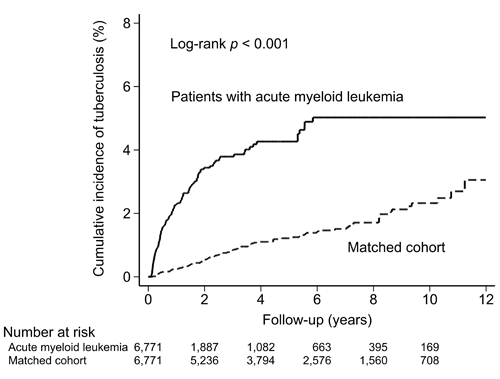
We conducted a nationwide population-based study using data retrieved from Taiwan’s National Health Insurance Research Database to determine the incidence of TB and to analyze the risk factors for TB in patients with newly diagnosed AML. From 2000 to 2011, we identified 6,771 AML patients and the same number of subjects without AML matched for sex, age, and comorbidities. Cox proportional hazards models were applied for further analysis. AML-related therapies were assessed as time-dependent covariates to avoid immortal time bias.
Results
Compared with the matched cohort, AML patients exhibited a higher risk for TB (adjusted hazard ratio [HR] 4.31, 95% confidence interval [CI] 3.27–5.67, p < 0.001), with an increased risk for both pulmonary (adjusted HR 4.22, 95% CI 3.13–5.69, p < 0·001) and extrapulmonary (adjusted HR 4.86, 95% CI 2.40–9.84, p < 0.001) TB. Adjusted HRs of TB occurrence for follow-up periods of < 1, 1–2, 2–5, and ≥ 5 years were 9.61 (95% CI 5.69–16.25), 5.40 (95% CI 2.88–10.13), 1.89 (95% CI 0.94–3.79), and 1.81 (95% CI 0.71–4.63), respectively. Multivariate analysis showed that being male (adjusted HR 1.47, 95% CI 1.06–2.04, p = 0.020) and having liver cirrhosis (adjusted HR 2.08, 95% CI 1.17–3.70, p = 0.012) were identified as independent risk factors for developing TB in AML patients. However, treatment with idarubicin, daunorubicin, high-dose cytarabine, or hematopoietic stem cell transplantation did not increase the risk of TB development. AML patients who developed TB had a higher mortality rate than those who did not (adjusted HR 1.63, 95% CI 1.33–1.99, p < 0.001).
Conclusion
Patients with AML had a higher risk of TB, especially within two years of diagnosis. Being male and having liver cirrhosis were independent risk factors for TB in AML patients. Physicians should be aware of the TB situation among their respective populations, particularly those in endemic areas.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Epidemiology, Infection, Tuberculosis
Type: Publication Only
Background
To date, few studies have investigated the association between tuberculosis (TB) and acute myeloid leukemia (AML).
Aims
We therefore aim to assess the impact and the risk factors of TB in patients with AML for a better risk stratification strategy.
Methods
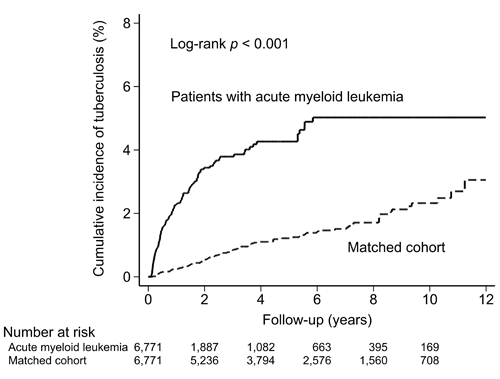
We conducted a nationwide population-based study using data retrieved from Taiwan’s National Health Insurance Research Database to determine the incidence of TB and to analyze the risk factors for TB in patients with newly diagnosed AML. From 2000 to 2011, we identified 6,771 AML patients and the same number of subjects without AML matched for sex, age, and comorbidities. Cox proportional hazards models were applied for further analysis. AML-related therapies were assessed as time-dependent covariates to avoid immortal time bias.
Results
Compared with the matched cohort, AML patients exhibited a higher risk for TB (adjusted hazard ratio [HR] 4.31, 95% confidence interval [CI] 3.27–5.67, p < 0.001), with an increased risk for both pulmonary (adjusted HR 4.22, 95% CI 3.13–5.69, p < 0·001) and extrapulmonary (adjusted HR 4.86, 95% CI 2.40–9.84, p < 0.001) TB. Adjusted HRs of TB occurrence for follow-up periods of < 1, 1–2, 2–5, and ≥ 5 years were 9.61 (95% CI 5.69–16.25), 5.40 (95% CI 2.88–10.13), 1.89 (95% CI 0.94–3.79), and 1.81 (95% CI 0.71–4.63), respectively. Multivariate analysis showed that being male (adjusted HR 1.47, 95% CI 1.06–2.04, p = 0.020) and having liver cirrhosis (adjusted HR 2.08, 95% CI 1.17–3.70, p = 0.012) were identified as independent risk factors for developing TB in AML patients. However, treatment with idarubicin, daunorubicin, high-dose cytarabine, or hematopoietic stem cell transplantation did not increase the risk of TB development. AML patients who developed TB had a higher mortality rate than those who did not (adjusted HR 1.63, 95% CI 1.33–1.99, p < 0.001).
Conclusion
Patients with AML had a higher risk of TB, especially within two years of diagnosis. Being male and having liver cirrhosis were independent risk factors for TB in AML patients. Physicians should be aware of the TB situation among their respective populations, particularly those in endemic areas.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Epidemiology, Infection, Tuberculosis
{{ help_message }}
{{filter}}


