IMPACT OF ADDITIONAL CYTOGENETIC ABERRATIONS ON OUTCOME OF ALLOGENEIC HEMATOPOIETIC STEM CELL TRANSPLANTATION IN PATIENTS WITH RUNX1-RUNX1T1 ACUTE MYELOID LEUKEMIA
(Abstract release date: 05/19/16)
EHA Library. Gindina T. 06/09/16; 134549; PB1649

Dr. Tatiana Gindina
Contributions
Contributions
Abstract
Abstract: PB1649
Type: Publication Only
Background
RUNX1-RUNX1T1-positive acute myeloid leukemia (AML) is considered as a favorable group. Allo-HSCT has been generally used for relapsed patients (pts), although prognostic factors are still unclear and prognostic significance of additional cytogenetic aberrations (ACA) in transplanted pts is contradictory.
Aims
To evaluate impact of additional cytogenetic aberrations on outcome of allogeneic hematopoietic stem cell transplantation in patients with RUNX1-RUNX1T1 acute myeloid leukemia
Methods
In this study, outcomes in 25 RUNX1-RUNX1T1-positive AML patients (pts), who were transplanted in a single institution between 2008 and 2015, were analyzed. All patients and transplant characteristics are listed in Table I.
Results
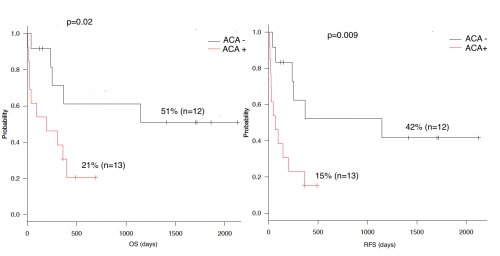
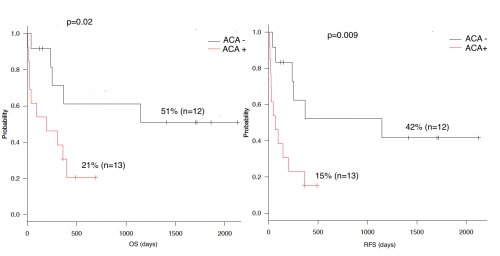
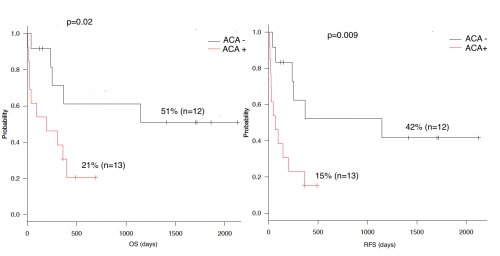
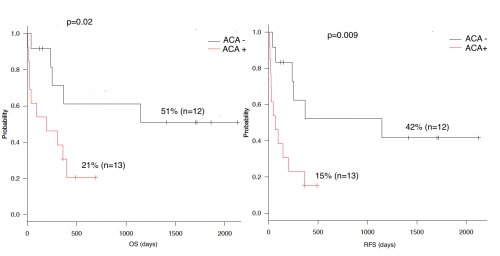
The median follow-up was 566 (8 – 2127) days. Overall survival (OS) was 33% (95% CI 14-53) and relapse free survival (RFS) was 26% (95% CI 9-45) at 4 years estimated with Kaplan-Meier method. In univariate analysis, prognostic factors associated with increased OS and RFS were age (>18 vs <18 years; p=0.03, p=0.0006, respectively), donor type (match related vs match unrelated vs haploidentical; p=0.0003, p=0.02, respectively), disease status at transplant (complete remission vs active disease; p=0.0002, p=0.005, respectively), the interval from diagnosis to transplant (<360 vs >360 days; p=0.008, p=0.9, respectively), ACA (ACA- vs ACA+; p=0.02, p=0.009, respectively) (Figure 1), complex karyotype (CK- vs CK+ ; p=0.004, p=0.0003, respectively). In multivariate analysis, the ACA (HR-13.5; P=0.04), the donor type (HR-6.86; P=0.01), the interval from diagnosis to HSCT (HR-6.80; P=0.02) remained statistically significant for OS. Moreover, age (HR-0.11; P=0.004) and the donor type (HR-4.16; P=0.04) were independent predictors of RFS.
Conclusion
The study demonstrates that the ACAs are independent prognostic factor for RUNX1-RUNX1T1-AML in transplanted pts. Since chemotherapy and cytotoxic conditioning regimen may be responsible for production of new ACAs, these regimens should be change by substitution of more toxic alkylating agents to less toxic.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, AML, Cytogenetic abnormalities, Prognosis
Type: Publication Only
Background
RUNX1-RUNX1T1-positive acute myeloid leukemia (AML) is considered as a favorable group. Allo-HSCT has been generally used for relapsed patients (pts), although prognostic factors are still unclear and prognostic significance of additional cytogenetic aberrations (ACA) in transplanted pts is contradictory.
Aims
To evaluate impact of additional cytogenetic aberrations on outcome of allogeneic hematopoietic stem cell transplantation in patients with RUNX1-RUNX1T1 acute myeloid leukemia
Methods
In this study, outcomes in 25 RUNX1-RUNX1T1-positive AML patients (pts), who were transplanted in a single institution between 2008 and 2015, were analyzed. All patients and transplant characteristics are listed in Table I.
| Number of patients | 25 (100 %) |
| Patient sex, n (%)MaleFemale | 15 (60 %)10 (40 %) |
| Age at HSCT, median, (range) years | 20.2 (2-58) |
| Age group≤18 yo ≥18 yo | 12 (48 %)13 (52 %) |
| Cytogenetics, n (%) t(8;21) without additional cytogenetic aberrationt(8;21) with additional cytogenetic aberrationComplex karyotype -Complex karyotype + | 12 (48 %)13 (52 %)16 (64 %) 9 (36 %) |
| Time from diagnosis to HSCT, n (%)<360 days>360 days | 14 (56 %)11 (44 %) |
| Clinical stage at HSCT, n (%)CRActive disease | 13 (52 %)12 (48 %) |
| HSC source, n (%)Bone marrowPeripheral bloodBoth | 13 (52 %)11 (44 %)1 (4 %) |
| Conditioning regimen, n (%)MANon-MA | 12 (48 %)13 (52 %) |
| Donor type, n (%)HLA-id siblingMatched unrelatedHaploidentical | 7 (28 %)12 (48 %)6 (24 %) |
Results
The median follow-up was 566 (8 – 2127) days. Overall survival (OS) was 33% (95% CI 14-53) and relapse free survival (RFS) was 26% (95% CI 9-45) at 4 years estimated with Kaplan-Meier method. In univariate analysis, prognostic factors associated with increased OS and RFS were age (>18 vs <18 years; p=0.03, p=0.0006, respectively), donor type (match related vs match unrelated vs haploidentical; p=0.0003, p=0.02, respectively), disease status at transplant (complete remission vs active disease; p=0.0002, p=0.005, respectively), the interval from diagnosis to transplant (<360 vs >360 days; p=0.008, p=0.9, respectively), ACA (ACA- vs ACA+; p=0.02, p=0.009, respectively) (Figure 1), complex karyotype (CK- vs CK+ ; p=0.004, p=0.0003, respectively). In multivariate analysis, the ACA (HR-13.5; P=0.04), the donor type (HR-6.86; P=0.01), the interval from diagnosis to HSCT (HR-6.80; P=0.02) remained statistically significant for OS. Moreover, age (HR-0.11; P=0.004) and the donor type (HR-4.16; P=0.04) were independent predictors of RFS.
Conclusion
The study demonstrates that the ACAs are independent prognostic factor for RUNX1-RUNX1T1-AML in transplanted pts. Since chemotherapy and cytotoxic conditioning regimen may be responsible for production of new ACAs, these regimens should be change by substitution of more toxic alkylating agents to less toxic.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, AML, Cytogenetic abnormalities, Prognosis
Abstract: PB1649
Type: Publication Only
Background
RUNX1-RUNX1T1-positive acute myeloid leukemia (AML) is considered as a favorable group. Allo-HSCT has been generally used for relapsed patients (pts), although prognostic factors are still unclear and prognostic significance of additional cytogenetic aberrations (ACA) in transplanted pts is contradictory.
Aims
To evaluate impact of additional cytogenetic aberrations on outcome of allogeneic hematopoietic stem cell transplantation in patients with RUNX1-RUNX1T1 acute myeloid leukemia
Methods
In this study, outcomes in 25 RUNX1-RUNX1T1-positive AML patients (pts), who were transplanted in a single institution between 2008 and 2015, were analyzed. All patients and transplant characteristics are listed in Table I.
Results
The median follow-up was 566 (8 – 2127) days. Overall survival (OS) was 33% (95% CI 14-53) and relapse free survival (RFS) was 26% (95% CI 9-45) at 4 years estimated with Kaplan-Meier method. In univariate analysis, prognostic factors associated with increased OS and RFS were age (>18 vs <18 years; p=0.03, p=0.0006, respectively), donor type (match related vs match unrelated vs haploidentical; p=0.0003, p=0.02, respectively), disease status at transplant (complete remission vs active disease; p=0.0002, p=0.005, respectively), the interval from diagnosis to transplant (<360 vs >360 days; p=0.008, p=0.9, respectively), ACA (ACA- vs ACA+; p=0.02, p=0.009, respectively) (Figure 1), complex karyotype (CK- vs CK+ ; p=0.004, p=0.0003, respectively). In multivariate analysis, the ACA (HR-13.5; P=0.04), the donor type (HR-6.86; P=0.01), the interval from diagnosis to HSCT (HR-6.80; P=0.02) remained statistically significant for OS. Moreover, age (HR-0.11; P=0.004) and the donor type (HR-4.16; P=0.04) were independent predictors of RFS.
Conclusion
The study demonstrates that the ACAs are independent prognostic factor for RUNX1-RUNX1T1-AML in transplanted pts. Since chemotherapy and cytotoxic conditioning regimen may be responsible for production of new ACAs, these regimens should be change by substitution of more toxic alkylating agents to less toxic.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, AML, Cytogenetic abnormalities, Prognosis
Type: Publication Only
Background
RUNX1-RUNX1T1-positive acute myeloid leukemia (AML) is considered as a favorable group. Allo-HSCT has been generally used for relapsed patients (pts), although prognostic factors are still unclear and prognostic significance of additional cytogenetic aberrations (ACA) in transplanted pts is contradictory.
Aims
To evaluate impact of additional cytogenetic aberrations on outcome of allogeneic hematopoietic stem cell transplantation in patients with RUNX1-RUNX1T1 acute myeloid leukemia
Methods
In this study, outcomes in 25 RUNX1-RUNX1T1-positive AML patients (pts), who were transplanted in a single institution between 2008 and 2015, were analyzed. All patients and transplant characteristics are listed in Table I.
| Number of patients | 25 (100 %) |
| Patient sex, n (%)MaleFemale | 15 (60 %)10 (40 %) |
| Age at HSCT, median, (range) years | 20.2 (2-58) |
| Age group≤18 yo ≥18 yo | 12 (48 %)13 (52 %) |
| Cytogenetics, n (%) t(8;21) without additional cytogenetic aberrationt(8;21) with additional cytogenetic aberrationComplex karyotype -Complex karyotype + | 12 (48 %)13 (52 %)16 (64 %) 9 (36 %) |
| Time from diagnosis to HSCT, n (%)<360 days>360 days | 14 (56 %)11 (44 %) |
| Clinical stage at HSCT, n (%)CRActive disease | 13 (52 %)12 (48 %) |
| HSC source, n (%)Bone marrowPeripheral bloodBoth | 13 (52 %)11 (44 %)1 (4 %) |
| Conditioning regimen, n (%)MANon-MA | 12 (48 %)13 (52 %) |
| Donor type, n (%)HLA-id siblingMatched unrelatedHaploidentical | 7 (28 %)12 (48 %)6 (24 %) |
Results
The median follow-up was 566 (8 – 2127) days. Overall survival (OS) was 33% (95% CI 14-53) and relapse free survival (RFS) was 26% (95% CI 9-45) at 4 years estimated with Kaplan-Meier method. In univariate analysis, prognostic factors associated with increased OS and RFS were age (>18 vs <18 years; p=0.03, p=0.0006, respectively), donor type (match related vs match unrelated vs haploidentical; p=0.0003, p=0.02, respectively), disease status at transplant (complete remission vs active disease; p=0.0002, p=0.005, respectively), the interval from diagnosis to transplant (<360 vs >360 days; p=0.008, p=0.9, respectively), ACA (ACA- vs ACA+; p=0.02, p=0.009, respectively) (Figure 1), complex karyotype (CK- vs CK+ ; p=0.004, p=0.0003, respectively). In multivariate analysis, the ACA (HR-13.5; P=0.04), the donor type (HR-6.86; P=0.01), the interval from diagnosis to HSCT (HR-6.80; P=0.02) remained statistically significant for OS. Moreover, age (HR-0.11; P=0.004) and the donor type (HR-4.16; P=0.04) were independent predictors of RFS.
Conclusion
The study demonstrates that the ACAs are independent prognostic factor for RUNX1-RUNX1T1-AML in transplanted pts. Since chemotherapy and cytotoxic conditioning regimen may be responsible for production of new ACAs, these regimens should be change by substitution of more toxic alkylating agents to less toxic.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, AML, Cytogenetic abnormalities, Prognosis
{{ help_message }}
{{filter}}


