RISK OF CEREBRAL VEIN THROMBOSIS (CVT) IN ADULT ALL PATIENTS IN FINLAND 1999-2012: SUGGESTION FOR A LEUKEMIA-RELATED PREDICTIVE SCORING MODEL
(Abstract release date: 05/19/16)
EHA Library. Roininen S. 06/10/16; 133158; P170

Mrs. Saara Roininen
Contributions
Contributions
Abstract
Abstract: P170
Type: Poster Presentation
Presentation during EHA21: On Friday, June 10, 2016 from 17:15 - 18:45
Location: Poster area (Hall H)
Background
Thrombosis causes remarkable morbidity among patients with cancer and is the second leading cause of death after malignancy itself in this patient group. Khorana score estimates the risk of deep venous thrombosis (DVT) in solid tumor neoplasms, and may help physicians to prevent thrombotic complications. However, Khorana score is not applicable in acute leukemias and specific leukemia-related thrombosis risk score is still called for. Previous analyses focusing on thrombosis in ALL patients have mainly been conducted on pediatric study groups. Thrombotic risk profile in adult patients could, however, differ from children and these studies may not be converted straight-forward to adult setting.
Aims
To identify patient characteristics detectable at ALL diagnosis and possibly predisposing to CVT, which often represents with the most drastic consequences in patient’s life.
Methods
We performed a population-based retrospective registry analysis on 186 adult-ALL patients treated with a national study protocol ALL2000 between years 1999-2012 in Finland.
Results
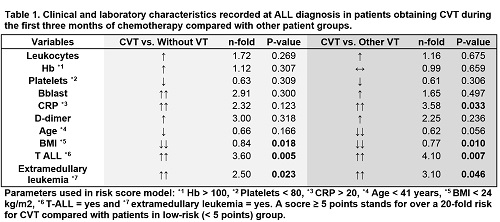
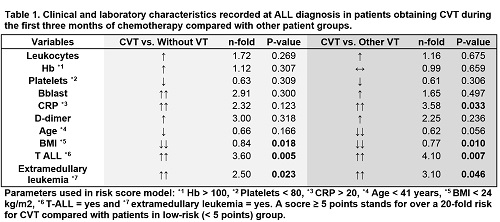
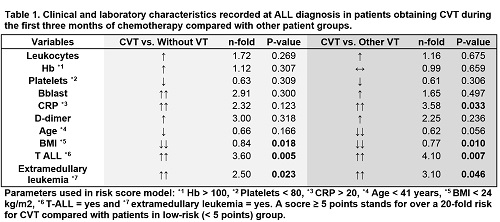
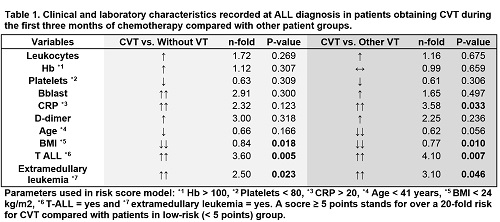
Of patients, 118 patients had pre-B ALL, 37 Philadelphia chromosome positive ALL and 31 T-ALL. Thirty-one patients (19%) suffered from a venous thrombosis (VT), whereof 9 (27%) from a CVT. Patients with CVT were thinner (p=0.018 and p=0.010) and had more T-ALL (Pearson Chi-Square values: 10.61, p=0.005 and 9.93, p=0.007), extramedullary leukemia (Pearson Chi-Square values: 5.167, p=0.023 and 5.412, p=0.046), and a higher pre-chemotherapy CRP (p=0.033 and p=0.123) compared with both patients without VT and with other VTs, respectively (Table 1). A trend for younger age, higher pre-chemotherapy D-dimer, leukocyte and blood blast counts, and a lower platelet count was also detected in patients with CVT in this setting. CVT patients also presented with a higher pre-chemotherapy hemoglobin compared with patients without VT but this distinction did not reach statistical significance. Notably, most CVTs (n=5/9) occurred prior to the introduction of asparaginase, which is known to be the major factor predisposing ALL patients to thrombotic complications. None of the CVT patients had received intrathecal cytostatic treatment during the previous week before the thrombosis was diagnosed.Based on these results we constructed a risk model for CVT, which takes into account seven basic features detectable in patients at ALL diagnosis (Table 1). Patients scoring ≥ 5 points represented with a 20-fold risk for CVT compared with the low-risk (<5 points) patients (HR=20.841, p<0.0001, CI: 5.208-83.401) in our study group. The scoring model showed a very good specificity and satisfying sensitivity (NPV: 0.982, PPV: 0.375) in this study and is currently under validation in another patient cohort.
Conclusion
Thrombotic events and especially CVTs often have a major impact on patients with ALL during their course of leukemia treatment and after. Here, we present a set of laboratory and clinical characteristics identifiable at ALL diagnosis and associating with a very high risk of CVT during the first months of ALL treatment. These high-risk characteristics (e.g. low BMI and young age) are partly in contradiction to the acknowledged features predisposing patients to other forms of VT. This phenomenon hints for a distinctive mechanism of CVT in ALL patients possibly in linkage with ALL biology.
Session topic: Acute lymphoblastic leukemia - Clinical 1
Keyword(s): ALL, Risk factor, Thrombosis
Type: Poster Presentation
Presentation during EHA21: On Friday, June 10, 2016 from 17:15 - 18:45
Location: Poster area (Hall H)
Background
Thrombosis causes remarkable morbidity among patients with cancer and is the second leading cause of death after malignancy itself in this patient group. Khorana score estimates the risk of deep venous thrombosis (DVT) in solid tumor neoplasms, and may help physicians to prevent thrombotic complications. However, Khorana score is not applicable in acute leukemias and specific leukemia-related thrombosis risk score is still called for. Previous analyses focusing on thrombosis in ALL patients have mainly been conducted on pediatric study groups. Thrombotic risk profile in adult patients could, however, differ from children and these studies may not be converted straight-forward to adult setting.
Aims
To identify patient characteristics detectable at ALL diagnosis and possibly predisposing to CVT, which often represents with the most drastic consequences in patient’s life.
Methods
We performed a population-based retrospective registry analysis on 186 adult-ALL patients treated with a national study protocol ALL2000 between years 1999-2012 in Finland.
Results
Of patients, 118 patients had pre-B ALL, 37 Philadelphia chromosome positive ALL and 31 T-ALL. Thirty-one patients (19%) suffered from a venous thrombosis (VT), whereof 9 (27%) from a CVT. Patients with CVT were thinner (p=0.018 and p=0.010) and had more T-ALL (Pearson Chi-Square values: 10.61, p=0.005 and 9.93, p=0.007), extramedullary leukemia (Pearson Chi-Square values: 5.167, p=0.023 and 5.412, p=0.046), and a higher pre-chemotherapy CRP (p=0.033 and p=0.123) compared with both patients without VT and with other VTs, respectively (Table 1). A trend for younger age, higher pre-chemotherapy D-dimer, leukocyte and blood blast counts, and a lower platelet count was also detected in patients with CVT in this setting. CVT patients also presented with a higher pre-chemotherapy hemoglobin compared with patients without VT but this distinction did not reach statistical significance. Notably, most CVTs (n=5/9) occurred prior to the introduction of asparaginase, which is known to be the major factor predisposing ALL patients to thrombotic complications. None of the CVT patients had received intrathecal cytostatic treatment during the previous week before the thrombosis was diagnosed.Based on these results we constructed a risk model for CVT, which takes into account seven basic features detectable in patients at ALL diagnosis (Table 1). Patients scoring ≥ 5 points represented with a 20-fold risk for CVT compared with the low-risk (<5 points) patients (HR=20.841, p<0.0001, CI: 5.208-83.401) in our study group. The scoring model showed a very good specificity and satisfying sensitivity (NPV: 0.982, PPV: 0.375) in this study and is currently under validation in another patient cohort.
Conclusion
Thrombotic events and especially CVTs often have a major impact on patients with ALL during their course of leukemia treatment and after. Here, we present a set of laboratory and clinical characteristics identifiable at ALL diagnosis and associating with a very high risk of CVT during the first months of ALL treatment. These high-risk characteristics (e.g. low BMI and young age) are partly in contradiction to the acknowledged features predisposing patients to other forms of VT. This phenomenon hints for a distinctive mechanism of CVT in ALL patients possibly in linkage with ALL biology.
Session topic: Acute lymphoblastic leukemia - Clinical 1
Keyword(s): ALL, Risk factor, Thrombosis
Abstract: P170
Type: Poster Presentation
Presentation during EHA21: On Friday, June 10, 2016 from 17:15 - 18:45
Location: Poster area (Hall H)
Background
Thrombosis causes remarkable morbidity among patients with cancer and is the second leading cause of death after malignancy itself in this patient group. Khorana score estimates the risk of deep venous thrombosis (DVT) in solid tumor neoplasms, and may help physicians to prevent thrombotic complications. However, Khorana score is not applicable in acute leukemias and specific leukemia-related thrombosis risk score is still called for. Previous analyses focusing on thrombosis in ALL patients have mainly been conducted on pediatric study groups. Thrombotic risk profile in adult patients could, however, differ from children and these studies may not be converted straight-forward to adult setting.
Aims
To identify patient characteristics detectable at ALL diagnosis and possibly predisposing to CVT, which often represents with the most drastic consequences in patient’s life.
Methods
We performed a population-based retrospective registry analysis on 186 adult-ALL patients treated with a national study protocol ALL2000 between years 1999-2012 in Finland.
Results
Of patients, 118 patients had pre-B ALL, 37 Philadelphia chromosome positive ALL and 31 T-ALL. Thirty-one patients (19%) suffered from a venous thrombosis (VT), whereof 9 (27%) from a CVT. Patients with CVT were thinner (p=0.018 and p=0.010) and had more T-ALL (Pearson Chi-Square values: 10.61, p=0.005 and 9.93, p=0.007), extramedullary leukemia (Pearson Chi-Square values: 5.167, p=0.023 and 5.412, p=0.046), and a higher pre-chemotherapy CRP (p=0.033 and p=0.123) compared with both patients without VT and with other VTs, respectively (Table 1). A trend for younger age, higher pre-chemotherapy D-dimer, leukocyte and blood blast counts, and a lower platelet count was also detected in patients with CVT in this setting. CVT patients also presented with a higher pre-chemotherapy hemoglobin compared with patients without VT but this distinction did not reach statistical significance. Notably, most CVTs (n=5/9) occurred prior to the introduction of asparaginase, which is known to be the major factor predisposing ALL patients to thrombotic complications. None of the CVT patients had received intrathecal cytostatic treatment during the previous week before the thrombosis was diagnosed.Based on these results we constructed a risk model for CVT, which takes into account seven basic features detectable in patients at ALL diagnosis (Table 1). Patients scoring ≥ 5 points represented with a 20-fold risk for CVT compared with the low-risk (<5 points) patients (HR=20.841, p<0.0001, CI: 5.208-83.401) in our study group. The scoring model showed a very good specificity and satisfying sensitivity (NPV: 0.982, PPV: 0.375) in this study and is currently under validation in another patient cohort.
Conclusion
Thrombotic events and especially CVTs often have a major impact on patients with ALL during their course of leukemia treatment and after. Here, we present a set of laboratory and clinical characteristics identifiable at ALL diagnosis and associating with a very high risk of CVT during the first months of ALL treatment. These high-risk characteristics (e.g. low BMI and young age) are partly in contradiction to the acknowledged features predisposing patients to other forms of VT. This phenomenon hints for a distinctive mechanism of CVT in ALL patients possibly in linkage with ALL biology.
Session topic: Acute lymphoblastic leukemia - Clinical 1
Keyword(s): ALL, Risk factor, Thrombosis
Type: Poster Presentation
Presentation during EHA21: On Friday, June 10, 2016 from 17:15 - 18:45
Location: Poster area (Hall H)
Background
Thrombosis causes remarkable morbidity among patients with cancer and is the second leading cause of death after malignancy itself in this patient group. Khorana score estimates the risk of deep venous thrombosis (DVT) in solid tumor neoplasms, and may help physicians to prevent thrombotic complications. However, Khorana score is not applicable in acute leukemias and specific leukemia-related thrombosis risk score is still called for. Previous analyses focusing on thrombosis in ALL patients have mainly been conducted on pediatric study groups. Thrombotic risk profile in adult patients could, however, differ from children and these studies may not be converted straight-forward to adult setting.
Aims
To identify patient characteristics detectable at ALL diagnosis and possibly predisposing to CVT, which often represents with the most drastic consequences in patient’s life.
Methods
We performed a population-based retrospective registry analysis on 186 adult-ALL patients treated with a national study protocol ALL2000 between years 1999-2012 in Finland.
Results
Of patients, 118 patients had pre-B ALL, 37 Philadelphia chromosome positive ALL and 31 T-ALL. Thirty-one patients (19%) suffered from a venous thrombosis (VT), whereof 9 (27%) from a CVT. Patients with CVT were thinner (p=0.018 and p=0.010) and had more T-ALL (Pearson Chi-Square values: 10.61, p=0.005 and 9.93, p=0.007), extramedullary leukemia (Pearson Chi-Square values: 5.167, p=0.023 and 5.412, p=0.046), and a higher pre-chemotherapy CRP (p=0.033 and p=0.123) compared with both patients without VT and with other VTs, respectively (Table 1). A trend for younger age, higher pre-chemotherapy D-dimer, leukocyte and blood blast counts, and a lower platelet count was also detected in patients with CVT in this setting. CVT patients also presented with a higher pre-chemotherapy hemoglobin compared with patients without VT but this distinction did not reach statistical significance. Notably, most CVTs (n=5/9) occurred prior to the introduction of asparaginase, which is known to be the major factor predisposing ALL patients to thrombotic complications. None of the CVT patients had received intrathecal cytostatic treatment during the previous week before the thrombosis was diagnosed.Based on these results we constructed a risk model for CVT, which takes into account seven basic features detectable in patients at ALL diagnosis (Table 1). Patients scoring ≥ 5 points represented with a 20-fold risk for CVT compared with the low-risk (<5 points) patients (HR=20.841, p<0.0001, CI: 5.208-83.401) in our study group. The scoring model showed a very good specificity and satisfying sensitivity (NPV: 0.982, PPV: 0.375) in this study and is currently under validation in another patient cohort.
Conclusion
Thrombotic events and especially CVTs often have a major impact on patients with ALL during their course of leukemia treatment and after. Here, we present a set of laboratory and clinical characteristics identifiable at ALL diagnosis and associating with a very high risk of CVT during the first months of ALL treatment. These high-risk characteristics (e.g. low BMI and young age) are partly in contradiction to the acknowledged features predisposing patients to other forms of VT. This phenomenon hints for a distinctive mechanism of CVT in ALL patients possibly in linkage with ALL biology.
Session topic: Acute lymphoblastic leukemia - Clinical 1
Keyword(s): ALL, Risk factor, Thrombosis
{{ help_message }}
{{filter}}


