TRANSFUSION PRACTICES USED IN TERMINAL STAGE –CANCER-PATIENTS
(Abstract release date: 05/19/16)
EHA Library. Argyrou A. 06/09/16; 133117; E1568

Dr. Aspasia Argyrou
Contributions
Contributions
Abstract
Abstract: E1568
Type: Eposter Presentation
Background
Despite the increased attention to quality palliative care, dying of oncology patients often take place in the ward or intensive care unit rather than hospice and with an intensive level of medical care.
Aims
To investigate the transfusion practises for the terminally ill cancer patients as part of their medical care during the last seven days of life.
Methods
We conducted a retrospective review of the causes of consecutive deaths oncology patients who succumbed in two Oncology Hospitals between April 2015 and June 2015.Patients were categorized as: solid tumor-patients, haematological malignancy-patients and no cancer-patients. We recorded the pretransfusion tests performed for these patients (ABO grouping, detection and identification tests for unexpected alloantibodies, crossmatching), as well as the transfusion episodes per patient and the number of transfused units per transfusion episode, during the last seven days of life. X2-test and one-way ANOVA tests were used for the statistical analysis. The number of transfused platelets corresponds to equivalent number of platelets random-donor.
Results
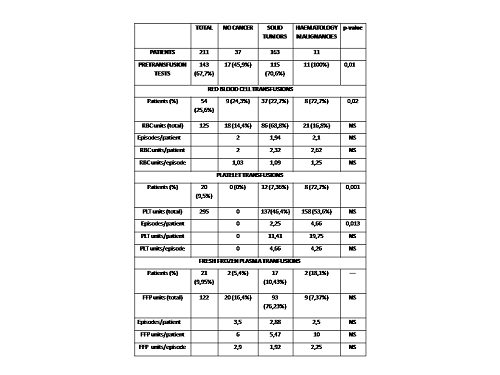
211 patients [116 males (55%) and 93 females (45%)] of mean age 67 years old (range 18-92) had died during the study period. Of them, 163 (77.25%) were solid tumor-patients, 11 (5.22%) were haematological malignancy-patients and 37 (17.53%) were no cancer-patients. The number of pretransfusion tests performed and blood product units transfused, are shown in the Table.
Conclusion
1. Blood transfusion practices remained intensive in terminal stage-cancer-patients and does not seem to be different compared to non-cancer patients.2. Patients with haematological malignancies had even more intensive transfusion practises especially regarding the platelet- transfusion- episodes.3. Cooperation with local hospital Transfusion Medicine Committee and the Ethics Committee, and proper allocation of medical resources could result in providing the optimal end-of-life care for cancer patients. The blood is a valuable but limited source. The health services have the duty to achieve both the maximum “beneficity” by transfusing blood products to the terminally ill patients, and “justice” by not depriving other patients of necessary transfusions.
Session topic: E-poster
Keyword(s): Hematological malignancy, Solid tumor, Transfusion
Type: Eposter Presentation
Background
Despite the increased attention to quality palliative care, dying of oncology patients often take place in the ward or intensive care unit rather than hospice and with an intensive level of medical care.
Aims
To investigate the transfusion practises for the terminally ill cancer patients as part of their medical care during the last seven days of life.
Methods
We conducted a retrospective review of the causes of consecutive deaths oncology patients who succumbed in two Oncology Hospitals between April 2015 and June 2015.Patients were categorized as: solid tumor-patients, haematological malignancy-patients and no cancer-patients. We recorded the pretransfusion tests performed for these patients (ABO grouping, detection and identification tests for unexpected alloantibodies, crossmatching), as well as the transfusion episodes per patient and the number of transfused units per transfusion episode, during the last seven days of life. X2-test and one-way ANOVA tests were used for the statistical analysis. The number of transfused platelets corresponds to equivalent number of platelets random-donor.
Results
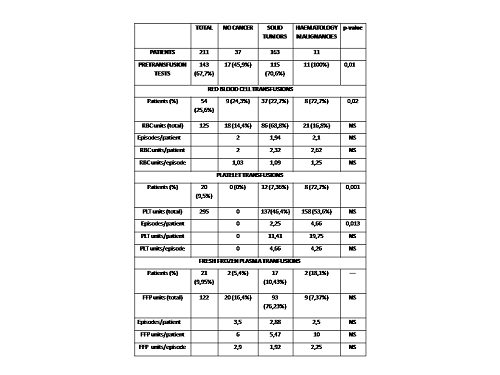
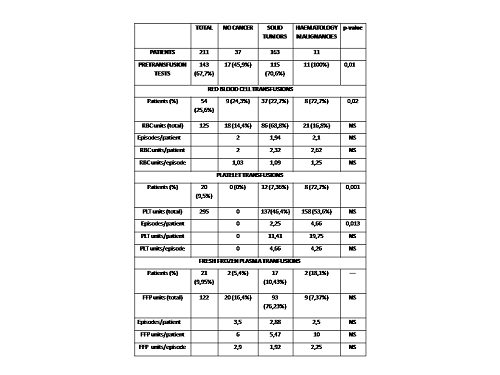
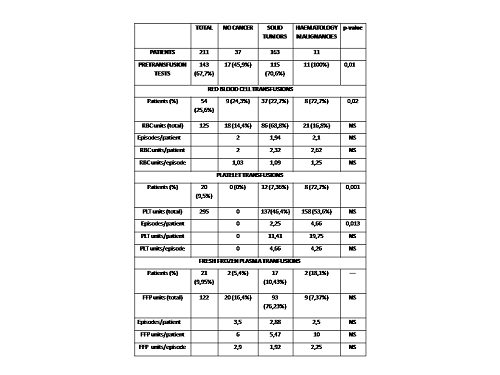
211 patients [116 males (55%) and 93 females (45%)] of mean age 67 years old (range 18-92) had died during the study period. Of them, 163 (77.25%) were solid tumor-patients, 11 (5.22%) were haematological malignancy-patients and 37 (17.53%) were no cancer-patients. The number of pretransfusion tests performed and blood product units transfused, are shown in the Table.
Conclusion
1. Blood transfusion practices remained intensive in terminal stage-cancer-patients and does not seem to be different compared to non-cancer patients.2. Patients with haematological malignancies had even more intensive transfusion practises especially regarding the platelet- transfusion- episodes.3. Cooperation with local hospital Transfusion Medicine Committee and the Ethics Committee, and proper allocation of medical resources could result in providing the optimal end-of-life care for cancer patients. The blood is a valuable but limited source. The health services have the duty to achieve both the maximum “beneficity” by transfusing blood products to the terminally ill patients, and “justice” by not depriving other patients of necessary transfusions.
Session topic: E-poster
Keyword(s): Hematological malignancy, Solid tumor, Transfusion
Abstract: E1568
Type: Eposter Presentation
Background
Despite the increased attention to quality palliative care, dying of oncology patients often take place in the ward or intensive care unit rather than hospice and with an intensive level of medical care.
Aims
To investigate the transfusion practises for the terminally ill cancer patients as part of their medical care during the last seven days of life.
Methods
We conducted a retrospective review of the causes of consecutive deaths oncology patients who succumbed in two Oncology Hospitals between April 2015 and June 2015.Patients were categorized as: solid tumor-patients, haematological malignancy-patients and no cancer-patients. We recorded the pretransfusion tests performed for these patients (ABO grouping, detection and identification tests for unexpected alloantibodies, crossmatching), as well as the transfusion episodes per patient and the number of transfused units per transfusion episode, during the last seven days of life. X2-test and one-way ANOVA tests were used for the statistical analysis. The number of transfused platelets corresponds to equivalent number of platelets random-donor.
Results
211 patients [116 males (55%) and 93 females (45%)] of mean age 67 years old (range 18-92) had died during the study period. Of them, 163 (77.25%) were solid tumor-patients, 11 (5.22%) were haematological malignancy-patients and 37 (17.53%) were no cancer-patients. The number of pretransfusion tests performed and blood product units transfused, are shown in the Table.
Conclusion
1. Blood transfusion practices remained intensive in terminal stage-cancer-patients and does not seem to be different compared to non-cancer patients.2. Patients with haematological malignancies had even more intensive transfusion practises especially regarding the platelet- transfusion- episodes.3. Cooperation with local hospital Transfusion Medicine Committee and the Ethics Committee, and proper allocation of medical resources could result in providing the optimal end-of-life care for cancer patients. The blood is a valuable but limited source. The health services have the duty to achieve both the maximum “beneficity” by transfusing blood products to the terminally ill patients, and “justice” by not depriving other patients of necessary transfusions.
Session topic: E-poster
Keyword(s): Hematological malignancy, Solid tumor, Transfusion
Type: Eposter Presentation
Background
Despite the increased attention to quality palliative care, dying of oncology patients often take place in the ward or intensive care unit rather than hospice and with an intensive level of medical care.
Aims
To investigate the transfusion practises for the terminally ill cancer patients as part of their medical care during the last seven days of life.
Methods
We conducted a retrospective review of the causes of consecutive deaths oncology patients who succumbed in two Oncology Hospitals between April 2015 and June 2015.Patients were categorized as: solid tumor-patients, haematological malignancy-patients and no cancer-patients. We recorded the pretransfusion tests performed for these patients (ABO grouping, detection and identification tests for unexpected alloantibodies, crossmatching), as well as the transfusion episodes per patient and the number of transfused units per transfusion episode, during the last seven days of life. X2-test and one-way ANOVA tests were used for the statistical analysis. The number of transfused platelets corresponds to equivalent number of platelets random-donor.
Results
211 patients [116 males (55%) and 93 females (45%)] of mean age 67 years old (range 18-92) had died during the study period. Of them, 163 (77.25%) were solid tumor-patients, 11 (5.22%) were haematological malignancy-patients and 37 (17.53%) were no cancer-patients. The number of pretransfusion tests performed and blood product units transfused, are shown in the Table.
Conclusion
1. Blood transfusion practices remained intensive in terminal stage-cancer-patients and does not seem to be different compared to non-cancer patients.2. Patients with haematological malignancies had even more intensive transfusion practises especially regarding the platelet- transfusion- episodes.3. Cooperation with local hospital Transfusion Medicine Committee and the Ethics Committee, and proper allocation of medical resources could result in providing the optimal end-of-life care for cancer patients. The blood is a valuable but limited source. The health services have the duty to achieve both the maximum “beneficity” by transfusing blood products to the terminally ill patients, and “justice” by not depriving other patients of necessary transfusions.
Session topic: E-poster
Keyword(s): Hematological malignancy, Solid tumor, Transfusion
{{ help_message }}
{{filter}}


