BEING OVERWEIGHT/OBESE PRIOR TO ALLOJENEIK HEMATOPOIETIC STEM CELL TRANSPLANTATION (ALLO-HSCT) IS RELATED TO BETTER OVERALL SURVIVAL (OS) AND DECREASED NON-RELASE MORTALITY
(Abstract release date: 05/19/16)
EHA Library. Atilla E. 06/09/16; 133095; E1546

Dr. Erden Atilla
Contributions
Contributions
Abstract
Abstract: E1546
Type: Eposter Presentation
Background
Obesity is an increasingly important health problem in developed countries and a cause of variability in treatment outcomes. The effect of being owerweight or obese had been studied in various populations in patients undergoing Allo-HSCT. Sorror et. al reported obesity as a factor in hemetopoietic cell transplant-specific comorbidity index and increased risk of non-relapse mortality (NRM).
Aims
In this study, we evaluated the impact of obesity on acute graft vs host disease (aGVHD) risk, overall survival (OS), relapse rate (RR), relapse free survival (RFS) and NRM in patients undergoing Allo-HSCT.
Methods
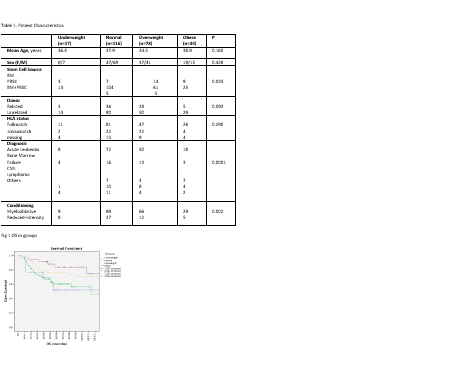
Retrospectively, 245 patients who underwent allo-HSCT between 2000 and 2015 at Ankara University School of Medicine was included in our study. Patients were classified into four groups based on pretransplant BMI values according to World Health Organization as follows: underweight (BMI < 18.5 kg/m2, n=17), normal (18.5 ≤ BMI < 25 mg/kg/m2, n=116), overweight (25 ≤ BMI < 30 mg/kg/m2, n=78) and obese (BMI ≥ 30 mg/kg/m2, n=34). Patients received weight adjusted chemotherapy doses. Characteristics of patients were compared using the Chi-squared test for categorical variables. The probilibity of OS was calculated by the Kaplan-Meier method.
Results
The patient characteristics are given in the table. Mean age of the group was 36.8 (range, 16-71). Overweight and obese patients received more bone marrow as a stem cell source (P=0.033). Bone marrow failure syndromes were more common diagnosis in normal and underweight recipients (p=0.0001). Myeloablative conditioning were prefered in overweight and obese group (p=0.002). Five year OS in underweight, normal, overweight and obese groups were as follows: 51%, 60%, 74% and 83% (P=0.005). Relaps rate was higher in underweight and normal compared to overweight and obese but not statistically different (23% vs 19%, P=0.53). 2-year RFS in underweight, normal, overweight and obese groups were as follows: 33%, 29%, 41%, 50%, P=0.069). The incidence of aGVHD detected higher in obese and overweight group however not statistically significant (44% vs 40%, p=0.6). NRM was lower in overweight and obese group (12% vs 31%, P=0.001).
Conclusion
Interestingly, we have demostrated that being overweight/obese improved OS and decreased NRM in our cohort. Relapse rate was higher in underweight and normal weight group however not statistically significant.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, Obesity
Type: Eposter Presentation
Background
Obesity is an increasingly important health problem in developed countries and a cause of variability in treatment outcomes. The effect of being owerweight or obese had been studied in various populations in patients undergoing Allo-HSCT. Sorror et. al reported obesity as a factor in hemetopoietic cell transplant-specific comorbidity index and increased risk of non-relapse mortality (NRM).
Aims
In this study, we evaluated the impact of obesity on acute graft vs host disease (aGVHD) risk, overall survival (OS), relapse rate (RR), relapse free survival (RFS) and NRM in patients undergoing Allo-HSCT.
Methods
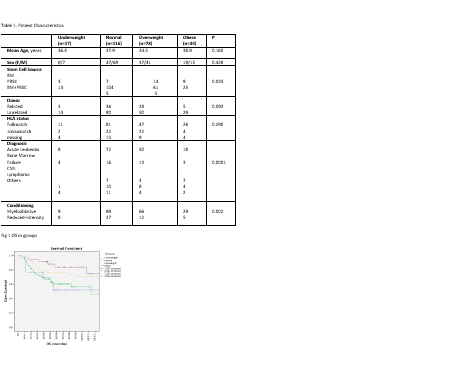
Retrospectively, 245 patients who underwent allo-HSCT between 2000 and 2015 at Ankara University School of Medicine was included in our study. Patients were classified into four groups based on pretransplant BMI values according to World Health Organization as follows: underweight (BMI < 18.5 kg/m2, n=17), normal (18.5 ≤ BMI < 25 mg/kg/m2, n=116), overweight (25 ≤ BMI < 30 mg/kg/m2, n=78) and obese (BMI ≥ 30 mg/kg/m2, n=34). Patients received weight adjusted chemotherapy doses. Characteristics of patients were compared using the Chi-squared test for categorical variables. The probilibity of OS was calculated by the Kaplan-Meier method.
Results
The patient characteristics are given in the table. Mean age of the group was 36.8 (range, 16-71). Overweight and obese patients received more bone marrow as a stem cell source (P=0.033). Bone marrow failure syndromes were more common diagnosis in normal and underweight recipients (p=0.0001). Myeloablative conditioning were prefered in overweight and obese group (p=0.002). Five year OS in underweight, normal, overweight and obese groups were as follows: 51%, 60%, 74% and 83% (P=0.005). Relaps rate was higher in underweight and normal compared to overweight and obese but not statistically different (23% vs 19%, P=0.53). 2-year RFS in underweight, normal, overweight and obese groups were as follows: 33%, 29%, 41%, 50%, P=0.069). The incidence of aGVHD detected higher in obese and overweight group however not statistically significant (44% vs 40%, p=0.6). NRM was lower in overweight and obese group (12% vs 31%, P=0.001).
Conclusion
Interestingly, we have demostrated that being overweight/obese improved OS and decreased NRM in our cohort. Relapse rate was higher in underweight and normal weight group however not statistically significant.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, Obesity
Abstract: E1546
Type: Eposter Presentation
Background
Obesity is an increasingly important health problem in developed countries and a cause of variability in treatment outcomes. The effect of being owerweight or obese had been studied in various populations in patients undergoing Allo-HSCT. Sorror et. al reported obesity as a factor in hemetopoietic cell transplant-specific comorbidity index and increased risk of non-relapse mortality (NRM).
Aims
In this study, we evaluated the impact of obesity on acute graft vs host disease (aGVHD) risk, overall survival (OS), relapse rate (RR), relapse free survival (RFS) and NRM in patients undergoing Allo-HSCT.
Methods
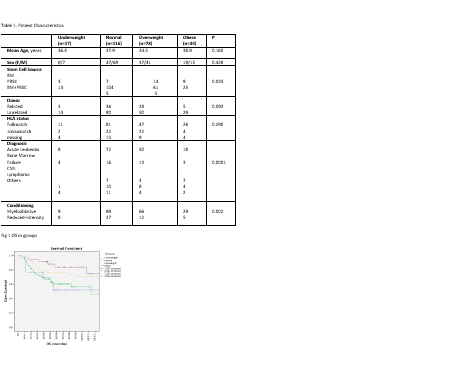
Retrospectively, 245 patients who underwent allo-HSCT between 2000 and 2015 at Ankara University School of Medicine was included in our study. Patients were classified into four groups based on pretransplant BMI values according to World Health Organization as follows: underweight (BMI < 18.5 kg/m2, n=17), normal (18.5 ≤ BMI < 25 mg/kg/m2, n=116), overweight (25 ≤ BMI < 30 mg/kg/m2, n=78) and obese (BMI ≥ 30 mg/kg/m2, n=34). Patients received weight adjusted chemotherapy doses. Characteristics of patients were compared using the Chi-squared test for categorical variables. The probilibity of OS was calculated by the Kaplan-Meier method.
Results
The patient characteristics are given in the table. Mean age of the group was 36.8 (range, 16-71). Overweight and obese patients received more bone marrow as a stem cell source (P=0.033). Bone marrow failure syndromes were more common diagnosis in normal and underweight recipients (p=0.0001). Myeloablative conditioning were prefered in overweight and obese group (p=0.002). Five year OS in underweight, normal, overweight and obese groups were as follows: 51%, 60%, 74% and 83% (P=0.005). Relaps rate was higher in underweight and normal compared to overweight and obese but not statistically different (23% vs 19%, P=0.53). 2-year RFS in underweight, normal, overweight and obese groups were as follows: 33%, 29%, 41%, 50%, P=0.069). The incidence of aGVHD detected higher in obese and overweight group however not statistically significant (44% vs 40%, p=0.6). NRM was lower in overweight and obese group (12% vs 31%, P=0.001).
Conclusion
Interestingly, we have demostrated that being overweight/obese improved OS and decreased NRM in our cohort. Relapse rate was higher in underweight and normal weight group however not statistically significant.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, Obesity
Type: Eposter Presentation
Background
Obesity is an increasingly important health problem in developed countries and a cause of variability in treatment outcomes. The effect of being owerweight or obese had been studied in various populations in patients undergoing Allo-HSCT. Sorror et. al reported obesity as a factor in hemetopoietic cell transplant-specific comorbidity index and increased risk of non-relapse mortality (NRM).
Aims
In this study, we evaluated the impact of obesity on acute graft vs host disease (aGVHD) risk, overall survival (OS), relapse rate (RR), relapse free survival (RFS) and NRM in patients undergoing Allo-HSCT.
Methods
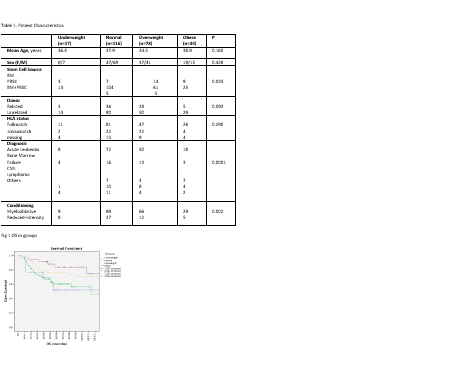
Retrospectively, 245 patients who underwent allo-HSCT between 2000 and 2015 at Ankara University School of Medicine was included in our study. Patients were classified into four groups based on pretransplant BMI values according to World Health Organization as follows: underweight (BMI < 18.5 kg/m2, n=17), normal (18.5 ≤ BMI < 25 mg/kg/m2, n=116), overweight (25 ≤ BMI < 30 mg/kg/m2, n=78) and obese (BMI ≥ 30 mg/kg/m2, n=34). Patients received weight adjusted chemotherapy doses. Characteristics of patients were compared using the Chi-squared test for categorical variables. The probilibity of OS was calculated by the Kaplan-Meier method.
Results
The patient characteristics are given in the table. Mean age of the group was 36.8 (range, 16-71). Overweight and obese patients received more bone marrow as a stem cell source (P=0.033). Bone marrow failure syndromes were more common diagnosis in normal and underweight recipients (p=0.0001). Myeloablative conditioning were prefered in overweight and obese group (p=0.002). Five year OS in underweight, normal, overweight and obese groups were as follows: 51%, 60%, 74% and 83% (P=0.005). Relaps rate was higher in underweight and normal compared to overweight and obese but not statistically different (23% vs 19%, P=0.53). 2-year RFS in underweight, normal, overweight and obese groups were as follows: 33%, 29%, 41%, 50%, P=0.069). The incidence of aGVHD detected higher in obese and overweight group however not statistically significant (44% vs 40%, p=0.6). NRM was lower in overweight and obese group (12% vs 31%, P=0.001).
Conclusion
Interestingly, we have demostrated that being overweight/obese improved OS and decreased NRM in our cohort. Relapse rate was higher in underweight and normal weight group however not statistically significant.
Session topic: E-poster
Keyword(s): Allogeneic hematopoietic stem cell transplant, Obesity
{{ help_message }}
{{filter}}


