IMPACT OF PLERIXAFOR ON HOSPITAL EFFICIENCY: A SINGLE CENTER EXPERIENCE
(Abstract release date: 05/19/16)
EHA Library. Azar N. 06/09/16; 133091; E1542

Dr. Nabih Azar
Contributions
Contributions
Abstract
Abstract: E1542
Type: Eposter Presentation
Background
Plerixafor in combination with granulocyte colony-stimulating factor (G-CSF) has shown to increase mobilization of peripheral blood stem cells (PBSC) as compared to G-CSF alone in patients undergoing autologous stem cell transplantation (ASCT). However, up to 25% of patients treated with G-CSF alone still fail mobilization. Adding plerixafor to the regimen of poor mobilizers allows to rescue these patients from mobilization failure and to reduce the number of apheresis sessions. Furthermore, it was hypothesized that the use of plerixafor would lead to a better prediction of the number of apheresis time-slots needed and a reduction of time-slots lost. This in turn would free hospital resources which could be dedicated to other procedures.
Aims
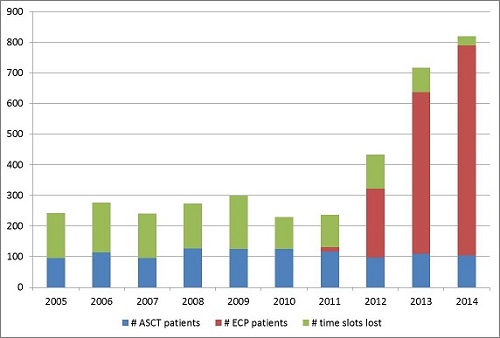
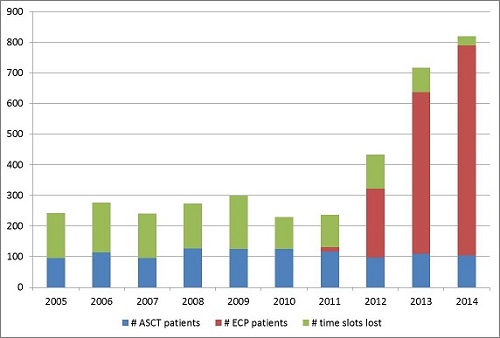
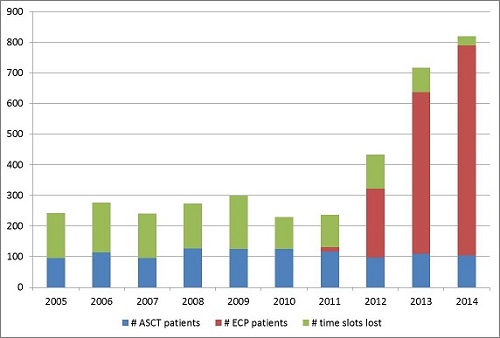
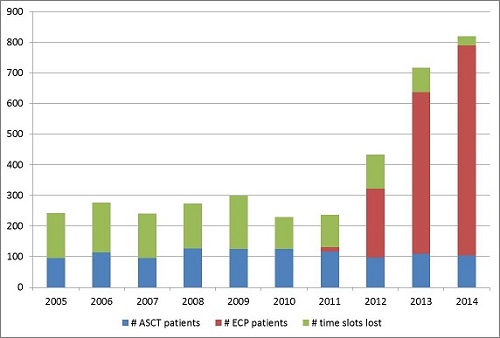
The goal of this retrospective study was to capture the impact of plerixafor on mobilization outcome and on the efficiency of the apheresis department. Efficiency was described in terms of time-slots lost and the number of extracorporeal photopheresis (ECP) sessions carried out. ECP, whose benefit is generally recognized in patients with cutaneous T-cell lymphoma and graft versus host disease, is a procedure which carries some similarities with standard apheresis techniques and may therefore be carried out by the same staff provided some additional training. The demand for this procedure has steadily increased over the last years, but could not be matched by available health care resources.
Methods
Hospital records of patients treated before (2005-2008) and after (2009-2014) introduction of plerixafor were collected and analyzed retrospectively. Main outcomes were mobilization failure rate and number of time-slots lost due to insufficient mobilization, ie low CD34 count. Secondary endpoints included the number of apheresis sessions per patient, mean CD34+ cells collected, the number of ASCT and ECP sessions carried out, and costs per ASCT patient.
Results
Following plerixafor introduction, the mobilization failure rate dropped from 12% to 4% and the mean number of time-slots lost per patient dropped from 1.39 to 0.89. Additional drug costs due to plerixafor were partially balanced by a reduction in apheresis sessions, resulting in an additional cost of 700 € per ASCT candidate. More importantly, with the use of plerixafor, the availability of time-slots turned from erratic to predictable such that freed capacity could be dedicated to other apheresis procedures, and the number of ECP sessions increased from 0 in 2005 to 685 sessions in 2014 (see Figure).
Conclusion
Plerixafor not only improved mobilization outcomes for patients undergoing ASCT, but also reduced uncertainty around scheduling of apheresis sessions, leading to a decrease in time-slots lost. Freed resources were used to manage patients requiring ECP therapy, showing that the introduction of plerixafor had much wider implications beyond that of improvement in PBSC mobilization. Even though this result is not generalizable, in a climate of stretched resources it is important to consider the opportunity and redistribution investment possible with freed capacities.
Session topic: E-poster
Keyword(s): Apheresis, Autologous stem cell collection, Extracorporeal photopheresis, Peripheral blood stem cell mobilization
Type: Eposter Presentation
Background
Plerixafor in combination with granulocyte colony-stimulating factor (G-CSF) has shown to increase mobilization of peripheral blood stem cells (PBSC) as compared to G-CSF alone in patients undergoing autologous stem cell transplantation (ASCT). However, up to 25% of patients treated with G-CSF alone still fail mobilization. Adding plerixafor to the regimen of poor mobilizers allows to rescue these patients from mobilization failure and to reduce the number of apheresis sessions. Furthermore, it was hypothesized that the use of plerixafor would lead to a better prediction of the number of apheresis time-slots needed and a reduction of time-slots lost. This in turn would free hospital resources which could be dedicated to other procedures.
Aims
The goal of this retrospective study was to capture the impact of plerixafor on mobilization outcome and on the efficiency of the apheresis department. Efficiency was described in terms of time-slots lost and the number of extracorporeal photopheresis (ECP) sessions carried out. ECP, whose benefit is generally recognized in patients with cutaneous T-cell lymphoma and graft versus host disease, is a procedure which carries some similarities with standard apheresis techniques and may therefore be carried out by the same staff provided some additional training. The demand for this procedure has steadily increased over the last years, but could not be matched by available health care resources.
Methods
Hospital records of patients treated before (2005-2008) and after (2009-2014) introduction of plerixafor were collected and analyzed retrospectively. Main outcomes were mobilization failure rate and number of time-slots lost due to insufficient mobilization, ie low CD34 count. Secondary endpoints included the number of apheresis sessions per patient, mean CD34+ cells collected, the number of ASCT and ECP sessions carried out, and costs per ASCT patient.
Results
Following plerixafor introduction, the mobilization failure rate dropped from 12% to 4% and the mean number of time-slots lost per patient dropped from 1.39 to 0.89. Additional drug costs due to plerixafor were partially balanced by a reduction in apheresis sessions, resulting in an additional cost of 700 € per ASCT candidate. More importantly, with the use of plerixafor, the availability of time-slots turned from erratic to predictable such that freed capacity could be dedicated to other apheresis procedures, and the number of ECP sessions increased from 0 in 2005 to 685 sessions in 2014 (see Figure).
Conclusion
Plerixafor not only improved mobilization outcomes for patients undergoing ASCT, but also reduced uncertainty around scheduling of apheresis sessions, leading to a decrease in time-slots lost. Freed resources were used to manage patients requiring ECP therapy, showing that the introduction of plerixafor had much wider implications beyond that of improvement in PBSC mobilization. Even though this result is not generalizable, in a climate of stretched resources it is important to consider the opportunity and redistribution investment possible with freed capacities.
Session topic: E-poster
Keyword(s): Apheresis, Autologous stem cell collection, Extracorporeal photopheresis, Peripheral blood stem cell mobilization
Abstract: E1542
Type: Eposter Presentation
Background
Plerixafor in combination with granulocyte colony-stimulating factor (G-CSF) has shown to increase mobilization of peripheral blood stem cells (PBSC) as compared to G-CSF alone in patients undergoing autologous stem cell transplantation (ASCT). However, up to 25% of patients treated with G-CSF alone still fail mobilization. Adding plerixafor to the regimen of poor mobilizers allows to rescue these patients from mobilization failure and to reduce the number of apheresis sessions. Furthermore, it was hypothesized that the use of plerixafor would lead to a better prediction of the number of apheresis time-slots needed and a reduction of time-slots lost. This in turn would free hospital resources which could be dedicated to other procedures.
Aims
The goal of this retrospective study was to capture the impact of plerixafor on mobilization outcome and on the efficiency of the apheresis department. Efficiency was described in terms of time-slots lost and the number of extracorporeal photopheresis (ECP) sessions carried out. ECP, whose benefit is generally recognized in patients with cutaneous T-cell lymphoma and graft versus host disease, is a procedure which carries some similarities with standard apheresis techniques and may therefore be carried out by the same staff provided some additional training. The demand for this procedure has steadily increased over the last years, but could not be matched by available health care resources.
Methods
Hospital records of patients treated before (2005-2008) and after (2009-2014) introduction of plerixafor were collected and analyzed retrospectively. Main outcomes were mobilization failure rate and number of time-slots lost due to insufficient mobilization, ie low CD34 count. Secondary endpoints included the number of apheresis sessions per patient, mean CD34+ cells collected, the number of ASCT and ECP sessions carried out, and costs per ASCT patient.
Results
Following plerixafor introduction, the mobilization failure rate dropped from 12% to 4% and the mean number of time-slots lost per patient dropped from 1.39 to 0.89. Additional drug costs due to plerixafor were partially balanced by a reduction in apheresis sessions, resulting in an additional cost of 700 € per ASCT candidate. More importantly, with the use of plerixafor, the availability of time-slots turned from erratic to predictable such that freed capacity could be dedicated to other apheresis procedures, and the number of ECP sessions increased from 0 in 2005 to 685 sessions in 2014 (see Figure).
Conclusion
Plerixafor not only improved mobilization outcomes for patients undergoing ASCT, but also reduced uncertainty around scheduling of apheresis sessions, leading to a decrease in time-slots lost. Freed resources were used to manage patients requiring ECP therapy, showing that the introduction of plerixafor had much wider implications beyond that of improvement in PBSC mobilization. Even though this result is not generalizable, in a climate of stretched resources it is important to consider the opportunity and redistribution investment possible with freed capacities.
Session topic: E-poster
Keyword(s): Apheresis, Autologous stem cell collection, Extracorporeal photopheresis, Peripheral blood stem cell mobilization
Type: Eposter Presentation
Background
Plerixafor in combination with granulocyte colony-stimulating factor (G-CSF) has shown to increase mobilization of peripheral blood stem cells (PBSC) as compared to G-CSF alone in patients undergoing autologous stem cell transplantation (ASCT). However, up to 25% of patients treated with G-CSF alone still fail mobilization. Adding plerixafor to the regimen of poor mobilizers allows to rescue these patients from mobilization failure and to reduce the number of apheresis sessions. Furthermore, it was hypothesized that the use of plerixafor would lead to a better prediction of the number of apheresis time-slots needed and a reduction of time-slots lost. This in turn would free hospital resources which could be dedicated to other procedures.
Aims
The goal of this retrospective study was to capture the impact of plerixafor on mobilization outcome and on the efficiency of the apheresis department. Efficiency was described in terms of time-slots lost and the number of extracorporeal photopheresis (ECP) sessions carried out. ECP, whose benefit is generally recognized in patients with cutaneous T-cell lymphoma and graft versus host disease, is a procedure which carries some similarities with standard apheresis techniques and may therefore be carried out by the same staff provided some additional training. The demand for this procedure has steadily increased over the last years, but could not be matched by available health care resources.
Methods
Hospital records of patients treated before (2005-2008) and after (2009-2014) introduction of plerixafor were collected and analyzed retrospectively. Main outcomes were mobilization failure rate and number of time-slots lost due to insufficient mobilization, ie low CD34 count. Secondary endpoints included the number of apheresis sessions per patient, mean CD34+ cells collected, the number of ASCT and ECP sessions carried out, and costs per ASCT patient.
Results
Following plerixafor introduction, the mobilization failure rate dropped from 12% to 4% and the mean number of time-slots lost per patient dropped from 1.39 to 0.89. Additional drug costs due to plerixafor were partially balanced by a reduction in apheresis sessions, resulting in an additional cost of 700 € per ASCT candidate. More importantly, with the use of plerixafor, the availability of time-slots turned from erratic to predictable such that freed capacity could be dedicated to other apheresis procedures, and the number of ECP sessions increased from 0 in 2005 to 685 sessions in 2014 (see Figure).
Conclusion
Plerixafor not only improved mobilization outcomes for patients undergoing ASCT, but also reduced uncertainty around scheduling of apheresis sessions, leading to a decrease in time-slots lost. Freed resources were used to manage patients requiring ECP therapy, showing that the introduction of plerixafor had much wider implications beyond that of improvement in PBSC mobilization. Even though this result is not generalizable, in a climate of stretched resources it is important to consider the opportunity and redistribution investment possible with freed capacities.
Session topic: E-poster
Keyword(s): Apheresis, Autologous stem cell collection, Extracorporeal photopheresis, Peripheral blood stem cell mobilization
{{ help_message }}
{{filter}}


