HCT.CI PREDICTS MORBI-MORTALITY IN AUTOLOGOUS STEM CELL TRANSPLANTATION
(Abstract release date: 05/19/16)
EHA Library. Berro M. 06/09/16; 133083; E1534

Dr. Mariano Berro
Contributions
Contributions
Abstract
Abstract: E1534
Type: Eposter Presentation
Background
Hematopoietic Stem Cell Transplant Comorbidity Index (HCT.CI) score, described by Sorror, is a useful tool to assess the risk for Non Relapse Mortality (NRM) after Allogeneic HSCT. The impact of this score in Autologous HSCT is still to be confirmed.
Aims
To determine the impact of HCT.Ci score in the morbidity and mortality after autologous HSCT, assessing the 100 day morbidity defined as orothraqueal intubation (OTI), dialysis or vasopressors need, early mortality (before day 100) and long term NRM.
Methods
We retrospectively reviewed 473 medical records of patients that received an autologous HSCT in our centres between October 2002 and September 2015. Median age was 49 years (range 1-74 years), 58% were male, prevalent diseases were Multiple Myeloma (37%), Non Hodgkin Lymphoma (26%) and Hodgkin Lymphoma (20%), 29% were in complete remission, 42% received one chemotherapy scheme before transplant, 46% two schemes and 12% three or more (heavily pre-treated). Regarding comorbidities, 42% had low risk (LR) HCT.CI (score 0), 47% intermediate risk (IR) (1-2) and 12% high risk (HR) (≥3). For univariate analysis we use Chi2 for dichotomic variables, Kaplan-Meier for Overall Survival (OS) and cumulative incidence for NRM; for multivariate analysis we used logistic regression for dichotomic and Cox regression for time dependant variables.
Results
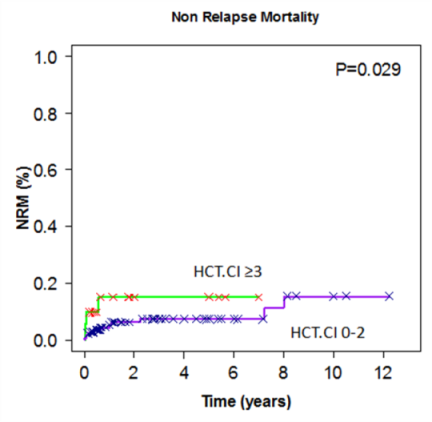
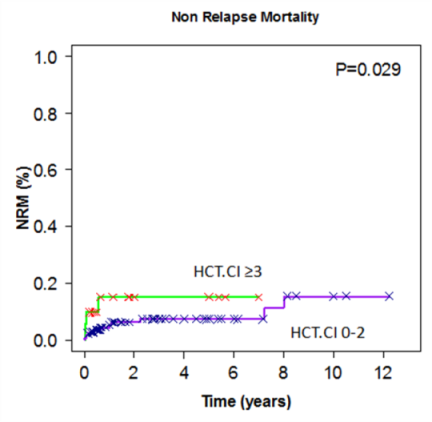
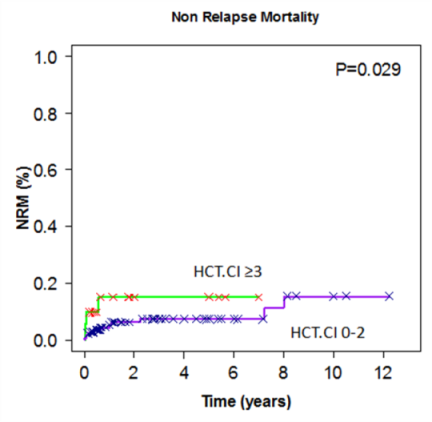
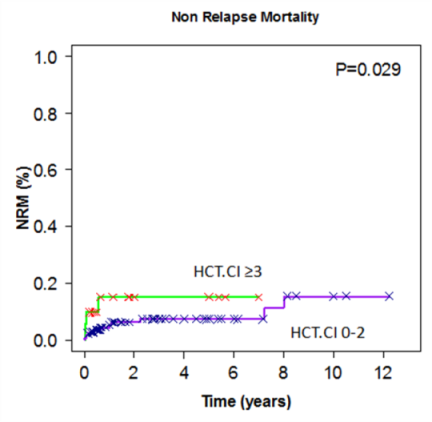
Median follow up was 1.3 years. Early mortality (day 100) was 4.4%, 9% required OTI, 8.5% vassopresors and 2.2% dialysis, 1-3 years NRM and OS were 7-9% and 85-79% respectively. High risk HCT.Ci patients had a significant increase in 100 day mortality compared to low and intermediate risk (11% vs. 4.1% vs. 2.6% respectively, p=0.02), OTI (18% vs. 8% vs. 7%, p=0.02), dialysis (9% vs.2% vs. 0.5%, p=0.001) and NRM (1-3 years HR vs. LR/IR 15-15% vs. 5-7%, p=0.02) (figure 1). After multivariate analysis these outcomes remain significant (comparing HR vs. LR/IR): early mortality (OR 3.4, 95% CI 1.1-10.4), OTI (OR 2.9, 95% CI 1.3-6.7), dialysis (OR 8.8, 95% CI 2.4-32.6) and NRM (OR 2.6, 95% CI 1.05-6.6). Other than comorbidities, Multiple Myeloma patients had a significant reduction in NRM (OR 0.25, 95% CI 0.1-0.8) and OTI (OR 0.28, 95% CI 0.1-0.83); patients older than 60 years had a significant increase in NRM (OR 4.6, 95% CI 2.1-10.5) and heavily pre-treated patients had a significant increase in NRM (OR 3.3, 95% CI 1.4-7.9) and OTI (OR 2.4, 95% CI 1.1-5.6).
Conclusion
We observed that HCT.CI had a significant impact on Autologous HSCT treatment related mortality basically due to early toxicity express as 100 day mortality and the three main morbidity outcomes. This observation should be confirmed in larger series.
Session topic: E-poster
Keyword(s): Autologous hematopoietic stem cell transplantation, Comorbidities, Transplant-related mortality
Type: Eposter Presentation
Background
Hematopoietic Stem Cell Transplant Comorbidity Index (HCT.CI) score, described by Sorror, is a useful tool to assess the risk for Non Relapse Mortality (NRM) after Allogeneic HSCT. The impact of this score in Autologous HSCT is still to be confirmed.
Aims
To determine the impact of HCT.Ci score in the morbidity and mortality after autologous HSCT, assessing the 100 day morbidity defined as orothraqueal intubation (OTI), dialysis or vasopressors need, early mortality (before day 100) and long term NRM.
Methods
We retrospectively reviewed 473 medical records of patients that received an autologous HSCT in our centres between October 2002 and September 2015. Median age was 49 years (range 1-74 years), 58% were male, prevalent diseases were Multiple Myeloma (37%), Non Hodgkin Lymphoma (26%) and Hodgkin Lymphoma (20%), 29% were in complete remission, 42% received one chemotherapy scheme before transplant, 46% two schemes and 12% three or more (heavily pre-treated). Regarding comorbidities, 42% had low risk (LR) HCT.CI (score 0), 47% intermediate risk (IR) (1-2) and 12% high risk (HR) (≥3). For univariate analysis we use Chi2 for dichotomic variables, Kaplan-Meier for Overall Survival (OS) and cumulative incidence for NRM; for multivariate analysis we used logistic regression for dichotomic and Cox regression for time dependant variables.
Results
Median follow up was 1.3 years. Early mortality (day 100) was 4.4%, 9% required OTI, 8.5% vassopresors and 2.2% dialysis, 1-3 years NRM and OS were 7-9% and 85-79% respectively. High risk HCT.Ci patients had a significant increase in 100 day mortality compared to low and intermediate risk (11% vs. 4.1% vs. 2.6% respectively, p=0.02), OTI (18% vs. 8% vs. 7%, p=0.02), dialysis (9% vs.2% vs. 0.5%, p=0.001) and NRM (1-3 years HR vs. LR/IR 15-15% vs. 5-7%, p=0.02) (figure 1). After multivariate analysis these outcomes remain significant (comparing HR vs. LR/IR): early mortality (OR 3.4, 95% CI 1.1-10.4), OTI (OR 2.9, 95% CI 1.3-6.7), dialysis (OR 8.8, 95% CI 2.4-32.6) and NRM (OR 2.6, 95% CI 1.05-6.6). Other than comorbidities, Multiple Myeloma patients had a significant reduction in NRM (OR 0.25, 95% CI 0.1-0.8) and OTI (OR 0.28, 95% CI 0.1-0.83); patients older than 60 years had a significant increase in NRM (OR 4.6, 95% CI 2.1-10.5) and heavily pre-treated patients had a significant increase in NRM (OR 3.3, 95% CI 1.4-7.9) and OTI (OR 2.4, 95% CI 1.1-5.6).
Conclusion
We observed that HCT.CI had a significant impact on Autologous HSCT treatment related mortality basically due to early toxicity express as 100 day mortality and the three main morbidity outcomes. This observation should be confirmed in larger series.
Session topic: E-poster
Keyword(s): Autologous hematopoietic stem cell transplantation, Comorbidities, Transplant-related mortality
Abstract: E1534
Type: Eposter Presentation
Background
Hematopoietic Stem Cell Transplant Comorbidity Index (HCT.CI) score, described by Sorror, is a useful tool to assess the risk for Non Relapse Mortality (NRM) after Allogeneic HSCT. The impact of this score in Autologous HSCT is still to be confirmed.
Aims
To determine the impact of HCT.Ci score in the morbidity and mortality after autologous HSCT, assessing the 100 day morbidity defined as orothraqueal intubation (OTI), dialysis or vasopressors need, early mortality (before day 100) and long term NRM.
Methods
We retrospectively reviewed 473 medical records of patients that received an autologous HSCT in our centres between October 2002 and September 2015. Median age was 49 years (range 1-74 years), 58% were male, prevalent diseases were Multiple Myeloma (37%), Non Hodgkin Lymphoma (26%) and Hodgkin Lymphoma (20%), 29% were in complete remission, 42% received one chemotherapy scheme before transplant, 46% two schemes and 12% three or more (heavily pre-treated). Regarding comorbidities, 42% had low risk (LR) HCT.CI (score 0), 47% intermediate risk (IR) (1-2) and 12% high risk (HR) (≥3). For univariate analysis we use Chi2 for dichotomic variables, Kaplan-Meier for Overall Survival (OS) and cumulative incidence for NRM; for multivariate analysis we used logistic regression for dichotomic and Cox regression for time dependant variables.
Results
Median follow up was 1.3 years. Early mortality (day 100) was 4.4%, 9% required OTI, 8.5% vassopresors and 2.2% dialysis, 1-3 years NRM and OS were 7-9% and 85-79% respectively. High risk HCT.Ci patients had a significant increase in 100 day mortality compared to low and intermediate risk (11% vs. 4.1% vs. 2.6% respectively, p=0.02), OTI (18% vs. 8% vs. 7%, p=0.02), dialysis (9% vs.2% vs. 0.5%, p=0.001) and NRM (1-3 years HR vs. LR/IR 15-15% vs. 5-7%, p=0.02) (figure 1). After multivariate analysis these outcomes remain significant (comparing HR vs. LR/IR): early mortality (OR 3.4, 95% CI 1.1-10.4), OTI (OR 2.9, 95% CI 1.3-6.7), dialysis (OR 8.8, 95% CI 2.4-32.6) and NRM (OR 2.6, 95% CI 1.05-6.6). Other than comorbidities, Multiple Myeloma patients had a significant reduction in NRM (OR 0.25, 95% CI 0.1-0.8) and OTI (OR 0.28, 95% CI 0.1-0.83); patients older than 60 years had a significant increase in NRM (OR 4.6, 95% CI 2.1-10.5) and heavily pre-treated patients had a significant increase in NRM (OR 3.3, 95% CI 1.4-7.9) and OTI (OR 2.4, 95% CI 1.1-5.6).
Conclusion
We observed that HCT.CI had a significant impact on Autologous HSCT treatment related mortality basically due to early toxicity express as 100 day mortality and the three main morbidity outcomes. This observation should be confirmed in larger series.
Session topic: E-poster
Keyword(s): Autologous hematopoietic stem cell transplantation, Comorbidities, Transplant-related mortality
Type: Eposter Presentation
Background
Hematopoietic Stem Cell Transplant Comorbidity Index (HCT.CI) score, described by Sorror, is a useful tool to assess the risk for Non Relapse Mortality (NRM) after Allogeneic HSCT. The impact of this score in Autologous HSCT is still to be confirmed.
Aims
To determine the impact of HCT.Ci score in the morbidity and mortality after autologous HSCT, assessing the 100 day morbidity defined as orothraqueal intubation (OTI), dialysis or vasopressors need, early mortality (before day 100) and long term NRM.
Methods
We retrospectively reviewed 473 medical records of patients that received an autologous HSCT in our centres between October 2002 and September 2015. Median age was 49 years (range 1-74 years), 58% were male, prevalent diseases were Multiple Myeloma (37%), Non Hodgkin Lymphoma (26%) and Hodgkin Lymphoma (20%), 29% were in complete remission, 42% received one chemotherapy scheme before transplant, 46% two schemes and 12% three or more (heavily pre-treated). Regarding comorbidities, 42% had low risk (LR) HCT.CI (score 0), 47% intermediate risk (IR) (1-2) and 12% high risk (HR) (≥3). For univariate analysis we use Chi2 for dichotomic variables, Kaplan-Meier for Overall Survival (OS) and cumulative incidence for NRM; for multivariate analysis we used logistic regression for dichotomic and Cox regression for time dependant variables.
Results
Median follow up was 1.3 years. Early mortality (day 100) was 4.4%, 9% required OTI, 8.5% vassopresors and 2.2% dialysis, 1-3 years NRM and OS were 7-9% and 85-79% respectively. High risk HCT.Ci patients had a significant increase in 100 day mortality compared to low and intermediate risk (11% vs. 4.1% vs. 2.6% respectively, p=0.02), OTI (18% vs. 8% vs. 7%, p=0.02), dialysis (9% vs.2% vs. 0.5%, p=0.001) and NRM (1-3 years HR vs. LR/IR 15-15% vs. 5-7%, p=0.02) (figure 1). After multivariate analysis these outcomes remain significant (comparing HR vs. LR/IR): early mortality (OR 3.4, 95% CI 1.1-10.4), OTI (OR 2.9, 95% CI 1.3-6.7), dialysis (OR 8.8, 95% CI 2.4-32.6) and NRM (OR 2.6, 95% CI 1.05-6.6). Other than comorbidities, Multiple Myeloma patients had a significant reduction in NRM (OR 0.25, 95% CI 0.1-0.8) and OTI (OR 0.28, 95% CI 0.1-0.83); patients older than 60 years had a significant increase in NRM (OR 4.6, 95% CI 2.1-10.5) and heavily pre-treated patients had a significant increase in NRM (OR 3.3, 95% CI 1.4-7.9) and OTI (OR 2.4, 95% CI 1.1-5.6).
Conclusion
We observed that HCT.CI had a significant impact on Autologous HSCT treatment related mortality basically due to early toxicity express as 100 day mortality and the three main morbidity outcomes. This observation should be confirmed in larger series.
Session topic: E-poster
Keyword(s): Autologous hematopoietic stem cell transplantation, Comorbidities, Transplant-related mortality
{{ help_message }}
{{filter}}


