THE IMPACT OF CARDIAC AND HEPATIC MRI ASSESSMENT ON THE CLINICAL MANAGEMENT OF AUSTRALIAN PATIENTS WITH TRANSFUSION-DEPENDENT ANEMIAS OR NON-TRANSFUSION-DEPENDENT THALASSEMIA IN THE TIMES STUDY
(Abstract release date: 05/19/16)
EHA Library. Ho P. 06/09/16; 133041; E1492
Disclosure(s): P J Ho: Honoraria, Membership on an entity’s Board of Directors or advisory committees and research
funding, Novartis and conference grant, Aspen; D Hiwase: Research funding, Celgene; N Viiala: Honoraria,
Novartis; E Zor and O L Gervasio: Employment, Novartis; D K Bowden: Research Funding, Novartis;
R Ramakrishna and D M Ross have no disclosures to declare

Dr. Phoebe Joy Ho
Contributions
Contributions
Abstract
Abstract: E1492
Type: Eposter Presentation
Background
Iron overload can lead to impaired organ function and is associated with significant morbidity and mortality, the risks of which can be reduced by effective long-term iron chelation therapy (ICT) and control of iron loading. Magnetic resonance imaging (MRI) allows accurate, reproducible assessment of iron load and its use may affect clinical management decisions, leading to improved patient care. The epidemiological TIMES study used MRI to assess prevalence and severity of cardiac and hepatic siderosis in a large population of Australian patients with transfusion-dependent anemia or non-transfusion-dependent thalassemia (NTDT). In this analysis of the TIMES study, we report the impact of MRI results on investigator treatment decisions.
Aims
To determine the prevalence of iron overload by MRI and its impact on the clinical management of iron overload in a population of patients with transfusion-dependent anemia or NTDT.
Methods
Patients with thalassemia major (TM), NTDT (β thalassemia intermedia, β thalassemia/Hb E, Hb H disease), myelodysplastic syndromes (MDS) or other chronic anemias were enrolled. Patients with NTDT had serum ferritin (SF) >300 ng/mL; others had a lifetime history of ≥20 units red blood cell (RBC) transfusions and SF >500 ng/mL. Past medical history was collected (including red blood cell (RBC) transfusion, ICT and hematologic data). Prospective MRI (FerriScan) was used to determine R2 liver iron concentration (LIC) and myocardial T2* (mT2*). Treatment decisions were assessed and recorded using an investigator questionnaire after evaluation of patient MRI results.
Results
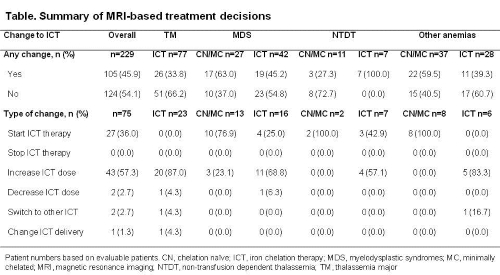
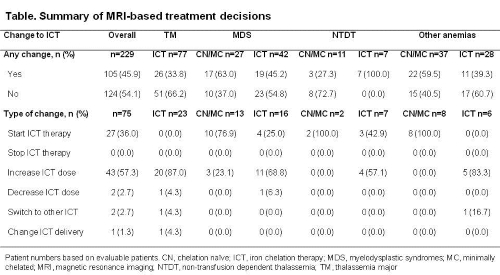
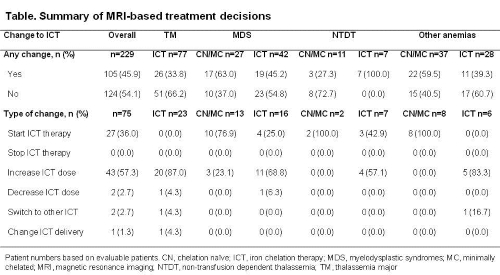
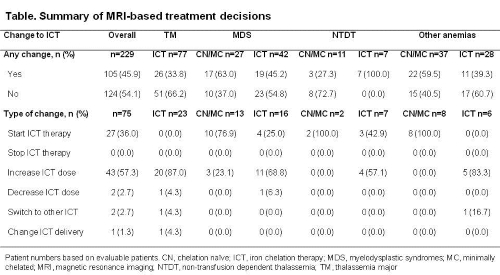
Of the 243 enrolled patients, 10 and 48% had cardiac and hepatic siderosis, respectively. In all disease groups, mean LIC was above the target range (3–7 mg Fe/g dw), while mean mT2* was normal (≥20 ms). 65.8% of patients received ICT for ≥1 month before or during the study. During the 12-month period prior to the study, 55.9% received deferasirox, 11.9% received deferoxamine and 2.5% received deferiprone. All patients with TM had received ICT; among patients with MDS, NTDT or other anemia types, some patients were chelation naïve (CN)/minimally chelated (MC, chelation <1 month in lifetime; Table). MRI assessment led to a change in management in 105 (45.9) of all evaluable patients (n=229) and in ~60% of CN/MC patients with MDS (17/27 [63.0%]) and other anemias (22/37 [59.5%]; Table). Across all diseases, the predominant changes were increasing chelator dose (43/75 [57.3%]) and starting chelation (27/75 [36.0%]; Table). In patients who had received ICT for >1 month, the most frequent change was increasing chelator dose (TM, 20/23 [87.0%]; MDS, 11/16 [68.8%]; NTDT, 4/7 [57.1%]; other anemias, 5/6 [83.3%]). In CN/MC patients, starting ICT was the predominant change (MDS, 10/13 [76.9%]; NTDT, 2/2 [100.0%]; other anemias, 8/8 [100.0%]). Cardiac MRI assessment (mT2*) was the key driver for ICT decisions in patients with TM (63.8%; ranked as the most important factor in the treatment decision); however, LIC was the key determinant in patients with MDS (42.0), NTDT (44.4%) and other anemias (56.3%).
Conclusion
These data provide real-life insight into the impact of MRI on treatment decisions in a large population of patients with heterogeneous causes of chronic anemia receiving RBC transfusions. A change in ICT management due to MRI analysis occurred in nearly half of all patients. This emphasizes the importance of accurate monitoring of iron load in patients with transfusion-dependent anemias or NTDT to allow for informed clinical decision making.
Session topic: E-poster
Keyword(s): Clinical data, Iron chelation, Iron overload, Magnetic resonance imaging
Type: Eposter Presentation
Background
Iron overload can lead to impaired organ function and is associated with significant morbidity and mortality, the risks of which can be reduced by effective long-term iron chelation therapy (ICT) and control of iron loading. Magnetic resonance imaging (MRI) allows accurate, reproducible assessment of iron load and its use may affect clinical management decisions, leading to improved patient care. The epidemiological TIMES study used MRI to assess prevalence and severity of cardiac and hepatic siderosis in a large population of Australian patients with transfusion-dependent anemia or non-transfusion-dependent thalassemia (NTDT). In this analysis of the TIMES study, we report the impact of MRI results on investigator treatment decisions.
Aims
To determine the prevalence of iron overload by MRI and its impact on the clinical management of iron overload in a population of patients with transfusion-dependent anemia or NTDT.
Methods
Patients with thalassemia major (TM), NTDT (β thalassemia intermedia, β thalassemia/Hb E, Hb H disease), myelodysplastic syndromes (MDS) or other chronic anemias were enrolled. Patients with NTDT had serum ferritin (SF) >300 ng/mL; others had a lifetime history of ≥20 units red blood cell (RBC) transfusions and SF >500 ng/mL. Past medical history was collected (including red blood cell (RBC) transfusion, ICT and hematologic data). Prospective MRI (FerriScan) was used to determine R2 liver iron concentration (LIC) and myocardial T2* (mT2*). Treatment decisions were assessed and recorded using an investigator questionnaire after evaluation of patient MRI results.
Results
Of the 243 enrolled patients, 10 and 48% had cardiac and hepatic siderosis, respectively. In all disease groups, mean LIC was above the target range (3–7 mg Fe/g dw), while mean mT2* was normal (≥20 ms). 65.8% of patients received ICT for ≥1 month before or during the study. During the 12-month period prior to the study, 55.9% received deferasirox, 11.9% received deferoxamine and 2.5% received deferiprone. All patients with TM had received ICT; among patients with MDS, NTDT or other anemia types, some patients were chelation naïve (CN)/minimally chelated (MC, chelation <1 month in lifetime; Table). MRI assessment led to a change in management in 105 (45.9) of all evaluable patients (n=229) and in ~60% of CN/MC patients with MDS (17/27 [63.0%]) and other anemias (22/37 [59.5%]; Table). Across all diseases, the predominant changes were increasing chelator dose (43/75 [57.3%]) and starting chelation (27/75 [36.0%]; Table). In patients who had received ICT for >1 month, the most frequent change was increasing chelator dose (TM, 20/23 [87.0%]; MDS, 11/16 [68.8%]; NTDT, 4/7 [57.1%]; other anemias, 5/6 [83.3%]). In CN/MC patients, starting ICT was the predominant change (MDS, 10/13 [76.9%]; NTDT, 2/2 [100.0%]; other anemias, 8/8 [100.0%]). Cardiac MRI assessment (mT2*) was the key driver for ICT decisions in patients with TM (63.8%; ranked as the most important factor in the treatment decision); however, LIC was the key determinant in patients with MDS (42.0), NTDT (44.4%) and other anemias (56.3%).
Conclusion
These data provide real-life insight into the impact of MRI on treatment decisions in a large population of patients with heterogeneous causes of chronic anemia receiving RBC transfusions. A change in ICT management due to MRI analysis occurred in nearly half of all patients. This emphasizes the importance of accurate monitoring of iron load in patients with transfusion-dependent anemias or NTDT to allow for informed clinical decision making.
Session topic: E-poster
Keyword(s): Clinical data, Iron chelation, Iron overload, Magnetic resonance imaging
Abstract: E1492
Type: Eposter Presentation
Background
Iron overload can lead to impaired organ function and is associated with significant morbidity and mortality, the risks of which can be reduced by effective long-term iron chelation therapy (ICT) and control of iron loading. Magnetic resonance imaging (MRI) allows accurate, reproducible assessment of iron load and its use may affect clinical management decisions, leading to improved patient care. The epidemiological TIMES study used MRI to assess prevalence and severity of cardiac and hepatic siderosis in a large population of Australian patients with transfusion-dependent anemia or non-transfusion-dependent thalassemia (NTDT). In this analysis of the TIMES study, we report the impact of MRI results on investigator treatment decisions.
Aims
To determine the prevalence of iron overload by MRI and its impact on the clinical management of iron overload in a population of patients with transfusion-dependent anemia or NTDT.
Methods
Patients with thalassemia major (TM), NTDT (β thalassemia intermedia, β thalassemia/Hb E, Hb H disease), myelodysplastic syndromes (MDS) or other chronic anemias were enrolled. Patients with NTDT had serum ferritin (SF) >300 ng/mL; others had a lifetime history of ≥20 units red blood cell (RBC) transfusions and SF >500 ng/mL. Past medical history was collected (including red blood cell (RBC) transfusion, ICT and hematologic data). Prospective MRI (FerriScan) was used to determine R2 liver iron concentration (LIC) and myocardial T2* (mT2*). Treatment decisions were assessed and recorded using an investigator questionnaire after evaluation of patient MRI results.
Results
Of the 243 enrolled patients, 10 and 48% had cardiac and hepatic siderosis, respectively. In all disease groups, mean LIC was above the target range (3–7 mg Fe/g dw), while mean mT2* was normal (≥20 ms). 65.8% of patients received ICT for ≥1 month before or during the study. During the 12-month period prior to the study, 55.9% received deferasirox, 11.9% received deferoxamine and 2.5% received deferiprone. All patients with TM had received ICT; among patients with MDS, NTDT or other anemia types, some patients were chelation naïve (CN)/minimally chelated (MC, chelation <1 month in lifetime; Table). MRI assessment led to a change in management in 105 (45.9) of all evaluable patients (n=229) and in ~60% of CN/MC patients with MDS (17/27 [63.0%]) and other anemias (22/37 [59.5%]; Table). Across all diseases, the predominant changes were increasing chelator dose (43/75 [57.3%]) and starting chelation (27/75 [36.0%]; Table). In patients who had received ICT for >1 month, the most frequent change was increasing chelator dose (TM, 20/23 [87.0%]; MDS, 11/16 [68.8%]; NTDT, 4/7 [57.1%]; other anemias, 5/6 [83.3%]). In CN/MC patients, starting ICT was the predominant change (MDS, 10/13 [76.9%]; NTDT, 2/2 [100.0%]; other anemias, 8/8 [100.0%]). Cardiac MRI assessment (mT2*) was the key driver for ICT decisions in patients with TM (63.8%; ranked as the most important factor in the treatment decision); however, LIC was the key determinant in patients with MDS (42.0), NTDT (44.4%) and other anemias (56.3%).
Conclusion
These data provide real-life insight into the impact of MRI on treatment decisions in a large population of patients with heterogeneous causes of chronic anemia receiving RBC transfusions. A change in ICT management due to MRI analysis occurred in nearly half of all patients. This emphasizes the importance of accurate monitoring of iron load in patients with transfusion-dependent anemias or NTDT to allow for informed clinical decision making.
Session topic: E-poster
Keyword(s): Clinical data, Iron chelation, Iron overload, Magnetic resonance imaging
Type: Eposter Presentation
Background
Iron overload can lead to impaired organ function and is associated with significant morbidity and mortality, the risks of which can be reduced by effective long-term iron chelation therapy (ICT) and control of iron loading. Magnetic resonance imaging (MRI) allows accurate, reproducible assessment of iron load and its use may affect clinical management decisions, leading to improved patient care. The epidemiological TIMES study used MRI to assess prevalence and severity of cardiac and hepatic siderosis in a large population of Australian patients with transfusion-dependent anemia or non-transfusion-dependent thalassemia (NTDT). In this analysis of the TIMES study, we report the impact of MRI results on investigator treatment decisions.
Aims
To determine the prevalence of iron overload by MRI and its impact on the clinical management of iron overload in a population of patients with transfusion-dependent anemia or NTDT.
Methods
Patients with thalassemia major (TM), NTDT (β thalassemia intermedia, β thalassemia/Hb E, Hb H disease), myelodysplastic syndromes (MDS) or other chronic anemias were enrolled. Patients with NTDT had serum ferritin (SF) >300 ng/mL; others had a lifetime history of ≥20 units red blood cell (RBC) transfusions and SF >500 ng/mL. Past medical history was collected (including red blood cell (RBC) transfusion, ICT and hematologic data). Prospective MRI (FerriScan) was used to determine R2 liver iron concentration (LIC) and myocardial T2* (mT2*). Treatment decisions were assessed and recorded using an investigator questionnaire after evaluation of patient MRI results.
Results
Of the 243 enrolled patients, 10 and 48% had cardiac and hepatic siderosis, respectively. In all disease groups, mean LIC was above the target range (3–7 mg Fe/g dw), while mean mT2* was normal (≥20 ms). 65.8% of patients received ICT for ≥1 month before or during the study. During the 12-month period prior to the study, 55.9% received deferasirox, 11.9% received deferoxamine and 2.5% received deferiprone. All patients with TM had received ICT; among patients with MDS, NTDT or other anemia types, some patients were chelation naïve (CN)/minimally chelated (MC, chelation <1 month in lifetime; Table). MRI assessment led to a change in management in 105 (45.9) of all evaluable patients (n=229) and in ~60% of CN/MC patients with MDS (17/27 [63.0%]) and other anemias (22/37 [59.5%]; Table). Across all diseases, the predominant changes were increasing chelator dose (43/75 [57.3%]) and starting chelation (27/75 [36.0%]; Table). In patients who had received ICT for >1 month, the most frequent change was increasing chelator dose (TM, 20/23 [87.0%]; MDS, 11/16 [68.8%]; NTDT, 4/7 [57.1%]; other anemias, 5/6 [83.3%]). In CN/MC patients, starting ICT was the predominant change (MDS, 10/13 [76.9%]; NTDT, 2/2 [100.0%]; other anemias, 8/8 [100.0%]). Cardiac MRI assessment (mT2*) was the key driver for ICT decisions in patients with TM (63.8%; ranked as the most important factor in the treatment decision); however, LIC was the key determinant in patients with MDS (42.0), NTDT (44.4%) and other anemias (56.3%).
Conclusion
These data provide real-life insight into the impact of MRI on treatment decisions in a large population of patients with heterogeneous causes of chronic anemia receiving RBC transfusions. A change in ICT management due to MRI analysis occurred in nearly half of all patients. This emphasizes the importance of accurate monitoring of iron load in patients with transfusion-dependent anemias or NTDT to allow for informed clinical decision making.
Session topic: E-poster
Keyword(s): Clinical data, Iron chelation, Iron overload, Magnetic resonance imaging
{{ help_message }}
{{filter}}


