NEURO-PSYCHIATRIC INVOLVEMENT IN PAROXYSMAL NOCTURNAL HEMOGLOBINURIA (PNH)
(Abstract release date: 05/19/16)
EHA Library. Barcellini W. 06/09/16; 133035; E1486

Dr. Wilma Barcellini
Contributions
Contributions
Abstract
Abstract: E1486
Type: Eposter Presentation
Background
PNH is a rare disorder due to a deficiency in GPI–anchored proteins, characterized by haemolytic anaemia, marrow failure and thrombosis. Thrombotic events in PNH generally occur in unusual sites, such as hepatic, portal, mesenteric, splenic, and renal veins. Case reports of cerebral venous sinus thrombosis and arterial ischemic strokes are described in PNH. However, no systematic studies have been reported in asymptomatic patients
Aims
to investigate neuro-psychiatric involvement and neuroradiological findings in PNH patients
Methods
17 PNH patients underwent non-enhanced cerebral magnetic resonance imaging (MRI), and intracranial arterial and venous angio-MRI. The following variables were evaluated: chronic ischemic small vessel disease, quantified according to ARWMC scale (Wahlund LO, Stroke 2001); focal alterations consistent with silent ischemic strokes; active or previous bleeding or micro-haemorrhages; atrophy. Moreover, abnormalities of the circle of Willis and its branches, and of cerebral venous sinus were evaluated. Psychiatric evaluation included the Brief Psychiatric Rating Scale, the Structured Clinical Interview 1 for DSM IV Axis Disorders (SCID-1), the Short Form (36) Health Survey, and the Trail making test
Results
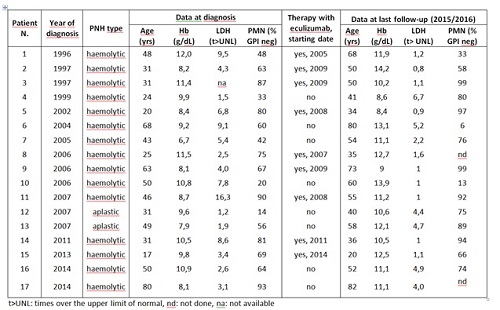
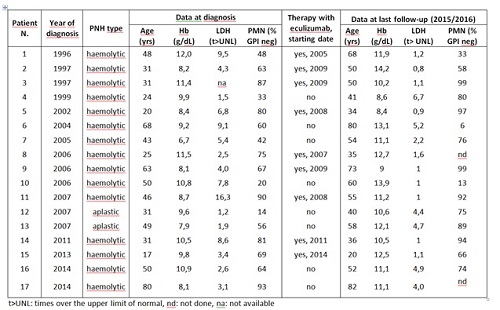
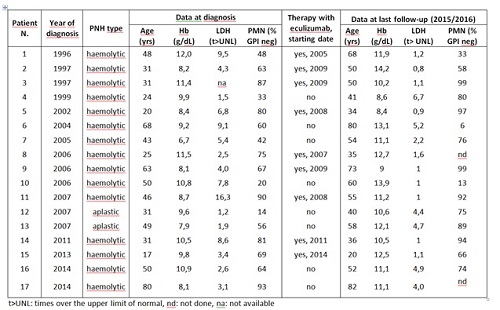
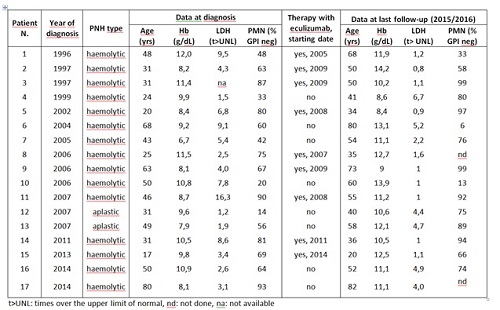
Clinical and haematological parameters of patients are shown in table; 15/17 patients were classic haemolytic (60% transfusion dependent), and 2 PNH in the context of aplastic anemia (both transfusion-dependent until treatment with ATG-Cya). Abdominal pain was present in 41% (N. 1, 2, 4, 10, 11, 14, 15), and abdominal thrombosis in 18% (N. 2, 7, 10). Eculizumab was administered in 53% of cases for transfusion dependence, abdominal pain and/or thrombosis. On MRI, 10 subjects showed white matter (WM) abnormalities related to chronic ischemic small vessel disease. In particular, 5 subjects displayed periventricular WM vascular degeneration, and 6 deep WM focal chronic ischemic lesions. In one subject (N.10) a focal abnormality >5 mm was detected. The evaluation of WM and basal ganglia lesions (ARWMC scale) gave a score of 2 in 2 subjects (N.7, 17), a score of 4 in 3 subjects (N. 2, 10, 11), and a score of 5 in 1 subject (N. 9). No subject displayed active or previous bleeding. Two patients (80 and 81 yrs) showed atrophy of the cerebral hemispheres. Regarding vascular abnormalities, one subject (N.1) had hypoplastic left transverse sinus with irregularities in the sinus wall, suspected for prior partial venous thrombosis. Intracranial artery stenosis or aneurysm, and Moya–Moya like alterations were not observed. Finally, cerebral MRI was unremarkable in 7/17 subjects. Neurological clinical examination was normal in all patients. Psychiatric evaluation did not reveal any psychotic behaviour (except a doubt case in which emerged ideas of delusional thoughts), and test scores for visual attention and task switching resulted appropriate to age. SCID-1 highlighted the presence of a case of generalized anxiety disorder and the suspect of a case of bipolar disorder type 2. The SF36 results evidenced a better health perception than the norm, and even a perception of increased quality of life.
Conclusion
Although largely related to age, unexpected chronic ischemic white matter involvement was present in PNH, and particularly important in two subjects with severe haemolytic disease (N. 9 and 10), of whom one not in eculizumab. White matter lesion burden in asymptomatic patients may help the decision to start therapy, which is not always easy on the clinical/haematological basis.
Session topic: E-poster
Keyword(s): Cerebrovascular disease, MRI, Paroxysmal nocturnal hemoglobinuria (PNH)
Type: Eposter Presentation
Background
PNH is a rare disorder due to a deficiency in GPI–anchored proteins, characterized by haemolytic anaemia, marrow failure and thrombosis. Thrombotic events in PNH generally occur in unusual sites, such as hepatic, portal, mesenteric, splenic, and renal veins. Case reports of cerebral venous sinus thrombosis and arterial ischemic strokes are described in PNH. However, no systematic studies have been reported in asymptomatic patients
Aims
to investigate neuro-psychiatric involvement and neuroradiological findings in PNH patients
Methods
17 PNH patients underwent non-enhanced cerebral magnetic resonance imaging (MRI), and intracranial arterial and venous angio-MRI. The following variables were evaluated: chronic ischemic small vessel disease, quantified according to ARWMC scale (Wahlund LO, Stroke 2001); focal alterations consistent with silent ischemic strokes; active or previous bleeding or micro-haemorrhages; atrophy. Moreover, abnormalities of the circle of Willis and its branches, and of cerebral venous sinus were evaluated. Psychiatric evaluation included the Brief Psychiatric Rating Scale, the Structured Clinical Interview 1 for DSM IV Axis Disorders (SCID-1), the Short Form (36) Health Survey, and the Trail making test
Results
Clinical and haematological parameters of patients are shown in table; 15/17 patients were classic haemolytic (60% transfusion dependent), and 2 PNH in the context of aplastic anemia (both transfusion-dependent until treatment with ATG-Cya). Abdominal pain was present in 41% (N. 1, 2, 4, 10, 11, 14, 15), and abdominal thrombosis in 18% (N. 2, 7, 10). Eculizumab was administered in 53% of cases for transfusion dependence, abdominal pain and/or thrombosis. On MRI, 10 subjects showed white matter (WM) abnormalities related to chronic ischemic small vessel disease. In particular, 5 subjects displayed periventricular WM vascular degeneration, and 6 deep WM focal chronic ischemic lesions. In one subject (N.10) a focal abnormality >5 mm was detected. The evaluation of WM and basal ganglia lesions (ARWMC scale) gave a score of 2 in 2 subjects (N.7, 17), a score of 4 in 3 subjects (N. 2, 10, 11), and a score of 5 in 1 subject (N. 9). No subject displayed active or previous bleeding. Two patients (80 and 81 yrs) showed atrophy of the cerebral hemispheres. Regarding vascular abnormalities, one subject (N.1) had hypoplastic left transverse sinus with irregularities in the sinus wall, suspected for prior partial venous thrombosis. Intracranial artery stenosis or aneurysm, and Moya–Moya like alterations were not observed. Finally, cerebral MRI was unremarkable in 7/17 subjects. Neurological clinical examination was normal in all patients. Psychiatric evaluation did not reveal any psychotic behaviour (except a doubt case in which emerged ideas of delusional thoughts), and test scores for visual attention and task switching resulted appropriate to age. SCID-1 highlighted the presence of a case of generalized anxiety disorder and the suspect of a case of bipolar disorder type 2. The SF36 results evidenced a better health perception than the norm, and even a perception of increased quality of life.
Conclusion
Although largely related to age, unexpected chronic ischemic white matter involvement was present in PNH, and particularly important in two subjects with severe haemolytic disease (N. 9 and 10), of whom one not in eculizumab. White matter lesion burden in asymptomatic patients may help the decision to start therapy, which is not always easy on the clinical/haematological basis.
Session topic: E-poster
Keyword(s): Cerebrovascular disease, MRI, Paroxysmal nocturnal hemoglobinuria (PNH)
Abstract: E1486
Type: Eposter Presentation
Background
PNH is a rare disorder due to a deficiency in GPI–anchored proteins, characterized by haemolytic anaemia, marrow failure and thrombosis. Thrombotic events in PNH generally occur in unusual sites, such as hepatic, portal, mesenteric, splenic, and renal veins. Case reports of cerebral venous sinus thrombosis and arterial ischemic strokes are described in PNH. However, no systematic studies have been reported in asymptomatic patients
Aims
to investigate neuro-psychiatric involvement and neuroradiological findings in PNH patients
Methods
17 PNH patients underwent non-enhanced cerebral magnetic resonance imaging (MRI), and intracranial arterial and venous angio-MRI. The following variables were evaluated: chronic ischemic small vessel disease, quantified according to ARWMC scale (Wahlund LO, Stroke 2001); focal alterations consistent with silent ischemic strokes; active or previous bleeding or micro-haemorrhages; atrophy. Moreover, abnormalities of the circle of Willis and its branches, and of cerebral venous sinus were evaluated. Psychiatric evaluation included the Brief Psychiatric Rating Scale, the Structured Clinical Interview 1 for DSM IV Axis Disorders (SCID-1), the Short Form (36) Health Survey, and the Trail making test
Results
Clinical and haematological parameters of patients are shown in table; 15/17 patients were classic haemolytic (60% transfusion dependent), and 2 PNH in the context of aplastic anemia (both transfusion-dependent until treatment with ATG-Cya). Abdominal pain was present in 41% (N. 1, 2, 4, 10, 11, 14, 15), and abdominal thrombosis in 18% (N. 2, 7, 10). Eculizumab was administered in 53% of cases for transfusion dependence, abdominal pain and/or thrombosis. On MRI, 10 subjects showed white matter (WM) abnormalities related to chronic ischemic small vessel disease. In particular, 5 subjects displayed periventricular WM vascular degeneration, and 6 deep WM focal chronic ischemic lesions. In one subject (N.10) a focal abnormality >5 mm was detected. The evaluation of WM and basal ganglia lesions (ARWMC scale) gave a score of 2 in 2 subjects (N.7, 17), a score of 4 in 3 subjects (N. 2, 10, 11), and a score of 5 in 1 subject (N. 9). No subject displayed active or previous bleeding. Two patients (80 and 81 yrs) showed atrophy of the cerebral hemispheres. Regarding vascular abnormalities, one subject (N.1) had hypoplastic left transverse sinus with irregularities in the sinus wall, suspected for prior partial venous thrombosis. Intracranial artery stenosis or aneurysm, and Moya–Moya like alterations were not observed. Finally, cerebral MRI was unremarkable in 7/17 subjects. Neurological clinical examination was normal in all patients. Psychiatric evaluation did not reveal any psychotic behaviour (except a doubt case in which emerged ideas of delusional thoughts), and test scores for visual attention and task switching resulted appropriate to age. SCID-1 highlighted the presence of a case of generalized anxiety disorder and the suspect of a case of bipolar disorder type 2. The SF36 results evidenced a better health perception than the norm, and even a perception of increased quality of life.
Conclusion
Although largely related to age, unexpected chronic ischemic white matter involvement was present in PNH, and particularly important in two subjects with severe haemolytic disease (N. 9 and 10), of whom one not in eculizumab. White matter lesion burden in asymptomatic patients may help the decision to start therapy, which is not always easy on the clinical/haematological basis.
Session topic: E-poster
Keyword(s): Cerebrovascular disease, MRI, Paroxysmal nocturnal hemoglobinuria (PNH)
Type: Eposter Presentation
Background
PNH is a rare disorder due to a deficiency in GPI–anchored proteins, characterized by haemolytic anaemia, marrow failure and thrombosis. Thrombotic events in PNH generally occur in unusual sites, such as hepatic, portal, mesenteric, splenic, and renal veins. Case reports of cerebral venous sinus thrombosis and arterial ischemic strokes are described in PNH. However, no systematic studies have been reported in asymptomatic patients
Aims
to investigate neuro-psychiatric involvement and neuroradiological findings in PNH patients
Methods
17 PNH patients underwent non-enhanced cerebral magnetic resonance imaging (MRI), and intracranial arterial and venous angio-MRI. The following variables were evaluated: chronic ischemic small vessel disease, quantified according to ARWMC scale (Wahlund LO, Stroke 2001); focal alterations consistent with silent ischemic strokes; active or previous bleeding or micro-haemorrhages; atrophy. Moreover, abnormalities of the circle of Willis and its branches, and of cerebral venous sinus were evaluated. Psychiatric evaluation included the Brief Psychiatric Rating Scale, the Structured Clinical Interview 1 for DSM IV Axis Disorders (SCID-1), the Short Form (36) Health Survey, and the Trail making test
Results
Clinical and haematological parameters of patients are shown in table; 15/17 patients were classic haemolytic (60% transfusion dependent), and 2 PNH in the context of aplastic anemia (both transfusion-dependent until treatment with ATG-Cya). Abdominal pain was present in 41% (N. 1, 2, 4, 10, 11, 14, 15), and abdominal thrombosis in 18% (N. 2, 7, 10). Eculizumab was administered in 53% of cases for transfusion dependence, abdominal pain and/or thrombosis. On MRI, 10 subjects showed white matter (WM) abnormalities related to chronic ischemic small vessel disease. In particular, 5 subjects displayed periventricular WM vascular degeneration, and 6 deep WM focal chronic ischemic lesions. In one subject (N.10) a focal abnormality >5 mm was detected. The evaluation of WM and basal ganglia lesions (ARWMC scale) gave a score of 2 in 2 subjects (N.7, 17), a score of 4 in 3 subjects (N. 2, 10, 11), and a score of 5 in 1 subject (N. 9). No subject displayed active or previous bleeding. Two patients (80 and 81 yrs) showed atrophy of the cerebral hemispheres. Regarding vascular abnormalities, one subject (N.1) had hypoplastic left transverse sinus with irregularities in the sinus wall, suspected for prior partial venous thrombosis. Intracranial artery stenosis or aneurysm, and Moya–Moya like alterations were not observed. Finally, cerebral MRI was unremarkable in 7/17 subjects. Neurological clinical examination was normal in all patients. Psychiatric evaluation did not reveal any psychotic behaviour (except a doubt case in which emerged ideas of delusional thoughts), and test scores for visual attention and task switching resulted appropriate to age. SCID-1 highlighted the presence of a case of generalized anxiety disorder and the suspect of a case of bipolar disorder type 2. The SF36 results evidenced a better health perception than the norm, and even a perception of increased quality of life.
Conclusion
Although largely related to age, unexpected chronic ischemic white matter involvement was present in PNH, and particularly important in two subjects with severe haemolytic disease (N. 9 and 10), of whom one not in eculizumab. White matter lesion burden in asymptomatic patients may help the decision to start therapy, which is not always easy on the clinical/haematological basis.
Session topic: E-poster
Keyword(s): Cerebrovascular disease, MRI, Paroxysmal nocturnal hemoglobinuria (PNH)
{{ help_message }}
{{filter}}


