MONOCENTRIC ASSESSMENT OF THE PROFESSIONAL PRACTICES IN THE MANAGEMENT OF PAIN DURING BONE MARROW ASPIRATION
(Abstract release date: 05/19/16)
EHA Library. poenou g. 06/09/16; 132991; E1442

Ms. geraldine poenou
Contributions
Contributions
Abstract
Abstract: E1442
Type: Eposter Presentation
Background
Bone marrow aspiration performed for the diagnosis of hematologic malignancies is known for being painful. However, pain management is a current concern in the follow-up of patients with chronic diseases.
Aims
Within this overall dynamic of improvement of the analgesic gesture support, an evaluation of the professional practices was initiated by the Hematology Department of the European Georges Pompidou Hospital (Paris, France). The aim of this study was to evaluate the factors involved in the feeling of pain during bone marrow aspiration.
Methods
This monocentric cohort study included 480 patients from 2010 to 2015. They underwent bone marrow aspiration and filled out a standardized questionnaire-based survey including: demographic characteristics (patient’s sex and age, medical department), clinical data (bone hardness, puncture site, diagnosis assumptions and final diagnosis), analgesia methods (lidocaine patch, infiltration with lidocaine, inhalation sedation and premedication) and processing (patient anxiety; intensity of pain evaluated after bone marrow aspiration quoted by the patient and the operator, using a visual analog scale (VAS) from 0 to 10; awareness of the gesture by the patient).
Results
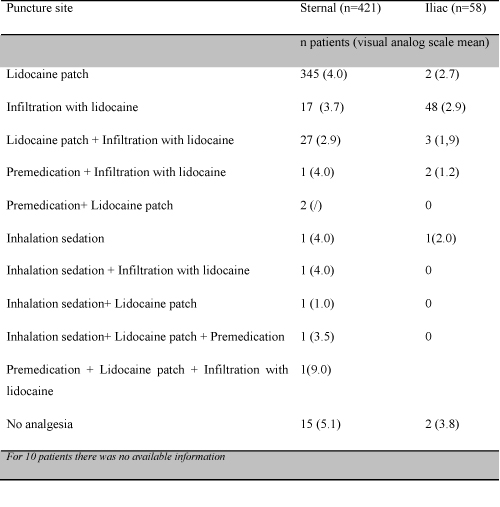
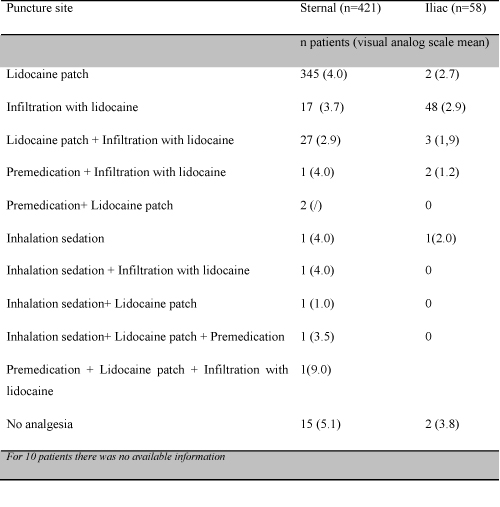
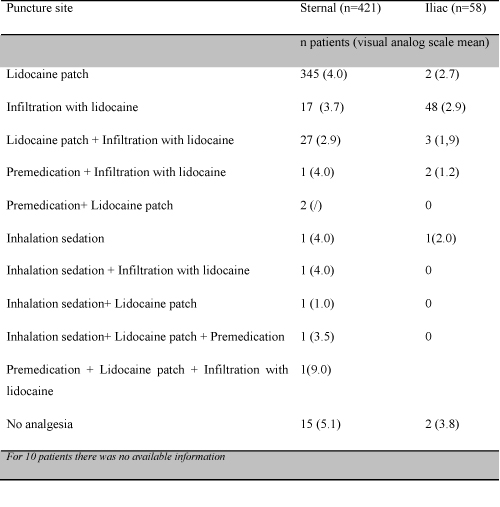
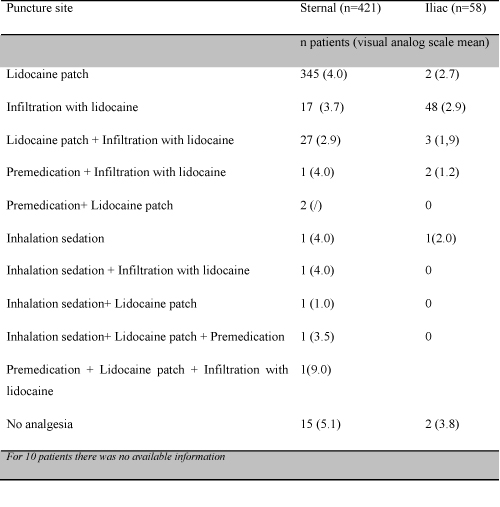
Among the 480 patients, 58% were men. Patients’ average age was 68.7 years. Most patients were from Nephrology (16%), Hematology (16%) and Internal medicine (30%) departments. The main indication of bone marrow aspiration was the diagnosis assessment of monoclonal gammapathies (30%). The most used puncture site was sternal site (88%) and in most cases the bone hardness was described as medium (64%). Bone marrow examination allowed us excluding a central origin for the hematologic anomaly in 43% patients. The foremost analgesia method was the use of lidocaine patch (80%) with an average exposure of 68 minutes. Half of patients declared not to be anxious before bone marrow aspiration. Pain was generally rated between 3 and 4 on a scale of 10 (43%), and lower than they had expected (58%). Overall, 97 % of bone marrow aspirations were performed under analgesia.(Table 1.Pain's management). Analgesic treatment was found significantly effective compared with no analgesia? (p<0.001). Patients experienced less pain when they considered that they were well-informed (p<0.001).Women were significantly more sensitive than men (p<0.05). In our study, sternal site was more painful than superior iliac bone site (p<0.001). There were no relationships between pain intensity and patients' age, medical department, bone hardness, diagnosis assumptions, final diagnosis, a particular analgesia method and patient anxiety (p>0.05).
Conclusion
The perception of and reaction to pain are influenced by the psychological state of the patient. This is an undisputed fact that medical staff should provide information on the steps taken in daily practice and our study on bone marrow aspiration is consistent with this behavior. The prevention and management of pain require an integrated approach between its sensori-discriminative component and its psychological dimension. In our study, we show the benefit of analgesia together with intelligible information in the management of pain during bone aspiration.
Session topic: E-poster
Keyword(s): Bone Marrow, Pain, Practice, Quality of life
Type: Eposter Presentation
Background
Bone marrow aspiration performed for the diagnosis of hematologic malignancies is known for being painful. However, pain management is a current concern in the follow-up of patients with chronic diseases.
Aims
Within this overall dynamic of improvement of the analgesic gesture support, an evaluation of the professional practices was initiated by the Hematology Department of the European Georges Pompidou Hospital (Paris, France). The aim of this study was to evaluate the factors involved in the feeling of pain during bone marrow aspiration.
Methods
This monocentric cohort study included 480 patients from 2010 to 2015. They underwent bone marrow aspiration and filled out a standardized questionnaire-based survey including: demographic characteristics (patient’s sex and age, medical department), clinical data (bone hardness, puncture site, diagnosis assumptions and final diagnosis), analgesia methods (lidocaine patch, infiltration with lidocaine, inhalation sedation and premedication) and processing (patient anxiety; intensity of pain evaluated after bone marrow aspiration quoted by the patient and the operator, using a visual analog scale (VAS) from 0 to 10; awareness of the gesture by the patient).
Results
Among the 480 patients, 58% were men. Patients’ average age was 68.7 years. Most patients were from Nephrology (16%), Hematology (16%) and Internal medicine (30%) departments. The main indication of bone marrow aspiration was the diagnosis assessment of monoclonal gammapathies (30%). The most used puncture site was sternal site (88%) and in most cases the bone hardness was described as medium (64%). Bone marrow examination allowed us excluding a central origin for the hematologic anomaly in 43% patients. The foremost analgesia method was the use of lidocaine patch (80%) with an average exposure of 68 minutes. Half of patients declared not to be anxious before bone marrow aspiration. Pain was generally rated between 3 and 4 on a scale of 10 (43%), and lower than they had expected (58%). Overall, 97 % of bone marrow aspirations were performed under analgesia.(Table 1.Pain's management). Analgesic treatment was found significantly effective compared with no analgesia? (p<0.001). Patients experienced less pain when they considered that they were well-informed (p<0.001).Women were significantly more sensitive than men (p<0.05). In our study, sternal site was more painful than superior iliac bone site (p<0.001). There were no relationships between pain intensity and patients' age, medical department, bone hardness, diagnosis assumptions, final diagnosis, a particular analgesia method and patient anxiety (p>0.05).
Conclusion
The perception of and reaction to pain are influenced by the psychological state of the patient. This is an undisputed fact that medical staff should provide information on the steps taken in daily practice and our study on bone marrow aspiration is consistent with this behavior. The prevention and management of pain require an integrated approach between its sensori-discriminative component and its psychological dimension. In our study, we show the benefit of analgesia together with intelligible information in the management of pain during bone aspiration.
Session topic: E-poster
Keyword(s): Bone Marrow, Pain, Practice, Quality of life
Abstract: E1442
Type: Eposter Presentation
Background
Bone marrow aspiration performed for the diagnosis of hematologic malignancies is known for being painful. However, pain management is a current concern in the follow-up of patients with chronic diseases.
Aims
Within this overall dynamic of improvement of the analgesic gesture support, an evaluation of the professional practices was initiated by the Hematology Department of the European Georges Pompidou Hospital (Paris, France). The aim of this study was to evaluate the factors involved in the feeling of pain during bone marrow aspiration.
Methods
This monocentric cohort study included 480 patients from 2010 to 2015. They underwent bone marrow aspiration and filled out a standardized questionnaire-based survey including: demographic characteristics (patient’s sex and age, medical department), clinical data (bone hardness, puncture site, diagnosis assumptions and final diagnosis), analgesia methods (lidocaine patch, infiltration with lidocaine, inhalation sedation and premedication) and processing (patient anxiety; intensity of pain evaluated after bone marrow aspiration quoted by the patient and the operator, using a visual analog scale (VAS) from 0 to 10; awareness of the gesture by the patient).
Results
Among the 480 patients, 58% were men. Patients’ average age was 68.7 years. Most patients were from Nephrology (16%), Hematology (16%) and Internal medicine (30%) departments. The main indication of bone marrow aspiration was the diagnosis assessment of monoclonal gammapathies (30%). The most used puncture site was sternal site (88%) and in most cases the bone hardness was described as medium (64%). Bone marrow examination allowed us excluding a central origin for the hematologic anomaly in 43% patients. The foremost analgesia method was the use of lidocaine patch (80%) with an average exposure of 68 minutes. Half of patients declared not to be anxious before bone marrow aspiration. Pain was generally rated between 3 and 4 on a scale of 10 (43%), and lower than they had expected (58%). Overall, 97 % of bone marrow aspirations were performed under analgesia.(Table 1.Pain's management). Analgesic treatment was found significantly effective compared with no analgesia? (p<0.001). Patients experienced less pain when they considered that they were well-informed (p<0.001).Women were significantly more sensitive than men (p<0.05). In our study, sternal site was more painful than superior iliac bone site (p<0.001). There were no relationships between pain intensity and patients' age, medical department, bone hardness, diagnosis assumptions, final diagnosis, a particular analgesia method and patient anxiety (p>0.05).
Conclusion
The perception of and reaction to pain are influenced by the psychological state of the patient. This is an undisputed fact that medical staff should provide information on the steps taken in daily practice and our study on bone marrow aspiration is consistent with this behavior. The prevention and management of pain require an integrated approach between its sensori-discriminative component and its psychological dimension. In our study, we show the benefit of analgesia together with intelligible information in the management of pain during bone aspiration.
Session topic: E-poster
Keyword(s): Bone Marrow, Pain, Practice, Quality of life
Type: Eposter Presentation
Background
Bone marrow aspiration performed for the diagnosis of hematologic malignancies is known for being painful. However, pain management is a current concern in the follow-up of patients with chronic diseases.
Aims
Within this overall dynamic of improvement of the analgesic gesture support, an evaluation of the professional practices was initiated by the Hematology Department of the European Georges Pompidou Hospital (Paris, France). The aim of this study was to evaluate the factors involved in the feeling of pain during bone marrow aspiration.
Methods
This monocentric cohort study included 480 patients from 2010 to 2015. They underwent bone marrow aspiration and filled out a standardized questionnaire-based survey including: demographic characteristics (patient’s sex and age, medical department), clinical data (bone hardness, puncture site, diagnosis assumptions and final diagnosis), analgesia methods (lidocaine patch, infiltration with lidocaine, inhalation sedation and premedication) and processing (patient anxiety; intensity of pain evaluated after bone marrow aspiration quoted by the patient and the operator, using a visual analog scale (VAS) from 0 to 10; awareness of the gesture by the patient).
Results
Among the 480 patients, 58% were men. Patients’ average age was 68.7 years. Most patients were from Nephrology (16%), Hematology (16%) and Internal medicine (30%) departments. The main indication of bone marrow aspiration was the diagnosis assessment of monoclonal gammapathies (30%). The most used puncture site was sternal site (88%) and in most cases the bone hardness was described as medium (64%). Bone marrow examination allowed us excluding a central origin for the hematologic anomaly in 43% patients. The foremost analgesia method was the use of lidocaine patch (80%) with an average exposure of 68 minutes. Half of patients declared not to be anxious before bone marrow aspiration. Pain was generally rated between 3 and 4 on a scale of 10 (43%), and lower than they had expected (58%). Overall, 97 % of bone marrow aspirations were performed under analgesia.(Table 1.Pain's management). Analgesic treatment was found significantly effective compared with no analgesia? (p<0.001). Patients experienced less pain when they considered that they were well-informed (p<0.001).Women were significantly more sensitive than men (p<0.05). In our study, sternal site was more painful than superior iliac bone site (p<0.001). There were no relationships between pain intensity and patients' age, medical department, bone hardness, diagnosis assumptions, final diagnosis, a particular analgesia method and patient anxiety (p>0.05).
Conclusion
The perception of and reaction to pain are influenced by the psychological state of the patient. This is an undisputed fact that medical staff should provide information on the steps taken in daily practice and our study on bone marrow aspiration is consistent with this behavior. The prevention and management of pain require an integrated approach between its sensori-discriminative component and its psychological dimension. In our study, we show the benefit of analgesia together with intelligible information in the management of pain during bone aspiration.
Session topic: E-poster
Keyword(s): Bone Marrow, Pain, Practice, Quality of life
{{ help_message }}
{{filter}}


