HEMOPHAGOCYTIC LYMPHOHISTIOCYTOSIS: RETROSPECTIVE ANALYSIS FOR PROGNOSTIC FACTORS
(Abstract release date: 05/19/16)
EHA Library. Dholaria B. 06/09/16; 132954; E1405

Dr. Bhagriathbhai Dholaria
Contributions
Contributions
Abstract
Abstract: E1405
Type: Eposter Presentation
Background
Hemophagocytic lymphohistiocytosis (HLH) is a life- threatening systemic inflammatory condition. Due to rarity of the cases, it presents difficulties in diagnosis and management. Survival remains poor despite aggressive chemotherapy. Patients with fever of unknown origin, lymphadenopathy, deteriorating performance status, encephalopathy and elevated systemic inflammatory parameters frequently show no clear cut diagnostic criteria specific for HLH. Among adults, late onset of inherited HLH is possible, but acquired HLH triggered by infection, malignancy or autoimmune disease is more frequent than in pediatrics.
Aims
Patient outcomes varied markedly despite standardize therapy. Reliable prognostic disease markers may help to tailor intensity of therapy and predict long term outcomes. We attempt to look for variables associated with difference in mortality within 30 days of diagnosis.
Methods
We performed a retrospective search on mayo clinic patient database for the patients with the diagnosis of HLH from 2005 to 2015.HLH-04 criteria were used to select the study population.1 Patients were divided in two groups based on survival after the diagnosis. We analyzed different clinical and laboratory parameters to detect significant difference between patients expired within 30 days of diagnosis or survived longer than 30 days.Chi-square analysis was performed between two groups of patients: 1- Time to death from diagnosis < 30 days.2- Time to death from diagnosis > 30 days.We assessed difference in various clinical and laboratory parameters.
Results
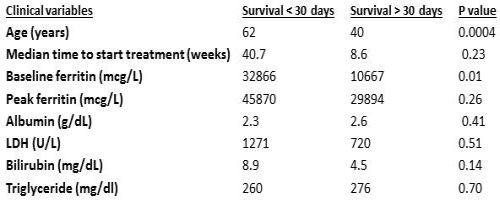
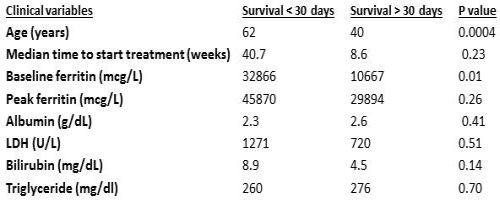
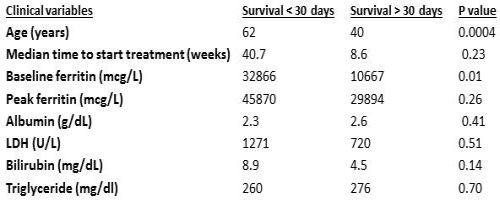
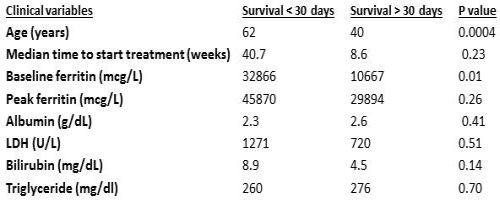
Demographics: 40 patients were included in the analysis who met HLH- 04 criteria. Mean age was 49 years, 40% (16/40) were female and 60% (24/40) were male. Underlying HLH etiology was malignancy 37% (15/40), infection 20% (8/40), rheumatological 17% (7/40), idiopathic 20% (8/40). Two patients were peripartum and one with Kikuchi syndrome. Fever was present in 90% (36/40) and splenomegaly was found in 75% (30/40) of the patients.Labs: Average ferritin at diagnosis 19546 mcg/L, ferritin peak 36284 mcg/L, ALP 226U/L, AST 274U/L, T. bilirubin 6.3mg/dL, LDH 937 U/L, triglyceride 269 mg/dL, albumin 2.4g/dL and EBV DNA PCR were positive in 32% (13/40) of the patients.Treatment: Median time from onset of symptoms to start the treatment was 8.1 weeks. Steroids were used in 92% (37/40), etoposide was used in 55% (22/40), and HLH 04 protocol (Etoposide/dexamethasone/cyclosporine) was used in 40% (16/40) of the patients. IVIG was used in 13% with underlying rheumatological process. Mean follow up was 57 weeks (0.1 to 336 weeks) for the whole group. Total 40% (16/40) died within 30 days of diagnosis.Outcomes: Risk of 30- days mortality was significantly higher in the patients with ferritin >5000 mcg/L at the time of diagnosis and age > 55 years.Out of total 40 patients, 54% (12/22) died in ferritin >5000mcg/L group and 22% (4/18) died in ferritin < 5000 mcg/L group within 30 days. (p- 0.03)Death rate within 30 days was 65% (11/17) with age > 55 years and 22% (5/23) with age < 55 years at the time of diagnosis of HLH. (p-0.05)We did not find any significant difference in the following factors:30 day mortality was 31% (4/13) in EBV positive group and 44% (12/27) in EBV negative group (P-0.40); 50% (8/16) in malignant group and 33% (8/24) in non- malignant. (P-0.29)No difference between the groups in terms of gender, etoposide use, and time to start treatment was found in 30 days mortality. Table 1 summarizes the findings.
Conclusion
Elevated ferritin at the time of diagnosis and older age are associated with significant risk of 30 day mortality from HLH. In combination with other prognostic factors age and ferritin can be used to risk stratification at the time of diagnosis. These factors can be incorporated in future clinical trials to choose different treatment pathways.
Session topic: E-poster
Keyword(s): EBV, Ferritin, Macrophage, Phagocytes
Type: Eposter Presentation
Background
Hemophagocytic lymphohistiocytosis (HLH) is a life- threatening systemic inflammatory condition. Due to rarity of the cases, it presents difficulties in diagnosis and management. Survival remains poor despite aggressive chemotherapy. Patients with fever of unknown origin, lymphadenopathy, deteriorating performance status, encephalopathy and elevated systemic inflammatory parameters frequently show no clear cut diagnostic criteria specific for HLH. Among adults, late onset of inherited HLH is possible, but acquired HLH triggered by infection, malignancy or autoimmune disease is more frequent than in pediatrics.
Aims
Patient outcomes varied markedly despite standardize therapy. Reliable prognostic disease markers may help to tailor intensity of therapy and predict long term outcomes. We attempt to look for variables associated with difference in mortality within 30 days of diagnosis.
Methods
We performed a retrospective search on mayo clinic patient database for the patients with the diagnosis of HLH from 2005 to 2015.HLH-04 criteria were used to select the study population.1 Patients were divided in two groups based on survival after the diagnosis. We analyzed different clinical and laboratory parameters to detect significant difference between patients expired within 30 days of diagnosis or survived longer than 30 days.Chi-square analysis was performed between two groups of patients: 1- Time to death from diagnosis < 30 days.2- Time to death from diagnosis > 30 days.We assessed difference in various clinical and laboratory parameters.
Results
Demographics: 40 patients were included in the analysis who met HLH- 04 criteria. Mean age was 49 years, 40% (16/40) were female and 60% (24/40) were male. Underlying HLH etiology was malignancy 37% (15/40), infection 20% (8/40), rheumatological 17% (7/40), idiopathic 20% (8/40). Two patients were peripartum and one with Kikuchi syndrome. Fever was present in 90% (36/40) and splenomegaly was found in 75% (30/40) of the patients.Labs: Average ferritin at diagnosis 19546 mcg/L, ferritin peak 36284 mcg/L, ALP 226U/L, AST 274U/L, T. bilirubin 6.3mg/dL, LDH 937 U/L, triglyceride 269 mg/dL, albumin 2.4g/dL and EBV DNA PCR were positive in 32% (13/40) of the patients.Treatment: Median time from onset of symptoms to start the treatment was 8.1 weeks. Steroids were used in 92% (37/40), etoposide was used in 55% (22/40), and HLH 04 protocol (Etoposide/dexamethasone/cyclosporine) was used in 40% (16/40) of the patients. IVIG was used in 13% with underlying rheumatological process. Mean follow up was 57 weeks (0.1 to 336 weeks) for the whole group. Total 40% (16/40) died within 30 days of diagnosis.Outcomes: Risk of 30- days mortality was significantly higher in the patients with ferritin >5000 mcg/L at the time of diagnosis and age > 55 years.Out of total 40 patients, 54% (12/22) died in ferritin >5000mcg/L group and 22% (4/18) died in ferritin < 5000 mcg/L group within 30 days. (p- 0.03)Death rate within 30 days was 65% (11/17) with age > 55 years and 22% (5/23) with age < 55 years at the time of diagnosis of HLH. (p-0.05)We did not find any significant difference in the following factors:30 day mortality was 31% (4/13) in EBV positive group and 44% (12/27) in EBV negative group (P-0.40); 50% (8/16) in malignant group and 33% (8/24) in non- malignant. (P-0.29)No difference between the groups in terms of gender, etoposide use, and time to start treatment was found in 30 days mortality. Table 1 summarizes the findings.
Conclusion
Elevated ferritin at the time of diagnosis and older age are associated with significant risk of 30 day mortality from HLH. In combination with other prognostic factors age and ferritin can be used to risk stratification at the time of diagnosis. These factors can be incorporated in future clinical trials to choose different treatment pathways.
Session topic: E-poster
Keyword(s): EBV, Ferritin, Macrophage, Phagocytes
Abstract: E1405
Type: Eposter Presentation
Background
Hemophagocytic lymphohistiocytosis (HLH) is a life- threatening systemic inflammatory condition. Due to rarity of the cases, it presents difficulties in diagnosis and management. Survival remains poor despite aggressive chemotherapy. Patients with fever of unknown origin, lymphadenopathy, deteriorating performance status, encephalopathy and elevated systemic inflammatory parameters frequently show no clear cut diagnostic criteria specific for HLH. Among adults, late onset of inherited HLH is possible, but acquired HLH triggered by infection, malignancy or autoimmune disease is more frequent than in pediatrics.
Aims
Patient outcomes varied markedly despite standardize therapy. Reliable prognostic disease markers may help to tailor intensity of therapy and predict long term outcomes. We attempt to look for variables associated with difference in mortality within 30 days of diagnosis.
Methods
We performed a retrospective search on mayo clinic patient database for the patients with the diagnosis of HLH from 2005 to 2015.HLH-04 criteria were used to select the study population.1 Patients were divided in two groups based on survival after the diagnosis. We analyzed different clinical and laboratory parameters to detect significant difference between patients expired within 30 days of diagnosis or survived longer than 30 days.Chi-square analysis was performed between two groups of patients: 1- Time to death from diagnosis < 30 days.2- Time to death from diagnosis > 30 days.We assessed difference in various clinical and laboratory parameters.
Results
Demographics: 40 patients were included in the analysis who met HLH- 04 criteria. Mean age was 49 years, 40% (16/40) were female and 60% (24/40) were male. Underlying HLH etiology was malignancy 37% (15/40), infection 20% (8/40), rheumatological 17% (7/40), idiopathic 20% (8/40). Two patients were peripartum and one with Kikuchi syndrome. Fever was present in 90% (36/40) and splenomegaly was found in 75% (30/40) of the patients.Labs: Average ferritin at diagnosis 19546 mcg/L, ferritin peak 36284 mcg/L, ALP 226U/L, AST 274U/L, T. bilirubin 6.3mg/dL, LDH 937 U/L, triglyceride 269 mg/dL, albumin 2.4g/dL and EBV DNA PCR were positive in 32% (13/40) of the patients.Treatment: Median time from onset of symptoms to start the treatment was 8.1 weeks. Steroids were used in 92% (37/40), etoposide was used in 55% (22/40), and HLH 04 protocol (Etoposide/dexamethasone/cyclosporine) was used in 40% (16/40) of the patients. IVIG was used in 13% with underlying rheumatological process. Mean follow up was 57 weeks (0.1 to 336 weeks) for the whole group. Total 40% (16/40) died within 30 days of diagnosis.Outcomes: Risk of 30- days mortality was significantly higher in the patients with ferritin >5000 mcg/L at the time of diagnosis and age > 55 years.Out of total 40 patients, 54% (12/22) died in ferritin >5000mcg/L group and 22% (4/18) died in ferritin < 5000 mcg/L group within 30 days. (p- 0.03)Death rate within 30 days was 65% (11/17) with age > 55 years and 22% (5/23) with age < 55 years at the time of diagnosis of HLH. (p-0.05)We did not find any significant difference in the following factors:30 day mortality was 31% (4/13) in EBV positive group and 44% (12/27) in EBV negative group (P-0.40); 50% (8/16) in malignant group and 33% (8/24) in non- malignant. (P-0.29)No difference between the groups in terms of gender, etoposide use, and time to start treatment was found in 30 days mortality. Table 1 summarizes the findings.
Conclusion
Elevated ferritin at the time of diagnosis and older age are associated with significant risk of 30 day mortality from HLH. In combination with other prognostic factors age and ferritin can be used to risk stratification at the time of diagnosis. These factors can be incorporated in future clinical trials to choose different treatment pathways.
Session topic: E-poster
Keyword(s): EBV, Ferritin, Macrophage, Phagocytes
Type: Eposter Presentation
Background
Hemophagocytic lymphohistiocytosis (HLH) is a life- threatening systemic inflammatory condition. Due to rarity of the cases, it presents difficulties in diagnosis and management. Survival remains poor despite aggressive chemotherapy. Patients with fever of unknown origin, lymphadenopathy, deteriorating performance status, encephalopathy and elevated systemic inflammatory parameters frequently show no clear cut diagnostic criteria specific for HLH. Among adults, late onset of inherited HLH is possible, but acquired HLH triggered by infection, malignancy or autoimmune disease is more frequent than in pediatrics.
Aims
Patient outcomes varied markedly despite standardize therapy. Reliable prognostic disease markers may help to tailor intensity of therapy and predict long term outcomes. We attempt to look for variables associated with difference in mortality within 30 days of diagnosis.
Methods
We performed a retrospective search on mayo clinic patient database for the patients with the diagnosis of HLH from 2005 to 2015.HLH-04 criteria were used to select the study population.1 Patients were divided in two groups based on survival after the diagnosis. We analyzed different clinical and laboratory parameters to detect significant difference between patients expired within 30 days of diagnosis or survived longer than 30 days.Chi-square analysis was performed between two groups of patients: 1- Time to death from diagnosis < 30 days.2- Time to death from diagnosis > 30 days.We assessed difference in various clinical and laboratory parameters.
Results
Demographics: 40 patients were included in the analysis who met HLH- 04 criteria. Mean age was 49 years, 40% (16/40) were female and 60% (24/40) were male. Underlying HLH etiology was malignancy 37% (15/40), infection 20% (8/40), rheumatological 17% (7/40), idiopathic 20% (8/40). Two patients were peripartum and one with Kikuchi syndrome. Fever was present in 90% (36/40) and splenomegaly was found in 75% (30/40) of the patients.Labs: Average ferritin at diagnosis 19546 mcg/L, ferritin peak 36284 mcg/L, ALP 226U/L, AST 274U/L, T. bilirubin 6.3mg/dL, LDH 937 U/L, triglyceride 269 mg/dL, albumin 2.4g/dL and EBV DNA PCR were positive in 32% (13/40) of the patients.Treatment: Median time from onset of symptoms to start the treatment was 8.1 weeks. Steroids were used in 92% (37/40), etoposide was used in 55% (22/40), and HLH 04 protocol (Etoposide/dexamethasone/cyclosporine) was used in 40% (16/40) of the patients. IVIG was used in 13% with underlying rheumatological process. Mean follow up was 57 weeks (0.1 to 336 weeks) for the whole group. Total 40% (16/40) died within 30 days of diagnosis.Outcomes: Risk of 30- days mortality was significantly higher in the patients with ferritin >5000 mcg/L at the time of diagnosis and age > 55 years.Out of total 40 patients, 54% (12/22) died in ferritin >5000mcg/L group and 22% (4/18) died in ferritin < 5000 mcg/L group within 30 days. (p- 0.03)Death rate within 30 days was 65% (11/17) with age > 55 years and 22% (5/23) with age < 55 years at the time of diagnosis of HLH. (p-0.05)We did not find any significant difference in the following factors:30 day mortality was 31% (4/13) in EBV positive group and 44% (12/27) in EBV negative group (P-0.40); 50% (8/16) in malignant group and 33% (8/24) in non- malignant. (P-0.29)No difference between the groups in terms of gender, etoposide use, and time to start treatment was found in 30 days mortality. Table 1 summarizes the findings.
Conclusion
Elevated ferritin at the time of diagnosis and older age are associated with significant risk of 30 day mortality from HLH. In combination with other prognostic factors age and ferritin can be used to risk stratification at the time of diagnosis. These factors can be incorporated in future clinical trials to choose different treatment pathways.
Session topic: E-poster
Keyword(s): EBV, Ferritin, Macrophage, Phagocytes
{{ help_message }}
{{filter}}


