DURATION OF SECOND LINE TREATMENT AND SURVIVAL IN MULTIPLE MYELOMA
(Abstract release date: 05/19/16)
EHA Library. Parameswaran H. 06/09/16; 132872; E1323

Dr. Hari Parameswaran
Contributions
Contributions
Abstract
Abstract: E1323
Type: Eposter Presentation
Background
Evidence from post-hoc analyses of clinical trials supports the paradigm of extended treatment leading to an overall survival (OS) benefit in relapsed/refractory multiple myeloma (RRMM).
Aims
This observational study evaluated whether longer 2nd line treatment (SLT) duration is associated with improved OS among patients with RRMM.
Methods
In this retrospective cohort study of a US national EMR database, newly diagnosed adults with MM initiating 1st line therapy (FLT) and SLT between 1/2008 and 12/2014 were followed through earliest of either 1 year or death/loss to follow up/end of study period (12/31/2014) after start of SLT. FLT began with the first claim for MM-directed therapy following diagnosis (dx). SLT was identified by: 1) retreatment with follow-up regimen with gap of >3 months after end of FLT, or 2) switch to another drug combination after FLT. A logistic marginal structural model was used to estimate the causal effect of SLT duration on 1-year OS probability, adjusting for time-dependent confounders and baseline covariates. Immortal time bias was addressed by estimating the effect of SLT duration on outcome within each monthly interval from start of SLT.
Results
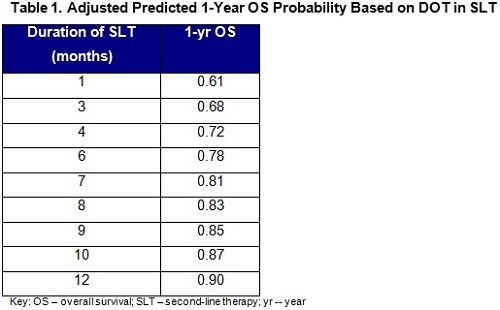
Among 340 patients, mean age was 70 years (standard deviation (SD), 10); 51% were male; 9% had known high risk MM; 46% received immunomodulatory (IMID-), 35% received proteasome inhibitor (PI-), and 6% received PI+IMID-based SLT. Median duration of SLT was 6.87 months (95% CI: 6.17, 8.40). The odds of 1-year OS were 1.17 times higher for each additional month of SLT (OR: 1.17 [95% CI: 1.10, 1.25] P<0.001), controlling for age, gender, cytogenetic risk, comorbidities, race, ethnicity, region, insurance type, treatment-free interval prior to SLT, FLT/SLT regimen type, year of diagnosis (dx), time since initial dx, time-dependent treatment- and MM-related symptoms, and post SLT regimens (Table 1).
Conclusion
Longer duration of SLT was significantly associated with longer OS. Despite substantial heterogeneity in patient/disease characteristics and treatment patterns, the clinical benefit of continued longer term therapy at relapse appears to be generalizable to patients receiving care in the real-world setting.
Session topic: E-poster
Keyword(s): Clinical outcome, Myeloma, Refractory, Relapse
Type: Eposter Presentation
Background
Evidence from post-hoc analyses of clinical trials supports the paradigm of extended treatment leading to an overall survival (OS) benefit in relapsed/refractory multiple myeloma (RRMM).
Aims
This observational study evaluated whether longer 2nd line treatment (SLT) duration is associated with improved OS among patients with RRMM.
Methods
In this retrospective cohort study of a US national EMR database, newly diagnosed adults with MM initiating 1st line therapy (FLT) and SLT between 1/2008 and 12/2014 were followed through earliest of either 1 year or death/loss to follow up/end of study period (12/31/2014) after start of SLT. FLT began with the first claim for MM-directed therapy following diagnosis (dx). SLT was identified by: 1) retreatment with follow-up regimen with gap of >3 months after end of FLT, or 2) switch to another drug combination after FLT. A logistic marginal structural model was used to estimate the causal effect of SLT duration on 1-year OS probability, adjusting for time-dependent confounders and baseline covariates. Immortal time bias was addressed by estimating the effect of SLT duration on outcome within each monthly interval from start of SLT.
Results
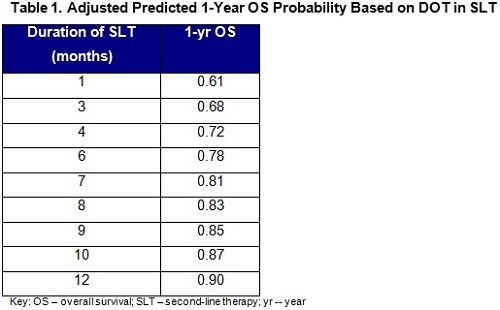
Among 340 patients, mean age was 70 years (standard deviation (SD), 10); 51% were male; 9% had known high risk MM; 46% received immunomodulatory (IMID-), 35% received proteasome inhibitor (PI-), and 6% received PI+IMID-based SLT. Median duration of SLT was 6.87 months (95% CI: 6.17, 8.40). The odds of 1-year OS were 1.17 times higher for each additional month of SLT (OR: 1.17 [95% CI: 1.10, 1.25] P<0.001), controlling for age, gender, cytogenetic risk, comorbidities, race, ethnicity, region, insurance type, treatment-free interval prior to SLT, FLT/SLT regimen type, year of diagnosis (dx), time since initial dx, time-dependent treatment- and MM-related symptoms, and post SLT regimens (Table 1).
Conclusion
Longer duration of SLT was significantly associated with longer OS. Despite substantial heterogeneity in patient/disease characteristics and treatment patterns, the clinical benefit of continued longer term therapy at relapse appears to be generalizable to patients receiving care in the real-world setting.
Session topic: E-poster
Keyword(s): Clinical outcome, Myeloma, Refractory, Relapse
Abstract: E1323
Type: Eposter Presentation
Background
Evidence from post-hoc analyses of clinical trials supports the paradigm of extended treatment leading to an overall survival (OS) benefit in relapsed/refractory multiple myeloma (RRMM).
Aims
This observational study evaluated whether longer 2nd line treatment (SLT) duration is associated with improved OS among patients with RRMM.
Methods
In this retrospective cohort study of a US national EMR database, newly diagnosed adults with MM initiating 1st line therapy (FLT) and SLT between 1/2008 and 12/2014 were followed through earliest of either 1 year or death/loss to follow up/end of study period (12/31/2014) after start of SLT. FLT began with the first claim for MM-directed therapy following diagnosis (dx). SLT was identified by: 1) retreatment with follow-up regimen with gap of >3 months after end of FLT, or 2) switch to another drug combination after FLT. A logistic marginal structural model was used to estimate the causal effect of SLT duration on 1-year OS probability, adjusting for time-dependent confounders and baseline covariates. Immortal time bias was addressed by estimating the effect of SLT duration on outcome within each monthly interval from start of SLT.
Results
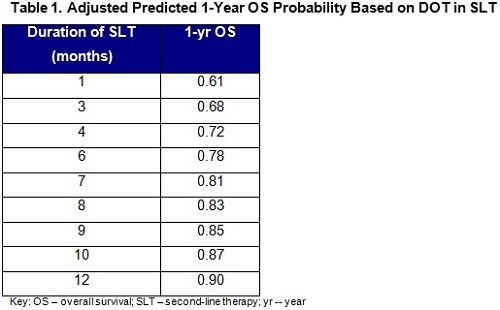
Among 340 patients, mean age was 70 years (standard deviation (SD), 10); 51% were male; 9% had known high risk MM; 46% received immunomodulatory (IMID-), 35% received proteasome inhibitor (PI-), and 6% received PI+IMID-based SLT. Median duration of SLT was 6.87 months (95% CI: 6.17, 8.40). The odds of 1-year OS were 1.17 times higher for each additional month of SLT (OR: 1.17 [95% CI: 1.10, 1.25] P<0.001), controlling for age, gender, cytogenetic risk, comorbidities, race, ethnicity, region, insurance type, treatment-free interval prior to SLT, FLT/SLT regimen type, year of diagnosis (dx), time since initial dx, time-dependent treatment- and MM-related symptoms, and post SLT regimens (Table 1).
Conclusion
Longer duration of SLT was significantly associated with longer OS. Despite substantial heterogeneity in patient/disease characteristics and treatment patterns, the clinical benefit of continued longer term therapy at relapse appears to be generalizable to patients receiving care in the real-world setting.
Session topic: E-poster
Keyword(s): Clinical outcome, Myeloma, Refractory, Relapse
Type: Eposter Presentation
Background
Evidence from post-hoc analyses of clinical trials supports the paradigm of extended treatment leading to an overall survival (OS) benefit in relapsed/refractory multiple myeloma (RRMM).
Aims
This observational study evaluated whether longer 2nd line treatment (SLT) duration is associated with improved OS among patients with RRMM.
Methods
In this retrospective cohort study of a US national EMR database, newly diagnosed adults with MM initiating 1st line therapy (FLT) and SLT between 1/2008 and 12/2014 were followed through earliest of either 1 year or death/loss to follow up/end of study period (12/31/2014) after start of SLT. FLT began with the first claim for MM-directed therapy following diagnosis (dx). SLT was identified by: 1) retreatment with follow-up regimen with gap of >3 months after end of FLT, or 2) switch to another drug combination after FLT. A logistic marginal structural model was used to estimate the causal effect of SLT duration on 1-year OS probability, adjusting for time-dependent confounders and baseline covariates. Immortal time bias was addressed by estimating the effect of SLT duration on outcome within each monthly interval from start of SLT.
Results
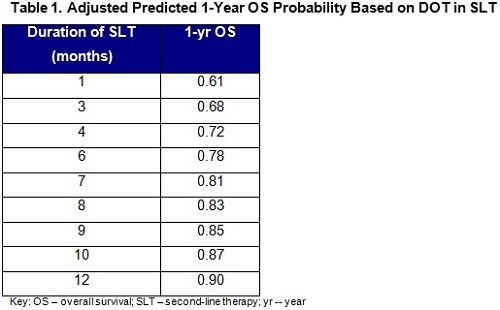
Among 340 patients, mean age was 70 years (standard deviation (SD), 10); 51% were male; 9% had known high risk MM; 46% received immunomodulatory (IMID-), 35% received proteasome inhibitor (PI-), and 6% received PI+IMID-based SLT. Median duration of SLT was 6.87 months (95% CI: 6.17, 8.40). The odds of 1-year OS were 1.17 times higher for each additional month of SLT (OR: 1.17 [95% CI: 1.10, 1.25] P<0.001), controlling for age, gender, cytogenetic risk, comorbidities, race, ethnicity, region, insurance type, treatment-free interval prior to SLT, FLT/SLT regimen type, year of diagnosis (dx), time since initial dx, time-dependent treatment- and MM-related symptoms, and post SLT regimens (Table 1).
Conclusion
Longer duration of SLT was significantly associated with longer OS. Despite substantial heterogeneity in patient/disease characteristics and treatment patterns, the clinical benefit of continued longer term therapy at relapse appears to be generalizable to patients receiving care in the real-world setting.
Session topic: E-poster
Keyword(s): Clinical outcome, Myeloma, Refractory, Relapse
{{ help_message }}
{{filter}}


