UPDATED RESULTS OF A SYSTEMATIC REVIEW OF THE RELATIVE EFFECTIVENESS OF TREATMENTS IN RELAPSED / REFRACTORY MULTIPLE MYELOMA
(Abstract release date: 05/19/16)
EHA Library. Maguire Á. 06/09/16; 132849; E1300
Disclosure(s): This research was funded by Cogentia Healthcare Consulting through a research grant from Celgene UK Ltd. Additionally co-author GC has relationships with Celgene, Janssen & Takeda Oncology (consultancy, research funding & speakers bureau); Sanofi & Amgen (consultancy & speakers bureau); BMS (consultancy). Co-author MO’D has a relationship with Celgene (honoraria & research funding). ÁM and KR do not receive any direct funds from Celgene but have a research grant from Cogentia Healthcare Consulting.

Ms. Áine Maguire
Contributions
Contributions
Abstract
Abstract: E1300
Type: Eposter Presentation
Background
Outcomes for multiple myeloma (MM) have improved with the introduction of novel therapies, and ongoing trials suggest positive outlooks for those with relapsed/refractory MM (rrMM). However, head-to-head clinical trials across treatment options are limited, and as such the evidence on relative effectiveness to inform best practice is lacking. A recent systematic review1 attempted to address this via a mixed treatment comparison using data from randomised control trials (RCTs) published before 2015. A network meta-analysis (NMA) was developed to estimate relative treatment effectiveness in this review, and two evidence networks were compiled, but no comparisons could be drawn across networks.
Aims
This systematic review is an update to a previously published study and aims to estimate the relative effectiveness of treatments for rrMM using the most up to date information available.
Methods
The literature search for the previous analysis was conducted in August and repeated again in December 2014. The search was then repeated January 2016 to identify further RCTs which might have been published in the interim. Data was extracted from all RCTs that reported median duration of progression-free survival (PFS), overall survival (OS) or time to progression (TTP) as a primary or secondary treatment outcome. A Bayesian NMA using non-informative prior distributions and assuming fixed effects was fitted due to scarcity of data in the networks. The number of prior treatment lines among patients recruited into trials in rrMM varied (1-5) and trials conducted in heavily pre-treated and refractory patient populations (a median of 3 or more prior lines of therapy) were excluded from the presented analysis in an attempt to reduce some heterogeneity.
Results
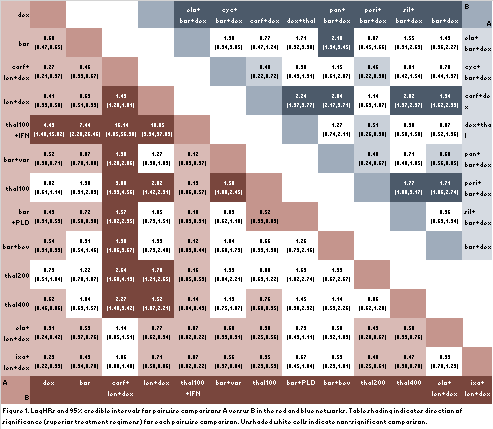
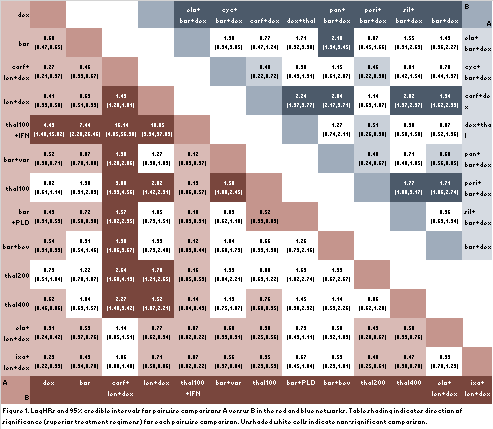
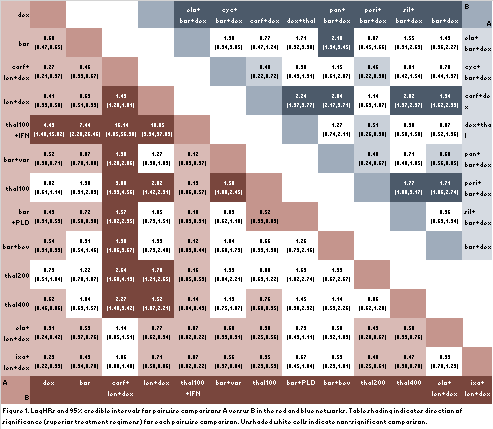
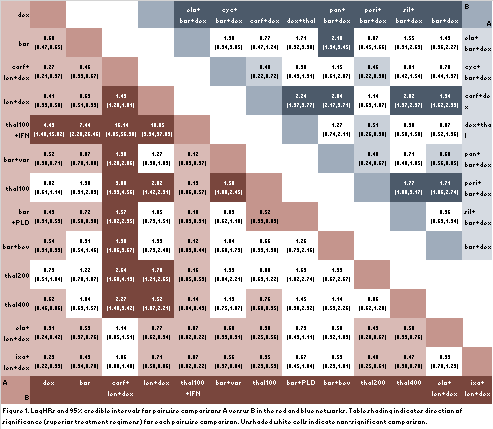
14 RCTs were included in the initial analysis1. These 14 trials assessed 16 different treatment regimens. From the updated review, 5 new RCTs which presented PFS or TTP data for 5 additional treatment regimens were identified to be included into the existing NMA. The combined trials form two separate evidence networks; all pairwise comparisons in each network were estimated in the analysis (figure 1). No relative effects between the two networks could be estimated.In the larger evidence network, novel agents combined with len+dex had superior outcomes with carf+len+dex being the most effective treatment, followed by ixa+len+dex, and then elo+len+dex. In the other, smaller evidence network, bort+dex+pan was the most effective treatment, followed by bort+dex+cyc.
Conclusion
The availability of treatments for rrMM is rapidly increasing. Within a year of conducting an initial systematic review the PFS and TTP outcomes of five additional RCTs of treatments for rrMM were released. Results of the larger network suggest that novel agents combined with len+dex have superior outcomes compared to other treatment options in the network. Less inferences can be drawn from the smaller network; of the newly included RCTs bort+dex+cyc ranked second in the network, whilst new treatment regimens elo+bor+dex and carf+dex ranked lower, and demonstrated no significant superiority relative to all other treatments in the network. The networks are not connected and as such it is impossible to make comparisons between the two regarding overall effectiveness of treatments. More RCTs comparing existing treatment regimens would greatly supplement these comparisons and allow for greater certainty. Nonetheless, the presented analysis is a significant step in evidence-based assessment for treatment in rrMM which indicates that novel agents combined with len+dex substantially improve treatment outcomes.
Session topic: E-poster
Keyword(s): Meta-analysis, Multiple myeloma, Systematic review, Treatment
Type: Eposter Presentation
Background
Outcomes for multiple myeloma (MM) have improved with the introduction of novel therapies, and ongoing trials suggest positive outlooks for those with relapsed/refractory MM (rrMM). However, head-to-head clinical trials across treatment options are limited, and as such the evidence on relative effectiveness to inform best practice is lacking. A recent systematic review1 attempted to address this via a mixed treatment comparison using data from randomised control trials (RCTs) published before 2015. A network meta-analysis (NMA) was developed to estimate relative treatment effectiveness in this review, and two evidence networks were compiled, but no comparisons could be drawn across networks.
Aims
This systematic review is an update to a previously published study and aims to estimate the relative effectiveness of treatments for rrMM using the most up to date information available.
Methods
The literature search for the previous analysis was conducted in August and repeated again in December 2014. The search was then repeated January 2016 to identify further RCTs which might have been published in the interim. Data was extracted from all RCTs that reported median duration of progression-free survival (PFS), overall survival (OS) or time to progression (TTP) as a primary or secondary treatment outcome. A Bayesian NMA using non-informative prior distributions and assuming fixed effects was fitted due to scarcity of data in the networks. The number of prior treatment lines among patients recruited into trials in rrMM varied (1-5) and trials conducted in heavily pre-treated and refractory patient populations (a median of 3 or more prior lines of therapy) were excluded from the presented analysis in an attempt to reduce some heterogeneity.
Results
14 RCTs were included in the initial analysis1. These 14 trials assessed 16 different treatment regimens. From the updated review, 5 new RCTs which presented PFS or TTP data for 5 additional treatment regimens were identified to be included into the existing NMA. The combined trials form two separate evidence networks; all pairwise comparisons in each network were estimated in the analysis (figure 1). No relative effects between the two networks could be estimated.In the larger evidence network, novel agents combined with len+dex had superior outcomes with carf+len+dex being the most effective treatment, followed by ixa+len+dex, and then elo+len+dex. In the other, smaller evidence network, bort+dex+pan was the most effective treatment, followed by bort+dex+cyc.
Conclusion
The availability of treatments for rrMM is rapidly increasing. Within a year of conducting an initial systematic review the PFS and TTP outcomes of five additional RCTs of treatments for rrMM were released. Results of the larger network suggest that novel agents combined with len+dex have superior outcomes compared to other treatment options in the network. Less inferences can be drawn from the smaller network; of the newly included RCTs bort+dex+cyc ranked second in the network, whilst new treatment regimens elo+bor+dex and carf+dex ranked lower, and demonstrated no significant superiority relative to all other treatments in the network. The networks are not connected and as such it is impossible to make comparisons between the two regarding overall effectiveness of treatments. More RCTs comparing existing treatment regimens would greatly supplement these comparisons and allow for greater certainty. Nonetheless, the presented analysis is a significant step in evidence-based assessment for treatment in rrMM which indicates that novel agents combined with len+dex substantially improve treatment outcomes.
Session topic: E-poster
Keyword(s): Meta-analysis, Multiple myeloma, Systematic review, Treatment
Abstract: E1300
Type: Eposter Presentation
Background
Outcomes for multiple myeloma (MM) have improved with the introduction of novel therapies, and ongoing trials suggest positive outlooks for those with relapsed/refractory MM (rrMM). However, head-to-head clinical trials across treatment options are limited, and as such the evidence on relative effectiveness to inform best practice is lacking. A recent systematic review1 attempted to address this via a mixed treatment comparison using data from randomised control trials (RCTs) published before 2015. A network meta-analysis (NMA) was developed to estimate relative treatment effectiveness in this review, and two evidence networks were compiled, but no comparisons could be drawn across networks.
Aims
This systematic review is an update to a previously published study and aims to estimate the relative effectiveness of treatments for rrMM using the most up to date information available.
Methods
The literature search for the previous analysis was conducted in August and repeated again in December 2014. The search was then repeated January 2016 to identify further RCTs which might have been published in the interim. Data was extracted from all RCTs that reported median duration of progression-free survival (PFS), overall survival (OS) or time to progression (TTP) as a primary or secondary treatment outcome. A Bayesian NMA using non-informative prior distributions and assuming fixed effects was fitted due to scarcity of data in the networks. The number of prior treatment lines among patients recruited into trials in rrMM varied (1-5) and trials conducted in heavily pre-treated and refractory patient populations (a median of 3 or more prior lines of therapy) were excluded from the presented analysis in an attempt to reduce some heterogeneity.
Results
14 RCTs were included in the initial analysis1. These 14 trials assessed 16 different treatment regimens. From the updated review, 5 new RCTs which presented PFS or TTP data for 5 additional treatment regimens were identified to be included into the existing NMA. The combined trials form two separate evidence networks; all pairwise comparisons in each network were estimated in the analysis (figure 1). No relative effects between the two networks could be estimated.In the larger evidence network, novel agents combined with len+dex had superior outcomes with carf+len+dex being the most effective treatment, followed by ixa+len+dex, and then elo+len+dex. In the other, smaller evidence network, bort+dex+pan was the most effective treatment, followed by bort+dex+cyc.
Conclusion
The availability of treatments for rrMM is rapidly increasing. Within a year of conducting an initial systematic review the PFS and TTP outcomes of five additional RCTs of treatments for rrMM were released. Results of the larger network suggest that novel agents combined with len+dex have superior outcomes compared to other treatment options in the network. Less inferences can be drawn from the smaller network; of the newly included RCTs bort+dex+cyc ranked second in the network, whilst new treatment regimens elo+bor+dex and carf+dex ranked lower, and demonstrated no significant superiority relative to all other treatments in the network. The networks are not connected and as such it is impossible to make comparisons between the two regarding overall effectiveness of treatments. More RCTs comparing existing treatment regimens would greatly supplement these comparisons and allow for greater certainty. Nonetheless, the presented analysis is a significant step in evidence-based assessment for treatment in rrMM which indicates that novel agents combined with len+dex substantially improve treatment outcomes.
Session topic: E-poster
Keyword(s): Meta-analysis, Multiple myeloma, Systematic review, Treatment
Type: Eposter Presentation
Background
Outcomes for multiple myeloma (MM) have improved with the introduction of novel therapies, and ongoing trials suggest positive outlooks for those with relapsed/refractory MM (rrMM). However, head-to-head clinical trials across treatment options are limited, and as such the evidence on relative effectiveness to inform best practice is lacking. A recent systematic review1 attempted to address this via a mixed treatment comparison using data from randomised control trials (RCTs) published before 2015. A network meta-analysis (NMA) was developed to estimate relative treatment effectiveness in this review, and two evidence networks were compiled, but no comparisons could be drawn across networks.
Aims
This systematic review is an update to a previously published study and aims to estimate the relative effectiveness of treatments for rrMM using the most up to date information available.
Methods
The literature search for the previous analysis was conducted in August and repeated again in December 2014. The search was then repeated January 2016 to identify further RCTs which might have been published in the interim. Data was extracted from all RCTs that reported median duration of progression-free survival (PFS), overall survival (OS) or time to progression (TTP) as a primary or secondary treatment outcome. A Bayesian NMA using non-informative prior distributions and assuming fixed effects was fitted due to scarcity of data in the networks. The number of prior treatment lines among patients recruited into trials in rrMM varied (1-5) and trials conducted in heavily pre-treated and refractory patient populations (a median of 3 or more prior lines of therapy) were excluded from the presented analysis in an attempt to reduce some heterogeneity.
Results
14 RCTs were included in the initial analysis1. These 14 trials assessed 16 different treatment regimens. From the updated review, 5 new RCTs which presented PFS or TTP data for 5 additional treatment regimens were identified to be included into the existing NMA. The combined trials form two separate evidence networks; all pairwise comparisons in each network were estimated in the analysis (figure 1). No relative effects between the two networks could be estimated.In the larger evidence network, novel agents combined with len+dex had superior outcomes with carf+len+dex being the most effective treatment, followed by ixa+len+dex, and then elo+len+dex. In the other, smaller evidence network, bort+dex+pan was the most effective treatment, followed by bort+dex+cyc.
Conclusion
The availability of treatments for rrMM is rapidly increasing. Within a year of conducting an initial systematic review the PFS and TTP outcomes of five additional RCTs of treatments for rrMM were released. Results of the larger network suggest that novel agents combined with len+dex have superior outcomes compared to other treatment options in the network. Less inferences can be drawn from the smaller network; of the newly included RCTs bort+dex+cyc ranked second in the network, whilst new treatment regimens elo+bor+dex and carf+dex ranked lower, and demonstrated no significant superiority relative to all other treatments in the network. The networks are not connected and as such it is impossible to make comparisons between the two regarding overall effectiveness of treatments. More RCTs comparing existing treatment regimens would greatly supplement these comparisons and allow for greater certainty. Nonetheless, the presented analysis is a significant step in evidence-based assessment for treatment in rrMM which indicates that novel agents combined with len+dex substantially improve treatment outcomes.
Session topic: E-poster
Keyword(s): Meta-analysis, Multiple myeloma, Systematic review, Treatment
{{ help_message }}
{{filter}}


