PRACTICE PATTERNS AND OUTCOMES IN ELDERLY U.S. PATIENTS WITH RELAPSED / REFRACTORY MULTIPLE MYELOMA (RRMM)
(Abstract release date: 05/19/16)
EHA Library. Romanus D. 06/09/16; 132837; E1288

Dr. Dorothy Romanus
Contributions
Contributions
Abstract
Abstract: E1288
Type: Eposter Presentation
Background
Multiple myeloma (MM) is a disease of the elderly; median age at diagnosis is 70 yrs (Larocca 2015). The advent of novel therapies has improved survival (OS) among newly diagnosed MM (NDMM) patients (pts) (Kumar 2014). But, the link between therapeutic regimens and OS benefit in elderly pts is not clearly established (Kumar 2014; Verlest 2012). Real-world information regarding prescribing patterns and clinical outcomes in elderly pts with RRMM is limited.
Aims
To describe the prescribing patterns and clinical outcomes, and to evaluate the impact of age on progression-free survival (PFS) and OS in elderly RRMM pts initiating second line therapy (2LT) in a large, national database in the U.S.
Methods
In this retrospective cohort study of an electronic medical records (EMR) database, NDMM adult pts initiating first-line therapy (1LT) between 1/2008 and 12/2014 were included and 2LT was identified accordingly: 1) retreatment after a treatment gap of >3 months of 1LT, or 2) a switch to another drug combination after starting 1LT. Third-line therapy (3LT) began with a switch in regimen post 2LT. Pts with salvage stem cell transplants (SCT) were excluded. Time to new line of therapy (TTNT) or death was used as a surrogate for PFS. Cox proportional hazard models for TTNT and OS were conducted from start of 2LT. Pts were censored at loss to follow up or the end of study period (6/30/2015).
Results
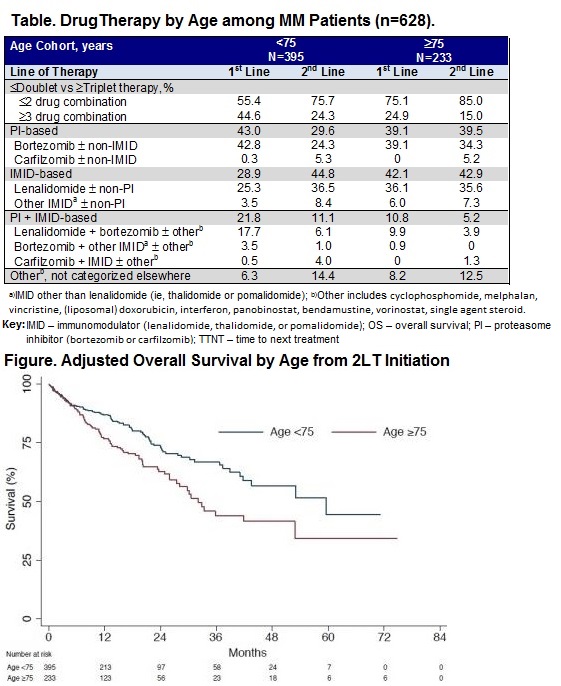
Among 628 pts with 1LT and 2LT, 37.1% were ≥75 yrs of age (yo) at start of 2LT, 51% male; 2% of those ≥75 yr vs 30% of those <75 yr underwent frontline SCT. Pts ≥75 yo had a higher comorbidity burden (mean Charlson Comorbidity score [CCI]: 2.1 vs 1.6), and a higher proportion had cardiovascular disease (CVD [38.6% vs 27.3%]) than those <75 yo at start of SLT. Median follow-up from start of 2LT was 13.0 mos (IQR: 5.2, 23.3).Younger pts were 2-fold more likely to receive more intensive therapy with a proteasome inhibitor + immunomodulatory drug (PI+IMID)-based combination both in 1LT (21.8% vs 10.8%) and in 2LT (11.1% vs 5.2%) compared to ≥75 yo (Table). In 1LT, older age was associated with an increased use of IMID-based therapies (42.1% vs 28.9% among ≥75 vs <75 yo). In 2LT, older age was associated with a higher frequency of PI-based therapies, 39.5% vs 29.6% in the younger cohort. OS probabilities at 1 yr and 2 yrs were 84.6% and 68.0% for those <75 yrs and 72.3% and 57.4% for those ≥75 yrs. Adjusting for observed confounders (gender, race, cytogenetic risk, CCI, CVD, yr of diagnosis, 1LT and 2LT regimen type), older age was associated with a significantly higher mortality risk after initiation of 2LT (HR: 1.57 [95% CI: 1.2, 2.1], P<0.01, for age ≥75 vs <75 yrs) (Figure). Median TTNT was 16.6 mos (95%CI: 13.5, 19.1) for pts <75 yrs and 13.8 mos (95% CI: 11.7, 17.8) for pts ≥75 yo. Age was not significantly associated with TTNT in 2LT in multivariate analyses.
Conclusion
In 1LT and 2LT in MM, older age appeared to impact treatment choice with less intensive therapy. The majority of patients received ≥1 novel agent irrespective of age; however, elderly pts were more likely to initiate IMID-based therapy in 1LT and PI-based therapy in 2LT compared to younger pts. Older age was associated with significantly worse OS outcomes after start of 2LT in the real-world.References: Larocca et al. Blood. 2015;126:2179-85; Verlest et al. Haematologica.2012; 97: 242; Kumar et al. Leukemia. 2014;28:5:1122-1128
Session topic: E-poster
Keyword(s): Clinical outcome, Elderly, Myeloma
Type: Eposter Presentation
Background
Multiple myeloma (MM) is a disease of the elderly; median age at diagnosis is 70 yrs (Larocca 2015). The advent of novel therapies has improved survival (OS) among newly diagnosed MM (NDMM) patients (pts) (Kumar 2014). But, the link between therapeutic regimens and OS benefit in elderly pts is not clearly established (Kumar 2014; Verlest 2012). Real-world information regarding prescribing patterns and clinical outcomes in elderly pts with RRMM is limited.
Aims
To describe the prescribing patterns and clinical outcomes, and to evaluate the impact of age on progression-free survival (PFS) and OS in elderly RRMM pts initiating second line therapy (2LT) in a large, national database in the U.S.
Methods
In this retrospective cohort study of an electronic medical records (EMR) database, NDMM adult pts initiating first-line therapy (1LT) between 1/2008 and 12/2014 were included and 2LT was identified accordingly: 1) retreatment after a treatment gap of >3 months of 1LT, or 2) a switch to another drug combination after starting 1LT. Third-line therapy (3LT) began with a switch in regimen post 2LT. Pts with salvage stem cell transplants (SCT) were excluded. Time to new line of therapy (TTNT) or death was used as a surrogate for PFS. Cox proportional hazard models for TTNT and OS were conducted from start of 2LT. Pts were censored at loss to follow up or the end of study period (6/30/2015).
Results
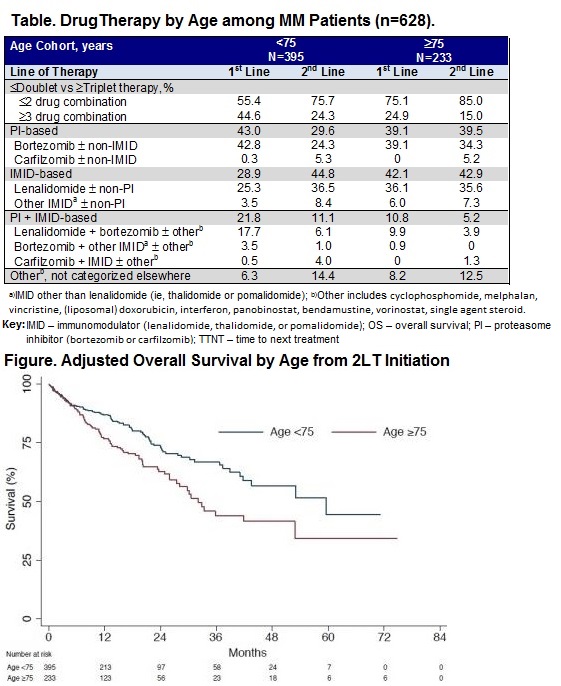
Among 628 pts with 1LT and 2LT, 37.1% were ≥75 yrs of age (yo) at start of 2LT, 51% male; 2% of those ≥75 yr vs 30% of those <75 yr underwent frontline SCT. Pts ≥75 yo had a higher comorbidity burden (mean Charlson Comorbidity score [CCI]: 2.1 vs 1.6), and a higher proportion had cardiovascular disease (CVD [38.6% vs 27.3%]) than those <75 yo at start of SLT. Median follow-up from start of 2LT was 13.0 mos (IQR: 5.2, 23.3).Younger pts were 2-fold more likely to receive more intensive therapy with a proteasome inhibitor + immunomodulatory drug (PI+IMID)-based combination both in 1LT (21.8% vs 10.8%) and in 2LT (11.1% vs 5.2%) compared to ≥75 yo (Table). In 1LT, older age was associated with an increased use of IMID-based therapies (42.1% vs 28.9% among ≥75 vs <75 yo). In 2LT, older age was associated with a higher frequency of PI-based therapies, 39.5% vs 29.6% in the younger cohort. OS probabilities at 1 yr and 2 yrs were 84.6% and 68.0% for those <75 yrs and 72.3% and 57.4% for those ≥75 yrs. Adjusting for observed confounders (gender, race, cytogenetic risk, CCI, CVD, yr of diagnosis, 1LT and 2LT regimen type), older age was associated with a significantly higher mortality risk after initiation of 2LT (HR: 1.57 [95% CI: 1.2, 2.1], P<0.01, for age ≥75 vs <75 yrs) (Figure). Median TTNT was 16.6 mos (95%CI: 13.5, 19.1) for pts <75 yrs and 13.8 mos (95% CI: 11.7, 17.8) for pts ≥75 yo. Age was not significantly associated with TTNT in 2LT in multivariate analyses.
Conclusion
In 1LT and 2LT in MM, older age appeared to impact treatment choice with less intensive therapy. The majority of patients received ≥1 novel agent irrespective of age; however, elderly pts were more likely to initiate IMID-based therapy in 1LT and PI-based therapy in 2LT compared to younger pts. Older age was associated with significantly worse OS outcomes after start of 2LT in the real-world.References: Larocca et al. Blood. 2015;126:2179-85; Verlest et al. Haematologica.2012; 97: 242; Kumar et al. Leukemia. 2014;28:5:1122-1128
Session topic: E-poster
Keyword(s): Clinical outcome, Elderly, Myeloma
Abstract: E1288
Type: Eposter Presentation
Background
Multiple myeloma (MM) is a disease of the elderly; median age at diagnosis is 70 yrs (Larocca 2015). The advent of novel therapies has improved survival (OS) among newly diagnosed MM (NDMM) patients (pts) (Kumar 2014). But, the link between therapeutic regimens and OS benefit in elderly pts is not clearly established (Kumar 2014; Verlest 2012). Real-world information regarding prescribing patterns and clinical outcomes in elderly pts with RRMM is limited.
Aims
To describe the prescribing patterns and clinical outcomes, and to evaluate the impact of age on progression-free survival (PFS) and OS in elderly RRMM pts initiating second line therapy (2LT) in a large, national database in the U.S.
Methods
In this retrospective cohort study of an electronic medical records (EMR) database, NDMM adult pts initiating first-line therapy (1LT) between 1/2008 and 12/2014 were included and 2LT was identified accordingly: 1) retreatment after a treatment gap of >3 months of 1LT, or 2) a switch to another drug combination after starting 1LT. Third-line therapy (3LT) began with a switch in regimen post 2LT. Pts with salvage stem cell transplants (SCT) were excluded. Time to new line of therapy (TTNT) or death was used as a surrogate for PFS. Cox proportional hazard models for TTNT and OS were conducted from start of 2LT. Pts were censored at loss to follow up or the end of study period (6/30/2015).
Results
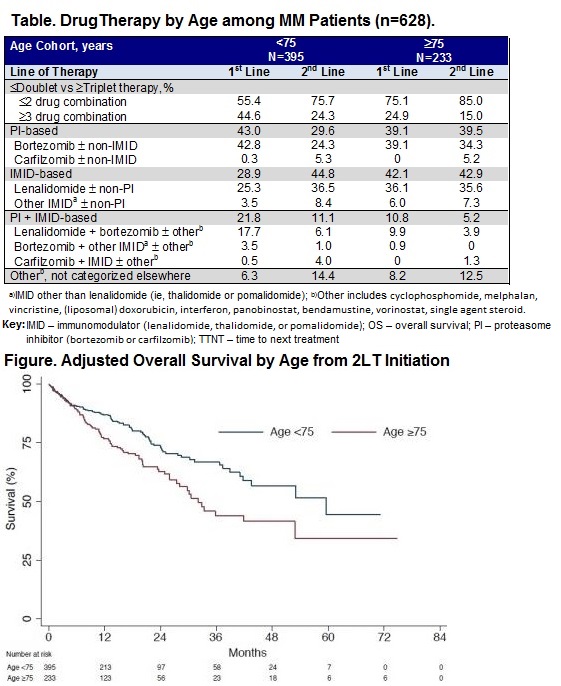
Among 628 pts with 1LT and 2LT, 37.1% were ≥75 yrs of age (yo) at start of 2LT, 51% male; 2% of those ≥75 yr vs 30% of those <75 yr underwent frontline SCT. Pts ≥75 yo had a higher comorbidity burden (mean Charlson Comorbidity score [CCI]: 2.1 vs 1.6), and a higher proportion had cardiovascular disease (CVD [38.6% vs 27.3%]) than those <75 yo at start of SLT. Median follow-up from start of 2LT was 13.0 mos (IQR: 5.2, 23.3).Younger pts were 2-fold more likely to receive more intensive therapy with a proteasome inhibitor + immunomodulatory drug (PI+IMID)-based combination both in 1LT (21.8% vs 10.8%) and in 2LT (11.1% vs 5.2%) compared to ≥75 yo (Table). In 1LT, older age was associated with an increased use of IMID-based therapies (42.1% vs 28.9% among ≥75 vs <75 yo). In 2LT, older age was associated with a higher frequency of PI-based therapies, 39.5% vs 29.6% in the younger cohort. OS probabilities at 1 yr and 2 yrs were 84.6% and 68.0% for those <75 yrs and 72.3% and 57.4% for those ≥75 yrs. Adjusting for observed confounders (gender, race, cytogenetic risk, CCI, CVD, yr of diagnosis, 1LT and 2LT regimen type), older age was associated with a significantly higher mortality risk after initiation of 2LT (HR: 1.57 [95% CI: 1.2, 2.1], P<0.01, for age ≥75 vs <75 yrs) (Figure). Median TTNT was 16.6 mos (95%CI: 13.5, 19.1) for pts <75 yrs and 13.8 mos (95% CI: 11.7, 17.8) for pts ≥75 yo. Age was not significantly associated with TTNT in 2LT in multivariate analyses.
Conclusion
In 1LT and 2LT in MM, older age appeared to impact treatment choice with less intensive therapy. The majority of patients received ≥1 novel agent irrespective of age; however, elderly pts were more likely to initiate IMID-based therapy in 1LT and PI-based therapy in 2LT compared to younger pts. Older age was associated with significantly worse OS outcomes after start of 2LT in the real-world.References: Larocca et al. Blood. 2015;126:2179-85; Verlest et al. Haematologica.2012; 97: 242; Kumar et al. Leukemia. 2014;28:5:1122-1128
Session topic: E-poster
Keyword(s): Clinical outcome, Elderly, Myeloma
Type: Eposter Presentation
Background
Multiple myeloma (MM) is a disease of the elderly; median age at diagnosis is 70 yrs (Larocca 2015). The advent of novel therapies has improved survival (OS) among newly diagnosed MM (NDMM) patients (pts) (Kumar 2014). But, the link between therapeutic regimens and OS benefit in elderly pts is not clearly established (Kumar 2014; Verlest 2012). Real-world information regarding prescribing patterns and clinical outcomes in elderly pts with RRMM is limited.
Aims
To describe the prescribing patterns and clinical outcomes, and to evaluate the impact of age on progression-free survival (PFS) and OS in elderly RRMM pts initiating second line therapy (2LT) in a large, national database in the U.S.
Methods
In this retrospective cohort study of an electronic medical records (EMR) database, NDMM adult pts initiating first-line therapy (1LT) between 1/2008 and 12/2014 were included and 2LT was identified accordingly: 1) retreatment after a treatment gap of >3 months of 1LT, or 2) a switch to another drug combination after starting 1LT. Third-line therapy (3LT) began with a switch in regimen post 2LT. Pts with salvage stem cell transplants (SCT) were excluded. Time to new line of therapy (TTNT) or death was used as a surrogate for PFS. Cox proportional hazard models for TTNT and OS were conducted from start of 2LT. Pts were censored at loss to follow up or the end of study period (6/30/2015).
Results
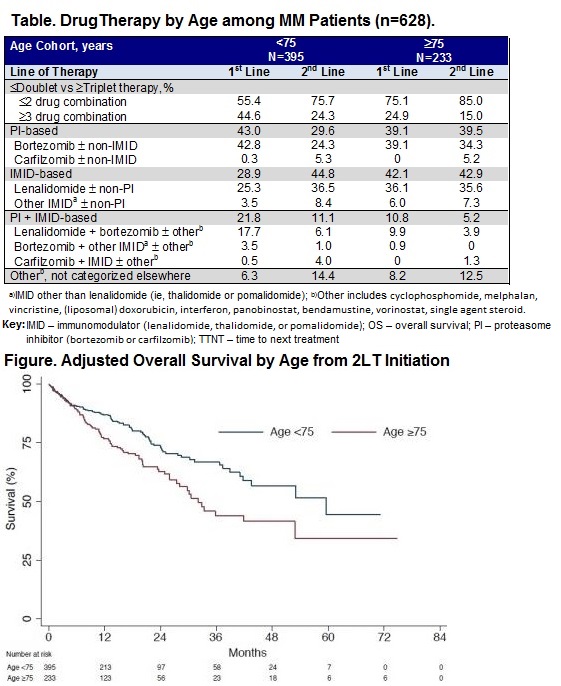
Among 628 pts with 1LT and 2LT, 37.1% were ≥75 yrs of age (yo) at start of 2LT, 51% male; 2% of those ≥75 yr vs 30% of those <75 yr underwent frontline SCT. Pts ≥75 yo had a higher comorbidity burden (mean Charlson Comorbidity score [CCI]: 2.1 vs 1.6), and a higher proportion had cardiovascular disease (CVD [38.6% vs 27.3%]) than those <75 yo at start of SLT. Median follow-up from start of 2LT was 13.0 mos (IQR: 5.2, 23.3).Younger pts were 2-fold more likely to receive more intensive therapy with a proteasome inhibitor + immunomodulatory drug (PI+IMID)-based combination both in 1LT (21.8% vs 10.8%) and in 2LT (11.1% vs 5.2%) compared to ≥75 yo (Table). In 1LT, older age was associated with an increased use of IMID-based therapies (42.1% vs 28.9% among ≥75 vs <75 yo). In 2LT, older age was associated with a higher frequency of PI-based therapies, 39.5% vs 29.6% in the younger cohort. OS probabilities at 1 yr and 2 yrs were 84.6% and 68.0% for those <75 yrs and 72.3% and 57.4% for those ≥75 yrs. Adjusting for observed confounders (gender, race, cytogenetic risk, CCI, CVD, yr of diagnosis, 1LT and 2LT regimen type), older age was associated with a significantly higher mortality risk after initiation of 2LT (HR: 1.57 [95% CI: 1.2, 2.1], P<0.01, for age ≥75 vs <75 yrs) (Figure). Median TTNT was 16.6 mos (95%CI: 13.5, 19.1) for pts <75 yrs and 13.8 mos (95% CI: 11.7, 17.8) for pts ≥75 yo. Age was not significantly associated with TTNT in 2LT in multivariate analyses.
Conclusion
In 1LT and 2LT in MM, older age appeared to impact treatment choice with less intensive therapy. The majority of patients received ≥1 novel agent irrespective of age; however, elderly pts were more likely to initiate IMID-based therapy in 1LT and PI-based therapy in 2LT compared to younger pts. Older age was associated with significantly worse OS outcomes after start of 2LT in the real-world.References: Larocca et al. Blood. 2015;126:2179-85; Verlest et al. Haematologica.2012; 97: 242; Kumar et al. Leukemia. 2014;28:5:1122-1128
Session topic: E-poster
Keyword(s): Clinical outcome, Elderly, Myeloma
{{ help_message }}
{{filter}}


