PRACTICE PATTERNS AND OUTCOMES IN U.S. PATIENTS (PTS) WITH RELAPSED / REFRACTORY MULTIPLE MYELOMA (RRMM) AND COMORBID RENAL DYSFUNCTION (RD) AND/OR CARDIOVASCULAR DISEASE (CVD)
(Abstract release date: 05/19/16)
EHA Library. Yong C. 06/09/16; 132826; E1277

Dr. Candice Yong
Contributions
Contributions
Abstract
Abstract: E1277
Type: Eposter Presentation
Background
Multiple myeloma (MM) is a disease of the elderly, many of whom often present with comorbidities including RD and CVD (Gupta 2015; Dimopoulus 2015). While the presence of RD and/or CVD may influence RRMM treatment choices, there is limited real-world data on prescribing patterns and outcomes in these patient populations (Castelli 2014; Larocca 2015).
Aims
To describe the prevalence of RD and CVD over time, and the variation in prescribing patterns and clinical outcomes (progression-free survival (PFS) and overall survival (OS)) by comorbidity profile in RRMM pts initiating second line therapy (2LT).
Methods
This was a retrospective cohort study using a large national EMR database in the U.S. Newly diagnosed adult MM patients initiating first line therapy (1LT) between 1/2008 and 12/2014 were followed until death/loss to follow up or the end of study period (6/30/2015). 2LT was identified by: 1) retreatment after a treatment gap of >3 months after 1LT discontinuation, or 2) a switch to another drug combination after starting 1LT. Comorbid RD was based on presence of a diagnosis (dx) code or a lab value (creatinine clearance <40ml/min or serum creatinine >2 mg/dL) in the 12 months prior to start of 1LT through the start of 2LT; and comorbid CVD was based on dx codes in the same timeframe. Time to new treatment (TTNT) or death was used as a surrogate for PFS. Kaplan-Meier analyses were performed for TTNT/OS from start of 2LT.
Results
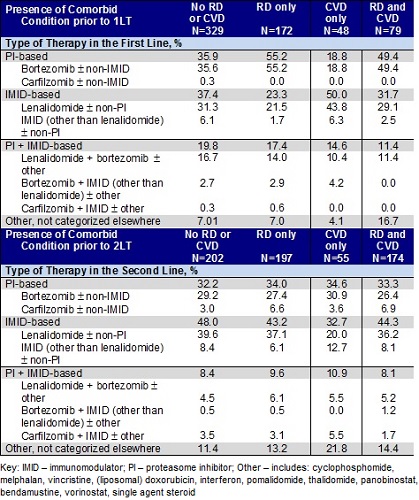
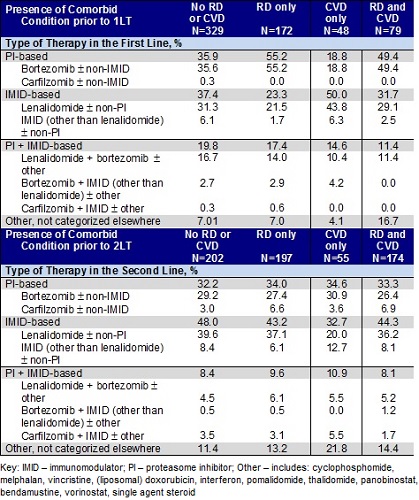
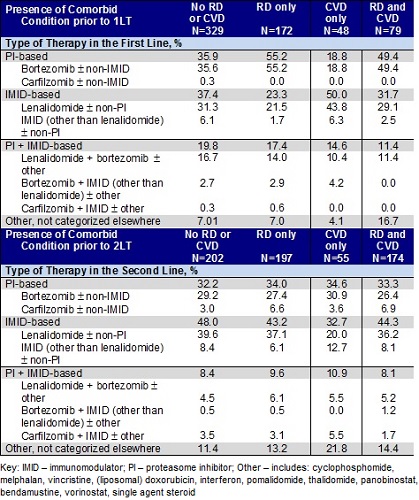
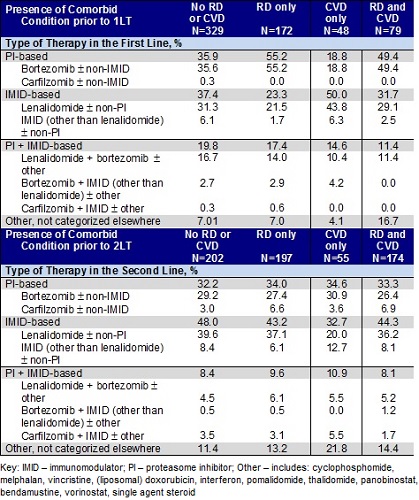
Among 628 RRMM pts (mean age 69 years), 27.4% had comorbid RD, 7.6% had comorbid CVD, and 12.6% had both RD and CVD prior to 1LT; this increased to 31.4%, 8.8%, and 27.7%, respectively, prior to 2LT. The distribution of treatments across 1LT and 2LT is shown in Table 1. In 1LT, pts with RD ± CVD were most likely to receive proteasome inhibitor (PI)-based therapies; in contrast, pts with CVD only were most likely to receive immunomodulatory drug (IMID)-based therapies. In 2LT, the use of IMID-based therapies was most common, except among pts with CVD only where a similar proportion used IMID-based or PI-based therapies (approx. one-third). Additionally, intensive regimens (PI+IMID) were more common for all pts regardless of comorbidity in 1LT compared to 2LT. Median TTNT from 2LT initiation was 14.3 months (95% CI: 9.2, 19.1) for pts with CVD only, 13.7 months (95% CI: 11.4, 17.8) for pts with RD only, 12.3 months (95% CI: 8.4, 16.6) for pts with RD and CVD, and 20.1 months (95% CI: 16.6, 24.4) for pts without CVD or RD. OS at 1 yr and 2 yrs from 2LT initiation were 77.8% and 64.1% for those with CVD only, 77.4% and 58.5% for those with RD only, 72.7% and 51.6% for those with CVD and RD, and 88.2% and 78.4% for pts without CVD or RD (log-rank test, P < 0.05).
Conclusion
Among pts receiving 2LT for RRMM, prevalence of RD and/or CVD increased from 48% to 68% during the MM clinical course. The type of therapy varied by presence of comorbidity for 1LT but to a lesser extent for 2LT. Pts with RD and/or CVD had a shorter TTNT and a lower 1- and 2-yr OS probability relative to those without these comorbidities.References: Castelli, et al. Expert Rev. Anticancer Ther. 2014;14:2:199–215; Dimopoulus, et al. Cancer Treatment Reviews. 2015; 41:827–835; Gupta, et al. Journal of Geriatric Oncology. 2015;6:178-184; Larocca, et al. Blood. 2015;126:19:2179-2185.
Session topic: E-poster
Keyword(s): Comorbidities, Multiple myeloma
Type: Eposter Presentation
Background
Multiple myeloma (MM) is a disease of the elderly, many of whom often present with comorbidities including RD and CVD (Gupta 2015; Dimopoulus 2015). While the presence of RD and/or CVD may influence RRMM treatment choices, there is limited real-world data on prescribing patterns and outcomes in these patient populations (Castelli 2014; Larocca 2015).
Aims
To describe the prevalence of RD and CVD over time, and the variation in prescribing patterns and clinical outcomes (progression-free survival (PFS) and overall survival (OS)) by comorbidity profile in RRMM pts initiating second line therapy (2LT).
Methods
This was a retrospective cohort study using a large national EMR database in the U.S. Newly diagnosed adult MM patients initiating first line therapy (1LT) between 1/2008 and 12/2014 were followed until death/loss to follow up or the end of study period (6/30/2015). 2LT was identified by: 1) retreatment after a treatment gap of >3 months after 1LT discontinuation, or 2) a switch to another drug combination after starting 1LT. Comorbid RD was based on presence of a diagnosis (dx) code or a lab value (creatinine clearance <40ml/min or serum creatinine >2 mg/dL) in the 12 months prior to start of 1LT through the start of 2LT; and comorbid CVD was based on dx codes in the same timeframe. Time to new treatment (TTNT) or death was used as a surrogate for PFS. Kaplan-Meier analyses were performed for TTNT/OS from start of 2LT.
Results
Among 628 RRMM pts (mean age 69 years), 27.4% had comorbid RD, 7.6% had comorbid CVD, and 12.6% had both RD and CVD prior to 1LT; this increased to 31.4%, 8.8%, and 27.7%, respectively, prior to 2LT. The distribution of treatments across 1LT and 2LT is shown in Table 1. In 1LT, pts with RD ± CVD were most likely to receive proteasome inhibitor (PI)-based therapies; in contrast, pts with CVD only were most likely to receive immunomodulatory drug (IMID)-based therapies. In 2LT, the use of IMID-based therapies was most common, except among pts with CVD only where a similar proportion used IMID-based or PI-based therapies (approx. one-third). Additionally, intensive regimens (PI+IMID) were more common for all pts regardless of comorbidity in 1LT compared to 2LT. Median TTNT from 2LT initiation was 14.3 months (95% CI: 9.2, 19.1) for pts with CVD only, 13.7 months (95% CI: 11.4, 17.8) for pts with RD only, 12.3 months (95% CI: 8.4, 16.6) for pts with RD and CVD, and 20.1 months (95% CI: 16.6, 24.4) for pts without CVD or RD. OS at 1 yr and 2 yrs from 2LT initiation were 77.8% and 64.1% for those with CVD only, 77.4% and 58.5% for those with RD only, 72.7% and 51.6% for those with CVD and RD, and 88.2% and 78.4% for pts without CVD or RD (log-rank test, P < 0.05).
Conclusion
Among pts receiving 2LT for RRMM, prevalence of RD and/or CVD increased from 48% to 68% during the MM clinical course. The type of therapy varied by presence of comorbidity for 1LT but to a lesser extent for 2LT. Pts with RD and/or CVD had a shorter TTNT and a lower 1- and 2-yr OS probability relative to those without these comorbidities.References: Castelli, et al. Expert Rev. Anticancer Ther. 2014;14:2:199–215; Dimopoulus, et al. Cancer Treatment Reviews. 2015; 41:827–835; Gupta, et al. Journal of Geriatric Oncology. 2015;6:178-184; Larocca, et al. Blood. 2015;126:19:2179-2185.
Session topic: E-poster
Keyword(s): Comorbidities, Multiple myeloma
Abstract: E1277
Type: Eposter Presentation
Background
Multiple myeloma (MM) is a disease of the elderly, many of whom often present with comorbidities including RD and CVD (Gupta 2015; Dimopoulus 2015). While the presence of RD and/or CVD may influence RRMM treatment choices, there is limited real-world data on prescribing patterns and outcomes in these patient populations (Castelli 2014; Larocca 2015).
Aims
To describe the prevalence of RD and CVD over time, and the variation in prescribing patterns and clinical outcomes (progression-free survival (PFS) and overall survival (OS)) by comorbidity profile in RRMM pts initiating second line therapy (2LT).
Methods
This was a retrospective cohort study using a large national EMR database in the U.S. Newly diagnosed adult MM patients initiating first line therapy (1LT) between 1/2008 and 12/2014 were followed until death/loss to follow up or the end of study period (6/30/2015). 2LT was identified by: 1) retreatment after a treatment gap of >3 months after 1LT discontinuation, or 2) a switch to another drug combination after starting 1LT. Comorbid RD was based on presence of a diagnosis (dx) code or a lab value (creatinine clearance <40ml/min or serum creatinine >2 mg/dL) in the 12 months prior to start of 1LT through the start of 2LT; and comorbid CVD was based on dx codes in the same timeframe. Time to new treatment (TTNT) or death was used as a surrogate for PFS. Kaplan-Meier analyses were performed for TTNT/OS from start of 2LT.
Results
Among 628 RRMM pts (mean age 69 years), 27.4% had comorbid RD, 7.6% had comorbid CVD, and 12.6% had both RD and CVD prior to 1LT; this increased to 31.4%, 8.8%, and 27.7%, respectively, prior to 2LT. The distribution of treatments across 1LT and 2LT is shown in Table 1. In 1LT, pts with RD ± CVD were most likely to receive proteasome inhibitor (PI)-based therapies; in contrast, pts with CVD only were most likely to receive immunomodulatory drug (IMID)-based therapies. In 2LT, the use of IMID-based therapies was most common, except among pts with CVD only where a similar proportion used IMID-based or PI-based therapies (approx. one-third). Additionally, intensive regimens (PI+IMID) were more common for all pts regardless of comorbidity in 1LT compared to 2LT. Median TTNT from 2LT initiation was 14.3 months (95% CI: 9.2, 19.1) for pts with CVD only, 13.7 months (95% CI: 11.4, 17.8) for pts with RD only, 12.3 months (95% CI: 8.4, 16.6) for pts with RD and CVD, and 20.1 months (95% CI: 16.6, 24.4) for pts without CVD or RD. OS at 1 yr and 2 yrs from 2LT initiation were 77.8% and 64.1% for those with CVD only, 77.4% and 58.5% for those with RD only, 72.7% and 51.6% for those with CVD and RD, and 88.2% and 78.4% for pts without CVD or RD (log-rank test, P < 0.05).
Conclusion
Among pts receiving 2LT for RRMM, prevalence of RD and/or CVD increased from 48% to 68% during the MM clinical course. The type of therapy varied by presence of comorbidity for 1LT but to a lesser extent for 2LT. Pts with RD and/or CVD had a shorter TTNT and a lower 1- and 2-yr OS probability relative to those without these comorbidities.References: Castelli, et al. Expert Rev. Anticancer Ther. 2014;14:2:199–215; Dimopoulus, et al. Cancer Treatment Reviews. 2015; 41:827–835; Gupta, et al. Journal of Geriatric Oncology. 2015;6:178-184; Larocca, et al. Blood. 2015;126:19:2179-2185.
Session topic: E-poster
Keyword(s): Comorbidities, Multiple myeloma
Type: Eposter Presentation
Background
Multiple myeloma (MM) is a disease of the elderly, many of whom often present with comorbidities including RD and CVD (Gupta 2015; Dimopoulus 2015). While the presence of RD and/or CVD may influence RRMM treatment choices, there is limited real-world data on prescribing patterns and outcomes in these patient populations (Castelli 2014; Larocca 2015).
Aims
To describe the prevalence of RD and CVD over time, and the variation in prescribing patterns and clinical outcomes (progression-free survival (PFS) and overall survival (OS)) by comorbidity profile in RRMM pts initiating second line therapy (2LT).
Methods
This was a retrospective cohort study using a large national EMR database in the U.S. Newly diagnosed adult MM patients initiating first line therapy (1LT) between 1/2008 and 12/2014 were followed until death/loss to follow up or the end of study period (6/30/2015). 2LT was identified by: 1) retreatment after a treatment gap of >3 months after 1LT discontinuation, or 2) a switch to another drug combination after starting 1LT. Comorbid RD was based on presence of a diagnosis (dx) code or a lab value (creatinine clearance <40ml/min or serum creatinine >2 mg/dL) in the 12 months prior to start of 1LT through the start of 2LT; and comorbid CVD was based on dx codes in the same timeframe. Time to new treatment (TTNT) or death was used as a surrogate for PFS. Kaplan-Meier analyses were performed for TTNT/OS from start of 2LT.
Results
Among 628 RRMM pts (mean age 69 years), 27.4% had comorbid RD, 7.6% had comorbid CVD, and 12.6% had both RD and CVD prior to 1LT; this increased to 31.4%, 8.8%, and 27.7%, respectively, prior to 2LT. The distribution of treatments across 1LT and 2LT is shown in Table 1. In 1LT, pts with RD ± CVD were most likely to receive proteasome inhibitor (PI)-based therapies; in contrast, pts with CVD only were most likely to receive immunomodulatory drug (IMID)-based therapies. In 2LT, the use of IMID-based therapies was most common, except among pts with CVD only where a similar proportion used IMID-based or PI-based therapies (approx. one-third). Additionally, intensive regimens (PI+IMID) were more common for all pts regardless of comorbidity in 1LT compared to 2LT. Median TTNT from 2LT initiation was 14.3 months (95% CI: 9.2, 19.1) for pts with CVD only, 13.7 months (95% CI: 11.4, 17.8) for pts with RD only, 12.3 months (95% CI: 8.4, 16.6) for pts with RD and CVD, and 20.1 months (95% CI: 16.6, 24.4) for pts without CVD or RD. OS at 1 yr and 2 yrs from 2LT initiation were 77.8% and 64.1% for those with CVD only, 77.4% and 58.5% for those with RD only, 72.7% and 51.6% for those with CVD and RD, and 88.2% and 78.4% for pts without CVD or RD (log-rank test, P < 0.05).
Conclusion
Among pts receiving 2LT for RRMM, prevalence of RD and/or CVD increased from 48% to 68% during the MM clinical course. The type of therapy varied by presence of comorbidity for 1LT but to a lesser extent for 2LT. Pts with RD and/or CVD had a shorter TTNT and a lower 1- and 2-yr OS probability relative to those without these comorbidities.References: Castelli, et al. Expert Rev. Anticancer Ther. 2014;14:2:199–215; Dimopoulus, et al. Cancer Treatment Reviews. 2015; 41:827–835; Gupta, et al. Journal of Geriatric Oncology. 2015;6:178-184; Larocca, et al. Blood. 2015;126:19:2179-2185.
Session topic: E-poster
Keyword(s): Comorbidities, Multiple myeloma
{{ help_message }}
{{filter}}


