TREATMENT OF PRE-MYELOMA STATES: A CLINICAL DECISION ANALYSIS
(Abstract release date: 05/19/16)
EHA Library. Liu D. 06/09/16; 132820; E1271

David Liu
Contributions
Contributions
Abstract
Abstract: E1271
Type: Eposter Presentation
Background
Recent studies suggest that treatment of pts with pre-myeloma disease may result in reduced progression to myeloma and improvement in overall survival. However, there is a lack of data to determine which patients would benefit and what type of treatments are optimal. A decision analysis to synthesize available data and quantify the benefits and risks of different treatments in different at-risk populations can help clarify both individual and policy decision-making.
Aims
To quantify the benefit and risks of different treatments in different at-risk populations.To develop a decision framework that informs both individual and policy decision-making for treatment of pre-myeloma states.
Methods
Monte Carlo simulations using a Markov Model were used to simulate the life course of patients diagnosed with pre-myeloma states in the modern era, either treated pre-emptively or monitored per standard of care. The primary outcome was number needed to treat (NNT) to save one life from myeloma, along with life expectancy (LE) and number needed to harm (NNH) given treatment risks. Pre-myeloma risk states modeled included standard risk MGUS (21% 20-yr progression), high risk MGUS (58% 20-yr progression), and smoldering myeloma (78% 20-yr risk of progression). Three interventions were modeled: (1) “high-intensity” treatment (e.g. lenalidomide + dexamethasone) with a conservatively modeled 50% reduction in risk of progression but also an increased risk of developing a secondary hematologic malignancy; (2) “low-intensity” treatment with a 10% reduction in risk of progression; and (3) observation until progression. Rates of progression, increased risk of hematologic malignancy, and death rates from myeloma and secondary malignancies were estimated by literature review. The life course of 500,000 patients for every combination of pre-myeloma state, treatment, and ages ranging from 35 to 75 was simulated. The model was validated against existing cohort data. Probabilistic sensitivity analyses were conducted to generate 95% “confidence intervals” [95% CI] given uncertainty in model parameters.
Results
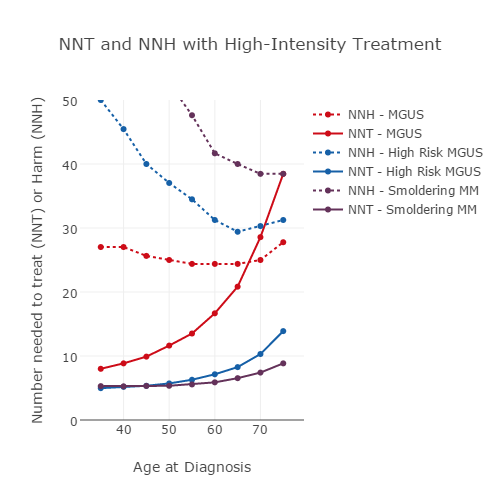
NNT and NNH varied substantially by age, pre-myeloma state, and type of treatment (Figure). For 65 year old patients with high risk MGUS, the high and low-intensity treatments yielded NNTs of 8.3 [6.8-9.8] and 47.6 [33.6-90.9] respectively, an increase in LE of +0.9 [0.3-1.5] and +0.2 [+0.1-0.4] yrs respectively, and an NNH of 29.4 [95% CI 18.2-47.1] for the high-intensity treatment. For 75 yr old patients with MGUS, the high-intensity regimen yielded a lower NNH (27.8 [17.6-58.7]) than NNT (38.5 [27.2-58.1]), suggesting that more patients would be harmed by secondary malignancies than be benefited with treatment, with a non-statistically significant decrease in LE of -0.1 [-0.3-0.1]. In the same cohort, the low-intensity treatment had an NNT of 200 [105.6- 887.5] and no benefit in LE (mean = 0 [0-0.1]). In general, younger patients with higher-risk disease benefitted more from treatment. In 35 yr old patients with smoldering myeloma, the high and low intensity treatments had NNT of 5.3 [4.8-6.5] and 41.7 [30.3-121.9] respectively, with estimated LE increase of +6.5 [5.5-7.7] and +1.0 [0.4-1.3] yrs, respectively, and a NNH for the high-intensity regimen of 71.4 [37.7-154.2].
Conclusion
The benefit/risk ratio of treatment for pre-myeloma patients varies considerably depending on age, risk of myeloma progression, and intensity/risk of treatment. For younger higher-risk pre-myeloma patients, the benefit/risk ratio of high-intensity pre-myeloma intervention is increased, whereas for older patients with lower-risk disease a lower-intensity or no treatment is preferred. Though cost and quality of life under these treatments also need to be considered, our results suggest there are substantial subgroups of patients with pre-myeloma disease who would benefit from treatment. As we develop improved therapies and risk-stratification, using such a quantitative framework will help inform decision-making.
Session topic: E-poster
Keyword(s): MGUS, Myeloma, Prevention, Screening
Type: Eposter Presentation
Background
Recent studies suggest that treatment of pts with pre-myeloma disease may result in reduced progression to myeloma and improvement in overall survival. However, there is a lack of data to determine which patients would benefit and what type of treatments are optimal. A decision analysis to synthesize available data and quantify the benefits and risks of different treatments in different at-risk populations can help clarify both individual and policy decision-making.
Aims
To quantify the benefit and risks of different treatments in different at-risk populations.To develop a decision framework that informs both individual and policy decision-making for treatment of pre-myeloma states.
Methods
Monte Carlo simulations using a Markov Model were used to simulate the life course of patients diagnosed with pre-myeloma states in the modern era, either treated pre-emptively or monitored per standard of care. The primary outcome was number needed to treat (NNT) to save one life from myeloma, along with life expectancy (LE) and number needed to harm (NNH) given treatment risks. Pre-myeloma risk states modeled included standard risk MGUS (21% 20-yr progression), high risk MGUS (58% 20-yr progression), and smoldering myeloma (78% 20-yr risk of progression). Three interventions were modeled: (1) “high-intensity” treatment (e.g. lenalidomide + dexamethasone) with a conservatively modeled 50% reduction in risk of progression but also an increased risk of developing a secondary hematologic malignancy; (2) “low-intensity” treatment with a 10% reduction in risk of progression; and (3) observation until progression. Rates of progression, increased risk of hematologic malignancy, and death rates from myeloma and secondary malignancies were estimated by literature review. The life course of 500,000 patients for every combination of pre-myeloma state, treatment, and ages ranging from 35 to 75 was simulated. The model was validated against existing cohort data. Probabilistic sensitivity analyses were conducted to generate 95% “confidence intervals” [95% CI] given uncertainty in model parameters.
Results
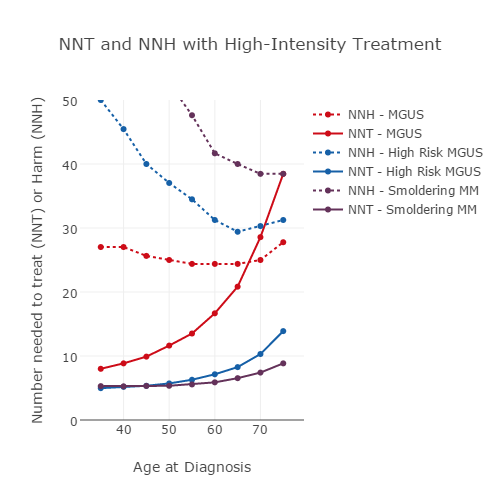
NNT and NNH varied substantially by age, pre-myeloma state, and type of treatment (Figure). For 65 year old patients with high risk MGUS, the high and low-intensity treatments yielded NNTs of 8.3 [6.8-9.8] and 47.6 [33.6-90.9] respectively, an increase in LE of +0.9 [0.3-1.5] and +0.2 [+0.1-0.4] yrs respectively, and an NNH of 29.4 [95% CI 18.2-47.1] for the high-intensity treatment. For 75 yr old patients with MGUS, the high-intensity regimen yielded a lower NNH (27.8 [17.6-58.7]) than NNT (38.5 [27.2-58.1]), suggesting that more patients would be harmed by secondary malignancies than be benefited with treatment, with a non-statistically significant decrease in LE of -0.1 [-0.3-0.1]. In the same cohort, the low-intensity treatment had an NNT of 200 [105.6- 887.5] and no benefit in LE (mean = 0 [0-0.1]). In general, younger patients with higher-risk disease benefitted more from treatment. In 35 yr old patients with smoldering myeloma, the high and low intensity treatments had NNT of 5.3 [4.8-6.5] and 41.7 [30.3-121.9] respectively, with estimated LE increase of +6.5 [5.5-7.7] and +1.0 [0.4-1.3] yrs, respectively, and a NNH for the high-intensity regimen of 71.4 [37.7-154.2].
Conclusion
The benefit/risk ratio of treatment for pre-myeloma patients varies considerably depending on age, risk of myeloma progression, and intensity/risk of treatment. For younger higher-risk pre-myeloma patients, the benefit/risk ratio of high-intensity pre-myeloma intervention is increased, whereas for older patients with lower-risk disease a lower-intensity or no treatment is preferred. Though cost and quality of life under these treatments also need to be considered, our results suggest there are substantial subgroups of patients with pre-myeloma disease who would benefit from treatment. As we develop improved therapies and risk-stratification, using such a quantitative framework will help inform decision-making.
Session topic: E-poster
Keyword(s): MGUS, Myeloma, Prevention, Screening
Abstract: E1271
Type: Eposter Presentation
Background
Recent studies suggest that treatment of pts with pre-myeloma disease may result in reduced progression to myeloma and improvement in overall survival. However, there is a lack of data to determine which patients would benefit and what type of treatments are optimal. A decision analysis to synthesize available data and quantify the benefits and risks of different treatments in different at-risk populations can help clarify both individual and policy decision-making.
Aims
To quantify the benefit and risks of different treatments in different at-risk populations.To develop a decision framework that informs both individual and policy decision-making for treatment of pre-myeloma states.
Methods
Monte Carlo simulations using a Markov Model were used to simulate the life course of patients diagnosed with pre-myeloma states in the modern era, either treated pre-emptively or monitored per standard of care. The primary outcome was number needed to treat (NNT) to save one life from myeloma, along with life expectancy (LE) and number needed to harm (NNH) given treatment risks. Pre-myeloma risk states modeled included standard risk MGUS (21% 20-yr progression), high risk MGUS (58% 20-yr progression), and smoldering myeloma (78% 20-yr risk of progression). Three interventions were modeled: (1) “high-intensity” treatment (e.g. lenalidomide + dexamethasone) with a conservatively modeled 50% reduction in risk of progression but also an increased risk of developing a secondary hematologic malignancy; (2) “low-intensity” treatment with a 10% reduction in risk of progression; and (3) observation until progression. Rates of progression, increased risk of hematologic malignancy, and death rates from myeloma and secondary malignancies were estimated by literature review. The life course of 500,000 patients for every combination of pre-myeloma state, treatment, and ages ranging from 35 to 75 was simulated. The model was validated against existing cohort data. Probabilistic sensitivity analyses were conducted to generate 95% “confidence intervals” [95% CI] given uncertainty in model parameters.
Results
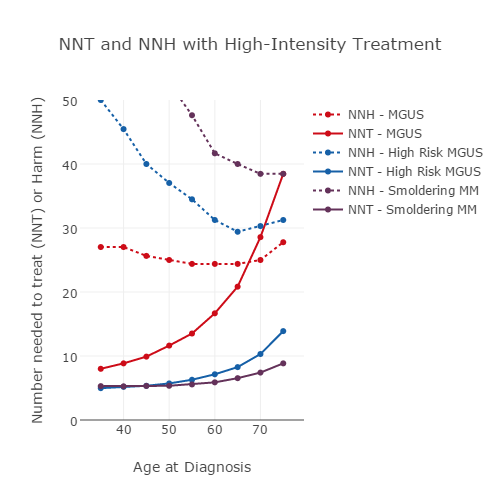
NNT and NNH varied substantially by age, pre-myeloma state, and type of treatment (Figure). For 65 year old patients with high risk MGUS, the high and low-intensity treatments yielded NNTs of 8.3 [6.8-9.8] and 47.6 [33.6-90.9] respectively, an increase in LE of +0.9 [0.3-1.5] and +0.2 [+0.1-0.4] yrs respectively, and an NNH of 29.4 [95% CI 18.2-47.1] for the high-intensity treatment. For 75 yr old patients with MGUS, the high-intensity regimen yielded a lower NNH (27.8 [17.6-58.7]) than NNT (38.5 [27.2-58.1]), suggesting that more patients would be harmed by secondary malignancies than be benefited with treatment, with a non-statistically significant decrease in LE of -0.1 [-0.3-0.1]. In the same cohort, the low-intensity treatment had an NNT of 200 [105.6- 887.5] and no benefit in LE (mean = 0 [0-0.1]). In general, younger patients with higher-risk disease benefitted more from treatment. In 35 yr old patients with smoldering myeloma, the high and low intensity treatments had NNT of 5.3 [4.8-6.5] and 41.7 [30.3-121.9] respectively, with estimated LE increase of +6.5 [5.5-7.7] and +1.0 [0.4-1.3] yrs, respectively, and a NNH for the high-intensity regimen of 71.4 [37.7-154.2].
Conclusion
The benefit/risk ratio of treatment for pre-myeloma patients varies considerably depending on age, risk of myeloma progression, and intensity/risk of treatment. For younger higher-risk pre-myeloma patients, the benefit/risk ratio of high-intensity pre-myeloma intervention is increased, whereas for older patients with lower-risk disease a lower-intensity or no treatment is preferred. Though cost and quality of life under these treatments also need to be considered, our results suggest there are substantial subgroups of patients with pre-myeloma disease who would benefit from treatment. As we develop improved therapies and risk-stratification, using such a quantitative framework will help inform decision-making.
Session topic: E-poster
Keyword(s): MGUS, Myeloma, Prevention, Screening
Type: Eposter Presentation
Background
Recent studies suggest that treatment of pts with pre-myeloma disease may result in reduced progression to myeloma and improvement in overall survival. However, there is a lack of data to determine which patients would benefit and what type of treatments are optimal. A decision analysis to synthesize available data and quantify the benefits and risks of different treatments in different at-risk populations can help clarify both individual and policy decision-making.
Aims
To quantify the benefit and risks of different treatments in different at-risk populations.To develop a decision framework that informs both individual and policy decision-making for treatment of pre-myeloma states.
Methods
Monte Carlo simulations using a Markov Model were used to simulate the life course of patients diagnosed with pre-myeloma states in the modern era, either treated pre-emptively or monitored per standard of care. The primary outcome was number needed to treat (NNT) to save one life from myeloma, along with life expectancy (LE) and number needed to harm (NNH) given treatment risks. Pre-myeloma risk states modeled included standard risk MGUS (21% 20-yr progression), high risk MGUS (58% 20-yr progression), and smoldering myeloma (78% 20-yr risk of progression). Three interventions were modeled: (1) “high-intensity” treatment (e.g. lenalidomide + dexamethasone) with a conservatively modeled 50% reduction in risk of progression but also an increased risk of developing a secondary hematologic malignancy; (2) “low-intensity” treatment with a 10% reduction in risk of progression; and (3) observation until progression. Rates of progression, increased risk of hematologic malignancy, and death rates from myeloma and secondary malignancies were estimated by literature review. The life course of 500,000 patients for every combination of pre-myeloma state, treatment, and ages ranging from 35 to 75 was simulated. The model was validated against existing cohort data. Probabilistic sensitivity analyses were conducted to generate 95% “confidence intervals” [95% CI] given uncertainty in model parameters.
Results
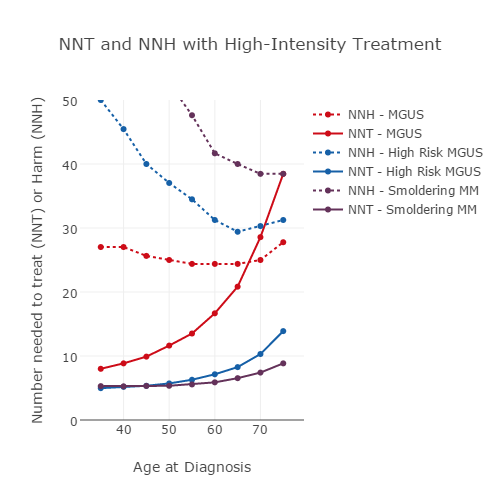
NNT and NNH varied substantially by age, pre-myeloma state, and type of treatment (Figure). For 65 year old patients with high risk MGUS, the high and low-intensity treatments yielded NNTs of 8.3 [6.8-9.8] and 47.6 [33.6-90.9] respectively, an increase in LE of +0.9 [0.3-1.5] and +0.2 [+0.1-0.4] yrs respectively, and an NNH of 29.4 [95% CI 18.2-47.1] for the high-intensity treatment. For 75 yr old patients with MGUS, the high-intensity regimen yielded a lower NNH (27.8 [17.6-58.7]) than NNT (38.5 [27.2-58.1]), suggesting that more patients would be harmed by secondary malignancies than be benefited with treatment, with a non-statistically significant decrease in LE of -0.1 [-0.3-0.1]. In the same cohort, the low-intensity treatment had an NNT of 200 [105.6- 887.5] and no benefit in LE (mean = 0 [0-0.1]). In general, younger patients with higher-risk disease benefitted more from treatment. In 35 yr old patients with smoldering myeloma, the high and low intensity treatments had NNT of 5.3 [4.8-6.5] and 41.7 [30.3-121.9] respectively, with estimated LE increase of +6.5 [5.5-7.7] and +1.0 [0.4-1.3] yrs, respectively, and a NNH for the high-intensity regimen of 71.4 [37.7-154.2].
Conclusion
The benefit/risk ratio of treatment for pre-myeloma patients varies considerably depending on age, risk of myeloma progression, and intensity/risk of treatment. For younger higher-risk pre-myeloma patients, the benefit/risk ratio of high-intensity pre-myeloma intervention is increased, whereas for older patients with lower-risk disease a lower-intensity or no treatment is preferred. Though cost and quality of life under these treatments also need to be considered, our results suggest there are substantial subgroups of patients with pre-myeloma disease who would benefit from treatment. As we develop improved therapies and risk-stratification, using such a quantitative framework will help inform decision-making.
Session topic: E-poster
Keyword(s): MGUS, Myeloma, Prevention, Screening
{{ help_message }}
{{filter}}


