REPORT ON OUTCOME OF HYPOMETHYLATING THERAPY WITH ANALYSIS ON PROGNOSTIC VALUE OF REVISED-INTERNATIONAL PROGNOSTIC SCORING SYSTEM IN PATIENTS WITH MYELODYSPLASTIC SYNDROMES OF LOWER-RISK BASED ON IPSS
(Abstract release date: 05/19/16)
EHA Library. Lee Y. 06/09/16; 132780; E1231

Yoo Jin Lee
Contributions
Contributions
Abstract
Abstract: E1231
Type: Eposter Presentation
Background
The outcome of patients with lower risk myelodysplastic syndromes (LR-MDS) by International Prognostic Scoring System (IPSS) is very various and sometimes poorer than expected.
Aims
We retrospectively evaluated the prognostic value of revised-International Prognostic Scoring System (IPSS-R) in accordance with Hypomethylating therapy (HMT) response for precise prognostication.
Methods
The treatment outcome of 236 patients with IPSS LR-MDS who received HMT in the Korean MDS Working Party was retrospectively evaluated. The patients were reclassified to very low/low (VL/L), intermediate (INT), and high (H) risk groups by IPSS-R.
Results
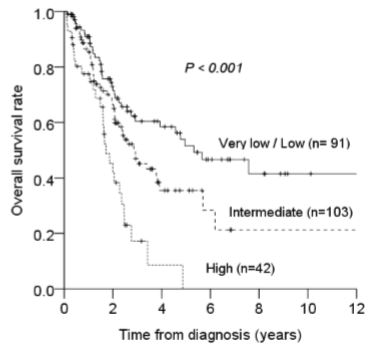
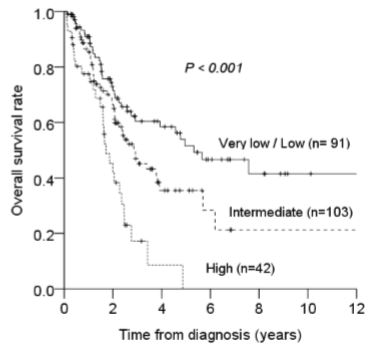
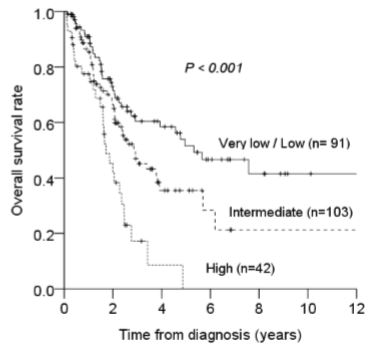
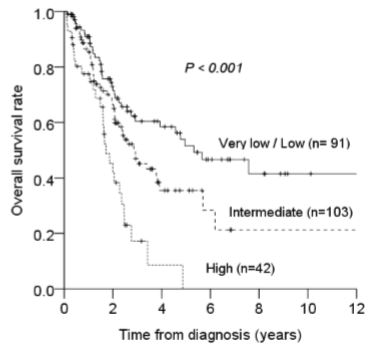
According to the HMT response, 3 year overall survival (OS) did not differ between response group (43.4 ± 0.8%) and stable group (Fig 1. 53.6 ± 0.6%, p=0. 672). Although 25 patients (38.4%) out of 65 responders had a benefit to continued HMT with a median 14 cycles, H risk group was only 2 patients. Among 27 patients (41.5%) progressed to secondary failure, H risk group was most common. Indeed, 42 patients (20.8%) out of 236 patients with LR-MDS had changed to H risk group based on IPSS-R. Median OS was 63.8 months (range, 32.6-95 months) in VL/L, 35 months (range, 24.2-45.9 months) in INT, and 22.3 months (range, 16.6-27.9 months) in H risk group, respectively (Fig-2. p<0.001). Transformation to AML was 8 patients (8.8%) in VL/L, 12 (12.7%) in INT, and 10 (23.8%) in H risk group (p=0.049). On multivariate analysis, the following factors were associated with survival: age ≥ 65 (HR= 1.731, p=0.023), ECOG ≥ 2 (HR= 4.997, p<0.001), H risk group by IPSS-R (HR=3.054, 95% CI=1.714-5.441, p<0.001), blast ≥ 5% (HR= 2.070, p=0.035), P/VP cytogenetic risk by IPSS-R (HR= 4.501, p=0.006) and transformation to AML (HR=2.208, p=0.007).
Conclusion
If patients with LR-MDS are included in the H risk by IPSS-R, they should be considered early allo-HCT regardless of current benefits from HMT. Prospective study will be needed to establish the therapeutic strategies in MDS patients with Low-risk by IPSS including optimal timing of allogeneic transplantation and the continuing HMT.
Session topic: E-poster
Keyword(s): Hypomethylation, Myelodysplasia
Type: Eposter Presentation
Background
The outcome of patients with lower risk myelodysplastic syndromes (LR-MDS) by International Prognostic Scoring System (IPSS) is very various and sometimes poorer than expected.
Aims
We retrospectively evaluated the prognostic value of revised-International Prognostic Scoring System (IPSS-R) in accordance with Hypomethylating therapy (HMT) response for precise prognostication.
Methods
The treatment outcome of 236 patients with IPSS LR-MDS who received HMT in the Korean MDS Working Party was retrospectively evaluated. The patients were reclassified to very low/low (VL/L), intermediate (INT), and high (H) risk groups by IPSS-R.
Results
According to the HMT response, 3 year overall survival (OS) did not differ between response group (43.4 ± 0.8%) and stable group (Fig 1. 53.6 ± 0.6%, p=0. 672). Although 25 patients (38.4%) out of 65 responders had a benefit to continued HMT with a median 14 cycles, H risk group was only 2 patients. Among 27 patients (41.5%) progressed to secondary failure, H risk group was most common. Indeed, 42 patients (20.8%) out of 236 patients with LR-MDS had changed to H risk group based on IPSS-R. Median OS was 63.8 months (range, 32.6-95 months) in VL/L, 35 months (range, 24.2-45.9 months) in INT, and 22.3 months (range, 16.6-27.9 months) in H risk group, respectively (Fig-2. p<0.001). Transformation to AML was 8 patients (8.8%) in VL/L, 12 (12.7%) in INT, and 10 (23.8%) in H risk group (p=0.049). On multivariate analysis, the following factors were associated with survival: age ≥ 65 (HR= 1.731, p=0.023), ECOG ≥ 2 (HR= 4.997, p<0.001), H risk group by IPSS-R (HR=3.054, 95% CI=1.714-5.441, p<0.001), blast ≥ 5% (HR= 2.070, p=0.035), P/VP cytogenetic risk by IPSS-R (HR= 4.501, p=0.006) and transformation to AML (HR=2.208, p=0.007).
Conclusion
If patients with LR-MDS are included in the H risk by IPSS-R, they should be considered early allo-HCT regardless of current benefits from HMT. Prospective study will be needed to establish the therapeutic strategies in MDS patients with Low-risk by IPSS including optimal timing of allogeneic transplantation and the continuing HMT.
Session topic: E-poster
Keyword(s): Hypomethylation, Myelodysplasia
Abstract: E1231
Type: Eposter Presentation
Background
The outcome of patients with lower risk myelodysplastic syndromes (LR-MDS) by International Prognostic Scoring System (IPSS) is very various and sometimes poorer than expected.
Aims
We retrospectively evaluated the prognostic value of revised-International Prognostic Scoring System (IPSS-R) in accordance with Hypomethylating therapy (HMT) response for precise prognostication.
Methods
The treatment outcome of 236 patients with IPSS LR-MDS who received HMT in the Korean MDS Working Party was retrospectively evaluated. The patients were reclassified to very low/low (VL/L), intermediate (INT), and high (H) risk groups by IPSS-R.
Results
According to the HMT response, 3 year overall survival (OS) did not differ between response group (43.4 ± 0.8%) and stable group (Fig 1. 53.6 ± 0.6%, p=0. 672). Although 25 patients (38.4%) out of 65 responders had a benefit to continued HMT with a median 14 cycles, H risk group was only 2 patients. Among 27 patients (41.5%) progressed to secondary failure, H risk group was most common. Indeed, 42 patients (20.8%) out of 236 patients with LR-MDS had changed to H risk group based on IPSS-R. Median OS was 63.8 months (range, 32.6-95 months) in VL/L, 35 months (range, 24.2-45.9 months) in INT, and 22.3 months (range, 16.6-27.9 months) in H risk group, respectively (Fig-2. p<0.001). Transformation to AML was 8 patients (8.8%) in VL/L, 12 (12.7%) in INT, and 10 (23.8%) in H risk group (p=0.049). On multivariate analysis, the following factors were associated with survival: age ≥ 65 (HR= 1.731, p=0.023), ECOG ≥ 2 (HR= 4.997, p<0.001), H risk group by IPSS-R (HR=3.054, 95% CI=1.714-5.441, p<0.001), blast ≥ 5% (HR= 2.070, p=0.035), P/VP cytogenetic risk by IPSS-R (HR= 4.501, p=0.006) and transformation to AML (HR=2.208, p=0.007).
Conclusion
If patients with LR-MDS are included in the H risk by IPSS-R, they should be considered early allo-HCT regardless of current benefits from HMT. Prospective study will be needed to establish the therapeutic strategies in MDS patients with Low-risk by IPSS including optimal timing of allogeneic transplantation and the continuing HMT.
Session topic: E-poster
Keyword(s): Hypomethylation, Myelodysplasia
Type: Eposter Presentation
Background
The outcome of patients with lower risk myelodysplastic syndromes (LR-MDS) by International Prognostic Scoring System (IPSS) is very various and sometimes poorer than expected.
Aims
We retrospectively evaluated the prognostic value of revised-International Prognostic Scoring System (IPSS-R) in accordance with Hypomethylating therapy (HMT) response for precise prognostication.
Methods
The treatment outcome of 236 patients with IPSS LR-MDS who received HMT in the Korean MDS Working Party was retrospectively evaluated. The patients were reclassified to very low/low (VL/L), intermediate (INT), and high (H) risk groups by IPSS-R.
Results
According to the HMT response, 3 year overall survival (OS) did not differ between response group (43.4 ± 0.8%) and stable group (Fig 1. 53.6 ± 0.6%, p=0. 672). Although 25 patients (38.4%) out of 65 responders had a benefit to continued HMT with a median 14 cycles, H risk group was only 2 patients. Among 27 patients (41.5%) progressed to secondary failure, H risk group was most common. Indeed, 42 patients (20.8%) out of 236 patients with LR-MDS had changed to H risk group based on IPSS-R. Median OS was 63.8 months (range, 32.6-95 months) in VL/L, 35 months (range, 24.2-45.9 months) in INT, and 22.3 months (range, 16.6-27.9 months) in H risk group, respectively (Fig-2. p<0.001). Transformation to AML was 8 patients (8.8%) in VL/L, 12 (12.7%) in INT, and 10 (23.8%) in H risk group (p=0.049). On multivariate analysis, the following factors were associated with survival: age ≥ 65 (HR= 1.731, p=0.023), ECOG ≥ 2 (HR= 4.997, p<0.001), H risk group by IPSS-R (HR=3.054, 95% CI=1.714-5.441, p<0.001), blast ≥ 5% (HR= 2.070, p=0.035), P/VP cytogenetic risk by IPSS-R (HR= 4.501, p=0.006) and transformation to AML (HR=2.208, p=0.007).
Conclusion
If patients with LR-MDS are included in the H risk by IPSS-R, they should be considered early allo-HCT regardless of current benefits from HMT. Prospective study will be needed to establish the therapeutic strategies in MDS patients with Low-risk by IPSS including optimal timing of allogeneic transplantation and the continuing HMT.
Session topic: E-poster
Keyword(s): Hypomethylation, Myelodysplasia
{{ help_message }}
{{filter}}


