DISCONTINUATION OF HYPOMETHYLATING AGENT, DOES IT BRING REDUCED SURVIVAL IN PATIENTS WITH NEWLY DIAGNOSED MYELODYSPLASTIC SYNDROME ?
(Abstract release date: 05/19/16)
EHA Library. Lee H. 06/09/16; 132772; E1223
Disclosure(s): We have no conflicts of interest to disclosure

Prof. Dr. Ho Sup Lee
Contributions
Contributions
Abstract
Abstract: E1223
Type: Eposter Presentation
Background
The myelodysplastic syndromes (MDSs) are a heterogeneous collection of clonal hematopoietic malignancies that primarily affect the elderly and are characterized by bone marrow failure, dysplasia. In previous study, prolonged treatment duration could have contributed to survival benefit. Although treatment with HMA undoubtedly prolongs survival in patients who have poor prognosis, there are still a significant proportion of patients with MDS who do not respond to therapy with HMA and patients who lose response or progress on therapy. However, in clinical practice, it is difficult to continue treatment of HMA because of problems such as toxicities, poor economics, comorbidities and compliance etc. For those reasons, discontinuation of HMA before disease progression often happen in clinical setting.
Aims
So there are some questions about survival in MDS patients treated with HMA in real clinical practice. Are there any differences of survival in patients with MDS received HMA between treatment failure and discontinuation of HMA ?. And what factors will be helpful to predict survival in both patients group ?.
Methods
The medical records of 246 patients were collected retrospectively from fourteen university hospitals in South Korea between January 2001 and October 2013. All included patients had been newly diagnosed to MDS and they were treated with HMA as front line therapy and they were treated continuously at least 4 cycles. Patients divided two groups into treatment failure group who discontinued HMA treatment due to disease progression and discontinuation of HMA group who stopped HMA treatment because of other cause without disease progression. The treatment free survival (TFS) was defined duration from the end date of HMA therapy to the date of disease progression, relapse, or death from any causes.
Results
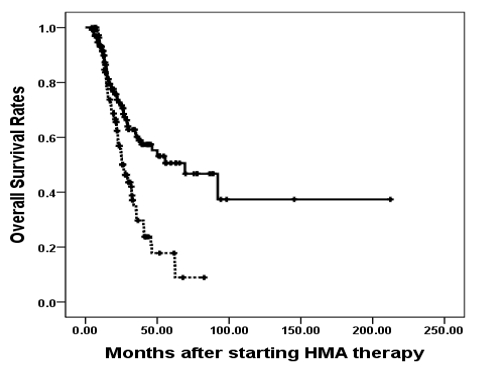
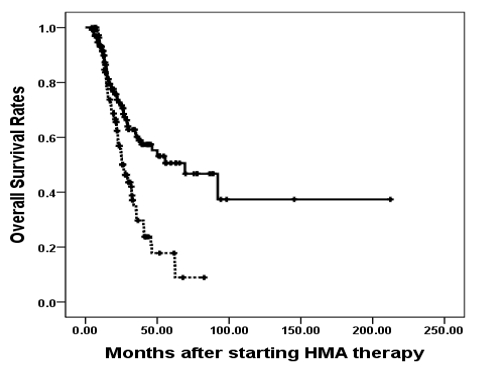
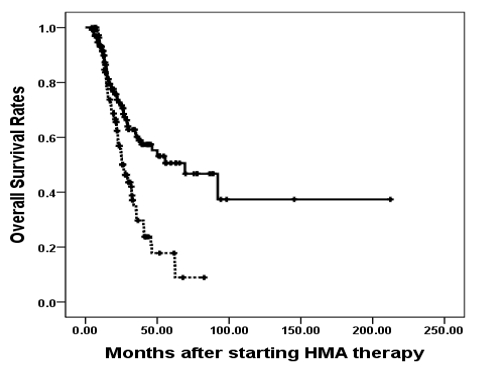
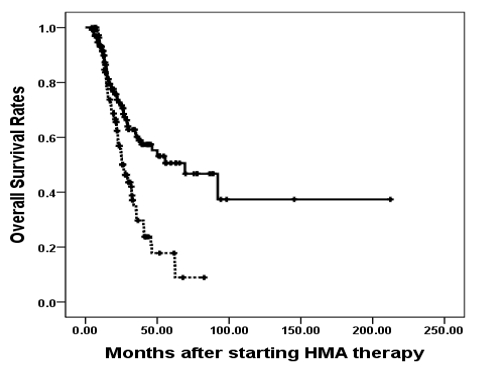
The median age of the patients was 68 years. (range 24-92 years) and the male to female ratio was 1.9:1.0. The percentage of lower than 5% of bone marrow myeloblast was 37.9% in treatment failure group, 62.1% in discontinuation group (p=0.015). Patients who found lower risk IPSS or WPSS were documented in discontinuation group more than those in treatment failure group (p=0.050 or 0.005). The median TFS was 4.7 months (range 2.4-7.0) and the median OS was 34.8 months (range 28.4 – 41.2). In multivariate analysis, treatment failure of HMA is independent risk factor for shorter TFS (RR:5.996, 95% C.I. 3.684-9.757, p<0.001). Age of more than 65 years, bone marrow myeloblast of more than 5%, poor cytogenetics, platelet counts of less than 50 x 103/uL, higher risk of WPSS and IPSS-R, median number of HMA cycles of less than 7 cycles and treatment failure of HMA were independent risk factors for shorter OS. Especially, The 3-year TFS and OS were 0.0% vs 40.7%, (p<0.001) and 29.7% vs 60.2% (p<0.001) in treatment failure group vs discontinuation of HMA group, respectively. However, in univariate and multivariate analysis, higher risk of WPSS was independent risk factor for shorter TFS and higher risk of WPSS and median number of HMA of less than 7 cycles were independent risk factors for shorter OS in only discontinuation of HMA group.
Conclusion
Patients who discontinued HMA without disease progression showed prolonged survival than those who failed HMA treatment in real clinical practice. Especially, lower risk of WPSS and more number of performed cycles of HMA may be helpful to predict TFS and OS in patients who discontinued HMA because of other causes such as toxicities, economics or compliance etc.
Session topic: E-poster
Keyword(s): Hypomethylation, Myelodysplasia, Survival prediction
Type: Eposter Presentation
Background
The myelodysplastic syndromes (MDSs) are a heterogeneous collection of clonal hematopoietic malignancies that primarily affect the elderly and are characterized by bone marrow failure, dysplasia. In previous study, prolonged treatment duration could have contributed to survival benefit. Although treatment with HMA undoubtedly prolongs survival in patients who have poor prognosis, there are still a significant proportion of patients with MDS who do not respond to therapy with HMA and patients who lose response or progress on therapy. However, in clinical practice, it is difficult to continue treatment of HMA because of problems such as toxicities, poor economics, comorbidities and compliance etc. For those reasons, discontinuation of HMA before disease progression often happen in clinical setting.
Aims
So there are some questions about survival in MDS patients treated with HMA in real clinical practice. Are there any differences of survival in patients with MDS received HMA between treatment failure and discontinuation of HMA ?. And what factors will be helpful to predict survival in both patients group ?.
Methods
The medical records of 246 patients were collected retrospectively from fourteen university hospitals in South Korea between January 2001 and October 2013. All included patients had been newly diagnosed to MDS and they were treated with HMA as front line therapy and they were treated continuously at least 4 cycles. Patients divided two groups into treatment failure group who discontinued HMA treatment due to disease progression and discontinuation of HMA group who stopped HMA treatment because of other cause without disease progression. The treatment free survival (TFS) was defined duration from the end date of HMA therapy to the date of disease progression, relapse, or death from any causes.
Results
The median age of the patients was 68 years. (range 24-92 years) and the male to female ratio was 1.9:1.0. The percentage of lower than 5% of bone marrow myeloblast was 37.9% in treatment failure group, 62.1% in discontinuation group (p=0.015). Patients who found lower risk IPSS or WPSS were documented in discontinuation group more than those in treatment failure group (p=0.050 or 0.005). The median TFS was 4.7 months (range 2.4-7.0) and the median OS was 34.8 months (range 28.4 – 41.2). In multivariate analysis, treatment failure of HMA is independent risk factor for shorter TFS (RR:5.996, 95% C.I. 3.684-9.757, p<0.001). Age of more than 65 years, bone marrow myeloblast of more than 5%, poor cytogenetics, platelet counts of less than 50 x 103/uL, higher risk of WPSS and IPSS-R, median number of HMA cycles of less than 7 cycles and treatment failure of HMA were independent risk factors for shorter OS. Especially, The 3-year TFS and OS were 0.0% vs 40.7%, (p<0.001) and 29.7% vs 60.2% (p<0.001) in treatment failure group vs discontinuation of HMA group, respectively. However, in univariate and multivariate analysis, higher risk of WPSS was independent risk factor for shorter TFS and higher risk of WPSS and median number of HMA of less than 7 cycles were independent risk factors for shorter OS in only discontinuation of HMA group.
Conclusion
Patients who discontinued HMA without disease progression showed prolonged survival than those who failed HMA treatment in real clinical practice. Especially, lower risk of WPSS and more number of performed cycles of HMA may be helpful to predict TFS and OS in patients who discontinued HMA because of other causes such as toxicities, economics or compliance etc.
Session topic: E-poster
Keyword(s): Hypomethylation, Myelodysplasia, Survival prediction
Abstract: E1223
Type: Eposter Presentation
Background
The myelodysplastic syndromes (MDSs) are a heterogeneous collection of clonal hematopoietic malignancies that primarily affect the elderly and are characterized by bone marrow failure, dysplasia. In previous study, prolonged treatment duration could have contributed to survival benefit. Although treatment with HMA undoubtedly prolongs survival in patients who have poor prognosis, there are still a significant proportion of patients with MDS who do not respond to therapy with HMA and patients who lose response or progress on therapy. However, in clinical practice, it is difficult to continue treatment of HMA because of problems such as toxicities, poor economics, comorbidities and compliance etc. For those reasons, discontinuation of HMA before disease progression often happen in clinical setting.
Aims
So there are some questions about survival in MDS patients treated with HMA in real clinical practice. Are there any differences of survival in patients with MDS received HMA between treatment failure and discontinuation of HMA ?. And what factors will be helpful to predict survival in both patients group ?.
Methods
The medical records of 246 patients were collected retrospectively from fourteen university hospitals in South Korea between January 2001 and October 2013. All included patients had been newly diagnosed to MDS and they were treated with HMA as front line therapy and they were treated continuously at least 4 cycles. Patients divided two groups into treatment failure group who discontinued HMA treatment due to disease progression and discontinuation of HMA group who stopped HMA treatment because of other cause without disease progression. The treatment free survival (TFS) was defined duration from the end date of HMA therapy to the date of disease progression, relapse, or death from any causes.
Results
The median age of the patients was 68 years. (range 24-92 years) and the male to female ratio was 1.9:1.0. The percentage of lower than 5% of bone marrow myeloblast was 37.9% in treatment failure group, 62.1% in discontinuation group (p=0.015). Patients who found lower risk IPSS or WPSS were documented in discontinuation group more than those in treatment failure group (p=0.050 or 0.005). The median TFS was 4.7 months (range 2.4-7.0) and the median OS was 34.8 months (range 28.4 – 41.2). In multivariate analysis, treatment failure of HMA is independent risk factor for shorter TFS (RR:5.996, 95% C.I. 3.684-9.757, p<0.001). Age of more than 65 years, bone marrow myeloblast of more than 5%, poor cytogenetics, platelet counts of less than 50 x 103/uL, higher risk of WPSS and IPSS-R, median number of HMA cycles of less than 7 cycles and treatment failure of HMA were independent risk factors for shorter OS. Especially, The 3-year TFS and OS were 0.0% vs 40.7%, (p<0.001) and 29.7% vs 60.2% (p<0.001) in treatment failure group vs discontinuation of HMA group, respectively. However, in univariate and multivariate analysis, higher risk of WPSS was independent risk factor for shorter TFS and higher risk of WPSS and median number of HMA of less than 7 cycles were independent risk factors for shorter OS in only discontinuation of HMA group.
Conclusion
Patients who discontinued HMA without disease progression showed prolonged survival than those who failed HMA treatment in real clinical practice. Especially, lower risk of WPSS and more number of performed cycles of HMA may be helpful to predict TFS and OS in patients who discontinued HMA because of other causes such as toxicities, economics or compliance etc.
Session topic: E-poster
Keyword(s): Hypomethylation, Myelodysplasia, Survival prediction
Type: Eposter Presentation
Background
The myelodysplastic syndromes (MDSs) are a heterogeneous collection of clonal hematopoietic malignancies that primarily affect the elderly and are characterized by bone marrow failure, dysplasia. In previous study, prolonged treatment duration could have contributed to survival benefit. Although treatment with HMA undoubtedly prolongs survival in patients who have poor prognosis, there are still a significant proportion of patients with MDS who do not respond to therapy with HMA and patients who lose response or progress on therapy. However, in clinical practice, it is difficult to continue treatment of HMA because of problems such as toxicities, poor economics, comorbidities and compliance etc. For those reasons, discontinuation of HMA before disease progression often happen in clinical setting.
Aims
So there are some questions about survival in MDS patients treated with HMA in real clinical practice. Are there any differences of survival in patients with MDS received HMA between treatment failure and discontinuation of HMA ?. And what factors will be helpful to predict survival in both patients group ?.
Methods
The medical records of 246 patients were collected retrospectively from fourteen university hospitals in South Korea between January 2001 and October 2013. All included patients had been newly diagnosed to MDS and they were treated with HMA as front line therapy and they were treated continuously at least 4 cycles. Patients divided two groups into treatment failure group who discontinued HMA treatment due to disease progression and discontinuation of HMA group who stopped HMA treatment because of other cause without disease progression. The treatment free survival (TFS) was defined duration from the end date of HMA therapy to the date of disease progression, relapse, or death from any causes.
Results
The median age of the patients was 68 years. (range 24-92 years) and the male to female ratio was 1.9:1.0. The percentage of lower than 5% of bone marrow myeloblast was 37.9% in treatment failure group, 62.1% in discontinuation group (p=0.015). Patients who found lower risk IPSS or WPSS were documented in discontinuation group more than those in treatment failure group (p=0.050 or 0.005). The median TFS was 4.7 months (range 2.4-7.0) and the median OS was 34.8 months (range 28.4 – 41.2). In multivariate analysis, treatment failure of HMA is independent risk factor for shorter TFS (RR:5.996, 95% C.I. 3.684-9.757, p<0.001). Age of more than 65 years, bone marrow myeloblast of more than 5%, poor cytogenetics, platelet counts of less than 50 x 103/uL, higher risk of WPSS and IPSS-R, median number of HMA cycles of less than 7 cycles and treatment failure of HMA were independent risk factors for shorter OS. Especially, The 3-year TFS and OS were 0.0% vs 40.7%, (p<0.001) and 29.7% vs 60.2% (p<0.001) in treatment failure group vs discontinuation of HMA group, respectively. However, in univariate and multivariate analysis, higher risk of WPSS was independent risk factor for shorter TFS and higher risk of WPSS and median number of HMA of less than 7 cycles were independent risk factors for shorter OS in only discontinuation of HMA group.
Conclusion
Patients who discontinued HMA without disease progression showed prolonged survival than those who failed HMA treatment in real clinical practice. Especially, lower risk of WPSS and more number of performed cycles of HMA may be helpful to predict TFS and OS in patients who discontinued HMA because of other causes such as toxicities, economics or compliance etc.
Session topic: E-poster
Keyword(s): Hypomethylation, Myelodysplasia, Survival prediction
{{ help_message }}
{{filter}}


