ANALYSIS OF P53 EXPRESSION BY IMMUNOHISTOCHEMISTRY AS AN ADDITIONAL PROGNOSTIC TOOL IN PATIENTS WITH MYELODYSPLASTIC SYNDROMES
(Abstract release date: 05/19/16)
EHA Library. maung s. 06/09/16; 132768; E1219
Disclosure(s): I have received speaker honorarium from Celgene Ltd.

Dr. su maung
Contributions
Contributions
Abstract
Abstract: E1219
Type: Eposter Presentation
Background
Somatic mutations in TP53 have been shown to be associated with aggressive disease, resistance to therapy and poor survival in many cancers including haematological neoplasms. The incidence of TP53 mutations in Myelodysplastic Syndromes (MDS) is low (5-15%) compared to other malignancies but may be associated with adverse outcomes. Consistent correlations of up to 96% between TP53 mutation by conventional sequencing and demonstration of p53 expression by immunohistochemistry (IHC) has been demonstrated by prior studies.
Aims
We assessed p53 expression by IHC on marrow trephine samples of 246 MDS patients to correlate the p53 expression with their clinical characteristics and outcomes.
Methods
IHC for p53 expression on marrow trephines of 246 MDS patients diagnosed between 2003 and 2014 in a single centre were analysed using DO-7 monoclonal antibody. Clinical information and overall survival including transformation to acute myeloid leukaemia (AML) were obtained from clinical notes and patient information systems. P53 expression was determined by assessing 1000 haematopoietic cells under high magnification and scored using a Modified Quick Scoring System.
Results
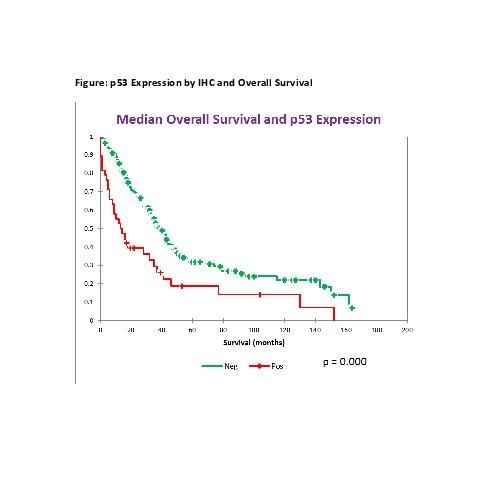
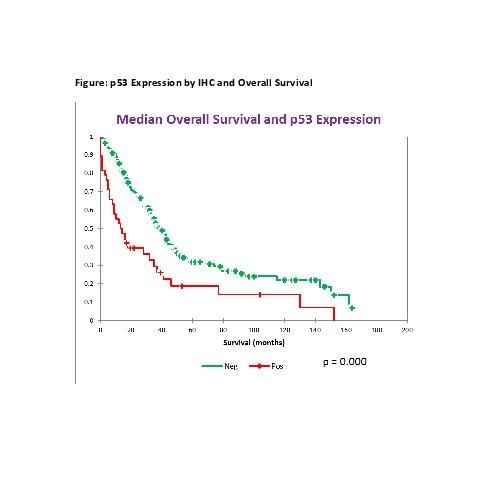
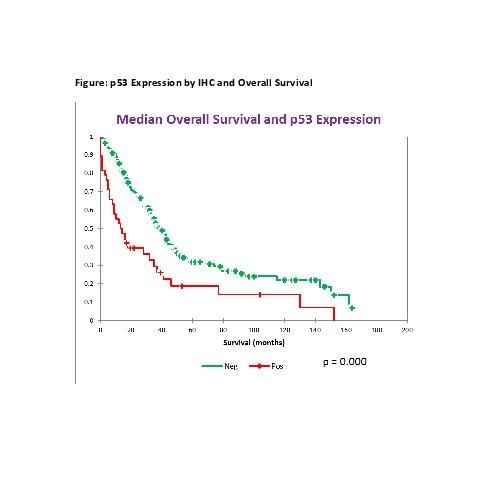
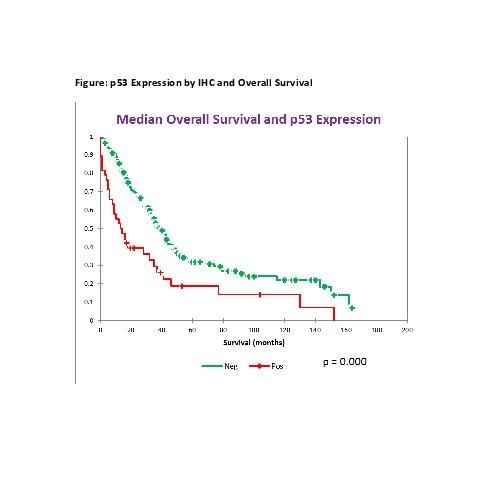
Thirty nine patients (16%) were positive for p53 expression and 207 patients (84%) were negative. P53 positive patients showed greater degree of peripheral cytopenias and higher marrow blasts. None of the patients with WHO subgroups of RARS, RCMD-RS or MDS 5q syndromes were p53 positive. P53 expression was positive in 5% of RA, 5% of RCMD, 18% of RAEB-1, 8% of RAEB-2 and 15% of MDS/MPN including CMML. P53 expression was significantly higher (51%) in patients with t-MDS (N=39). P53 positive patients showed a higher incidence of complex karyotype with ≥3 abnormalities (58%) and single/double abnormalities (40%). Only 7% of p53 positive patients had a normal karyotype. This is reflected by a higher proportion of patients with Int-2 and high risk IPSS (57% vs. 14%) and with high and very high IPSS-R (53% vs. 14%) in p53 positive patients compared to p53 negative patients. The median overall survival of p53 positive patients was 14 months compared to 33 months in p53 negative patients (p=0.000). The rate of AML transformation was 16% in p53 positive patients compared to 8% in p53 negative patients and the time to development of AML from MDS was shorter in p53 positive patients (9 months vs. 20 months).
Conclusion
Positive p53 expression of 16% in the MDS patients in this study reflected the incidence of p53 mutation published by prior studies. Positive p53 expression by IHC correlates with higher blast count, adverse WHO subgroup, complex karyotype, higher IPSS and IPSS-R, poor overall survival and increased risk of AML transformation. Analysis of p53 expression by IHC is a reproducible, rapid and inexpensive method and is a useful adjunctive prognostic tool in clinical practice.
Session topic: E-poster
Keyword(s): Immunohistochemistry, Myelodysplasia, P53, Prognosis
Type: Eposter Presentation
Background
Somatic mutations in TP53 have been shown to be associated with aggressive disease, resistance to therapy and poor survival in many cancers including haematological neoplasms. The incidence of TP53 mutations in Myelodysplastic Syndromes (MDS) is low (5-15%) compared to other malignancies but may be associated with adverse outcomes. Consistent correlations of up to 96% between TP53 mutation by conventional sequencing and demonstration of p53 expression by immunohistochemistry (IHC) has been demonstrated by prior studies.
Aims
We assessed p53 expression by IHC on marrow trephine samples of 246 MDS patients to correlate the p53 expression with their clinical characteristics and outcomes.
Methods
IHC for p53 expression on marrow trephines of 246 MDS patients diagnosed between 2003 and 2014 in a single centre were analysed using DO-7 monoclonal antibody. Clinical information and overall survival including transformation to acute myeloid leukaemia (AML) were obtained from clinical notes and patient information systems. P53 expression was determined by assessing 1000 haematopoietic cells under high magnification and scored using a Modified Quick Scoring System.
Results
Thirty nine patients (16%) were positive for p53 expression and 207 patients (84%) were negative. P53 positive patients showed greater degree of peripheral cytopenias and higher marrow blasts. None of the patients with WHO subgroups of RARS, RCMD-RS or MDS 5q syndromes were p53 positive. P53 expression was positive in 5% of RA, 5% of RCMD, 18% of RAEB-1, 8% of RAEB-2 and 15% of MDS/MPN including CMML. P53 expression was significantly higher (51%) in patients with t-MDS (N=39). P53 positive patients showed a higher incidence of complex karyotype with ≥3 abnormalities (58%) and single/double abnormalities (40%). Only 7% of p53 positive patients had a normal karyotype. This is reflected by a higher proportion of patients with Int-2 and high risk IPSS (57% vs. 14%) and with high and very high IPSS-R (53% vs. 14%) in p53 positive patients compared to p53 negative patients. The median overall survival of p53 positive patients was 14 months compared to 33 months in p53 negative patients (p=0.000). The rate of AML transformation was 16% in p53 positive patients compared to 8% in p53 negative patients and the time to development of AML from MDS was shorter in p53 positive patients (9 months vs. 20 months).
Conclusion
Positive p53 expression of 16% in the MDS patients in this study reflected the incidence of p53 mutation published by prior studies. Positive p53 expression by IHC correlates with higher blast count, adverse WHO subgroup, complex karyotype, higher IPSS and IPSS-R, poor overall survival and increased risk of AML transformation. Analysis of p53 expression by IHC is a reproducible, rapid and inexpensive method and is a useful adjunctive prognostic tool in clinical practice.
Session topic: E-poster
Keyword(s): Immunohistochemistry, Myelodysplasia, P53, Prognosis
Abstract: E1219
Type: Eposter Presentation
Background
Somatic mutations in TP53 have been shown to be associated with aggressive disease, resistance to therapy and poor survival in many cancers including haematological neoplasms. The incidence of TP53 mutations in Myelodysplastic Syndromes (MDS) is low (5-15%) compared to other malignancies but may be associated with adverse outcomes. Consistent correlations of up to 96% between TP53 mutation by conventional sequencing and demonstration of p53 expression by immunohistochemistry (IHC) has been demonstrated by prior studies.
Aims
We assessed p53 expression by IHC on marrow trephine samples of 246 MDS patients to correlate the p53 expression with their clinical characteristics and outcomes.
Methods
IHC for p53 expression on marrow trephines of 246 MDS patients diagnosed between 2003 and 2014 in a single centre were analysed using DO-7 monoclonal antibody. Clinical information and overall survival including transformation to acute myeloid leukaemia (AML) were obtained from clinical notes and patient information systems. P53 expression was determined by assessing 1000 haematopoietic cells under high magnification and scored using a Modified Quick Scoring System.
Results
Thirty nine patients (16%) were positive for p53 expression and 207 patients (84%) were negative. P53 positive patients showed greater degree of peripheral cytopenias and higher marrow blasts. None of the patients with WHO subgroups of RARS, RCMD-RS or MDS 5q syndromes were p53 positive. P53 expression was positive in 5% of RA, 5% of RCMD, 18% of RAEB-1, 8% of RAEB-2 and 15% of MDS/MPN including CMML. P53 expression was significantly higher (51%) in patients with t-MDS (N=39). P53 positive patients showed a higher incidence of complex karyotype with ≥3 abnormalities (58%) and single/double abnormalities (40%). Only 7% of p53 positive patients had a normal karyotype. This is reflected by a higher proportion of patients with Int-2 and high risk IPSS (57% vs. 14%) and with high and very high IPSS-R (53% vs. 14%) in p53 positive patients compared to p53 negative patients. The median overall survival of p53 positive patients was 14 months compared to 33 months in p53 negative patients (p=0.000). The rate of AML transformation was 16% in p53 positive patients compared to 8% in p53 negative patients and the time to development of AML from MDS was shorter in p53 positive patients (9 months vs. 20 months).
Conclusion
Positive p53 expression of 16% in the MDS patients in this study reflected the incidence of p53 mutation published by prior studies. Positive p53 expression by IHC correlates with higher blast count, adverse WHO subgroup, complex karyotype, higher IPSS and IPSS-R, poor overall survival and increased risk of AML transformation. Analysis of p53 expression by IHC is a reproducible, rapid and inexpensive method and is a useful adjunctive prognostic tool in clinical practice.
Session topic: E-poster
Keyword(s): Immunohistochemistry, Myelodysplasia, P53, Prognosis
Type: Eposter Presentation
Background
Somatic mutations in TP53 have been shown to be associated with aggressive disease, resistance to therapy and poor survival in many cancers including haematological neoplasms. The incidence of TP53 mutations in Myelodysplastic Syndromes (MDS) is low (5-15%) compared to other malignancies but may be associated with adverse outcomes. Consistent correlations of up to 96% between TP53 mutation by conventional sequencing and demonstration of p53 expression by immunohistochemistry (IHC) has been demonstrated by prior studies.
Aims
We assessed p53 expression by IHC on marrow trephine samples of 246 MDS patients to correlate the p53 expression with their clinical characteristics and outcomes.
Methods
IHC for p53 expression on marrow trephines of 246 MDS patients diagnosed between 2003 and 2014 in a single centre were analysed using DO-7 monoclonal antibody. Clinical information and overall survival including transformation to acute myeloid leukaemia (AML) were obtained from clinical notes and patient information systems. P53 expression was determined by assessing 1000 haematopoietic cells under high magnification and scored using a Modified Quick Scoring System.
Results
Thirty nine patients (16%) were positive for p53 expression and 207 patients (84%) were negative. P53 positive patients showed greater degree of peripheral cytopenias and higher marrow blasts. None of the patients with WHO subgroups of RARS, RCMD-RS or MDS 5q syndromes were p53 positive. P53 expression was positive in 5% of RA, 5% of RCMD, 18% of RAEB-1, 8% of RAEB-2 and 15% of MDS/MPN including CMML. P53 expression was significantly higher (51%) in patients with t-MDS (N=39). P53 positive patients showed a higher incidence of complex karyotype with ≥3 abnormalities (58%) and single/double abnormalities (40%). Only 7% of p53 positive patients had a normal karyotype. This is reflected by a higher proportion of patients with Int-2 and high risk IPSS (57% vs. 14%) and with high and very high IPSS-R (53% vs. 14%) in p53 positive patients compared to p53 negative patients. The median overall survival of p53 positive patients was 14 months compared to 33 months in p53 negative patients (p=0.000). The rate of AML transformation was 16% in p53 positive patients compared to 8% in p53 negative patients and the time to development of AML from MDS was shorter in p53 positive patients (9 months vs. 20 months).
Conclusion
Positive p53 expression of 16% in the MDS patients in this study reflected the incidence of p53 mutation published by prior studies. Positive p53 expression by IHC correlates with higher blast count, adverse WHO subgroup, complex karyotype, higher IPSS and IPSS-R, poor overall survival and increased risk of AML transformation. Analysis of p53 expression by IHC is a reproducible, rapid and inexpensive method and is a useful adjunctive prognostic tool in clinical practice.
Session topic: E-poster
Keyword(s): Immunohistochemistry, Myelodysplasia, P53, Prognosis
{{ help_message }}
{{filter}}


