FERRITINE LEVEL AND PERFORMANCE STATUS ARE SIGNIFICATIVE PROGNOSTIC FACTORS FOR OVERALL SURVIVAL IN LOWER-RISK MDS PATIENTS GRUPO ARGENTINO DE ESTUDIO DE LOS SINDROMES MIELODISPLASICOS
(Abstract release date: 05/19/16)
EHA Library. Enrico A. 06/09/16; 132761; E1212

Dr. Alicia Enrico
Contributions
Contributions
Abstract
Abstract: E1212
Type: Eposter Presentation
Background
Myelodysplastic syndromes (MSD) are a heterogeneous group of clonal haematopoietic stem cell malignancies characterized by defects in haematopoietic cell maduration/differentiation. According to the original IPSS, the majority of patients are classified within low or intermediate-I (lower) risk with a survival of >3.5 years. However, a large diversity exists within these patients varying in several characteristics at diagnosis. Up to 10% evolve to AML and 50% succumb as a result of the severity of cytopenias. The WPSS, MD Anderson (MDA) and IPSS-R recognized some IPSS limitations. The use of these systems has improved survival prediction but their usefulness is not clear in lower risk patients. Also, the inclusion of non-classical variables, as ferritine level or performance status, is also in debate.
Aims
To analyze the usefulness of risk stratification to predict survival and evolution to AML in lower risk patients. And, to test whether non classical variables are independent prognostic variables in these patients.
Methods
This is a retrospective study of 566 patients from the Registro Argentino de Enfermedades Hematologicas (RAEH), Sociedad Argentina de Hematologia, diagnosed between 2007 and 2015, last up-date Jan 2016. Out of the registry, 328 (57.9%) were selected and evaluated according to the IPSS criteria, excluding those with secondary MDS and with proliferative CMML.WPSS (both the one including transfusion dependence and with hemoglobin levels according to gender), MDA and the specific for Low Risk (MDA-LR), and IPSS-R systems were applied. Univariate (Kaplan-Meier and Long-rank) and multivariate (Cox regression) analysis were performed to evaluate survival and evolution to AML.
Results
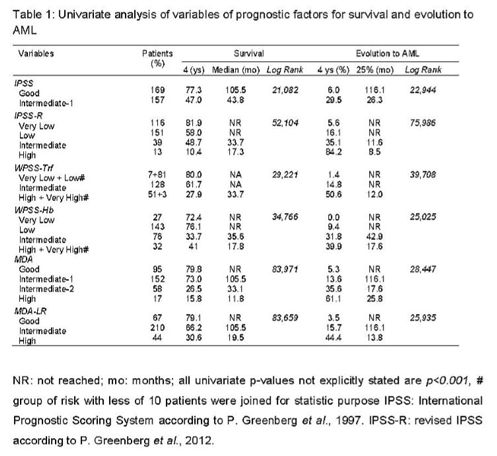
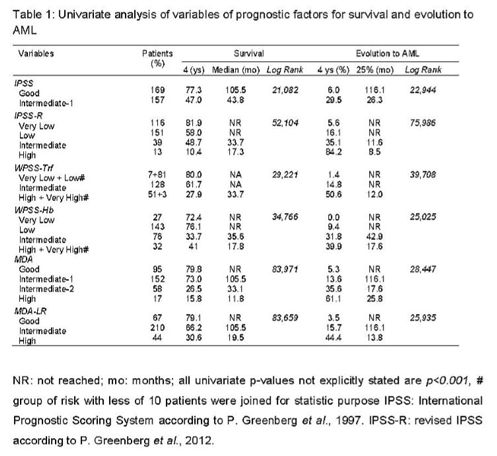
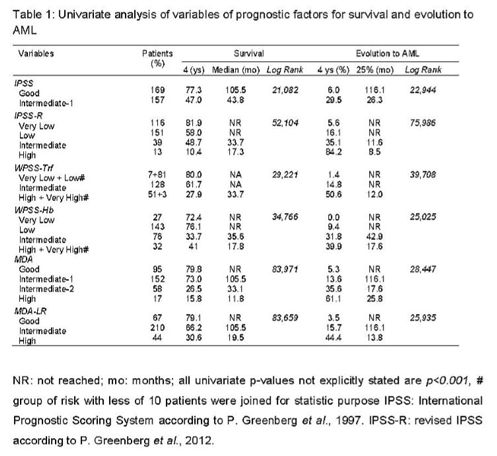
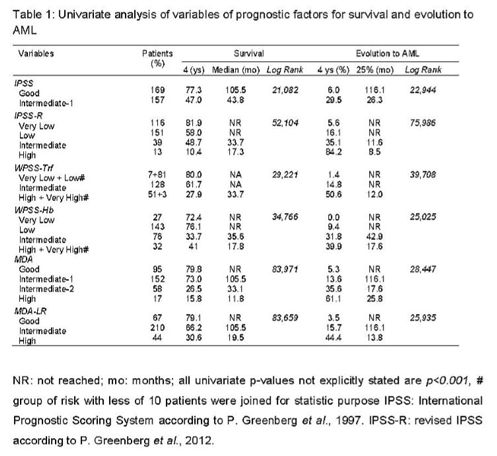
The selected 328 lower risk patients showed a median age of 72.5 years, 54.6% were male and 17.7% showed a performance status ≥2. With a median follow-up of 25.4 months, 86 (26.2%) died and 38 (11.6%) evolved to AML.Gender, ferritine level (<170, 170-350, >350 mg/ML) and all variables grouped according to different evaluated systems were significant predictive variables for prognosis. Table 1 shows the distribution of patients according to all evaluated systems and their respective median survival and time to evolution to AML. It also depicts that all systems were useful to predict outcome. The IPSS-R sustained its independence for both survival [p<0.001, exp(B) 1.676] and evolution to AML [p<0.001, exp(B) 2.544]. Also the classic MDA was useful for survival [p<0.001, exp(B) 1.987] and both WPSS for evolution to AML [p<0.001 and 0.02, exp(B) 2.281 and 0.554, respectively including either trf or Hb]. As the IPSS-R was the only system that sustained its independence to predict both survival and evolution to AML, all variables not included were analyzed in a multivariate model. Performance status and ferritine level were significative predictive parameters in the model to predict survival [p<0.001 and p=0.012, exp(B) 1.807 and 1.455]. However, any variable showed an independent prognostic impact for evolution to AML besides the IPSS-R.
Conclusion
WPSS, MDA, MDA-LR and IPSS-R systems allowed us to identify subgroups of patients (11.5% - 26.2%) that shift to worse prognosis categories in lower risk-IPSS patients. IPSS-R sustained its independence to predict both survival and evolution to AML, while the MDA did it for survival and the WPSS for leukemic evolution. Performance status and ferritine level were significative independent prognostic factors to predict survival along with the IPSS-R in lower risk patients.
Session topic: E-poster
Keyword(s): Myelodysplasia, Prognostic factor
Type: Eposter Presentation
Background
Myelodysplastic syndromes (MSD) are a heterogeneous group of clonal haematopoietic stem cell malignancies characterized by defects in haematopoietic cell maduration/differentiation. According to the original IPSS, the majority of patients are classified within low or intermediate-I (lower) risk with a survival of >3.5 years. However, a large diversity exists within these patients varying in several characteristics at diagnosis. Up to 10% evolve to AML and 50% succumb as a result of the severity of cytopenias. The WPSS, MD Anderson (MDA) and IPSS-R recognized some IPSS limitations. The use of these systems has improved survival prediction but their usefulness is not clear in lower risk patients. Also, the inclusion of non-classical variables, as ferritine level or performance status, is also in debate.
Aims
To analyze the usefulness of risk stratification to predict survival and evolution to AML in lower risk patients. And, to test whether non classical variables are independent prognostic variables in these patients.
Methods
This is a retrospective study of 566 patients from the Registro Argentino de Enfermedades Hematologicas (RAEH), Sociedad Argentina de Hematologia, diagnosed between 2007 and 2015, last up-date Jan 2016. Out of the registry, 328 (57.9%) were selected and evaluated according to the IPSS criteria, excluding those with secondary MDS and with proliferative CMML.WPSS (both the one including transfusion dependence and with hemoglobin levels according to gender), MDA and the specific for Low Risk (MDA-LR), and IPSS-R systems were applied. Univariate (Kaplan-Meier and Long-rank) and multivariate (Cox regression) analysis were performed to evaluate survival and evolution to AML.
Results
The selected 328 lower risk patients showed a median age of 72.5 years, 54.6% were male and 17.7% showed a performance status ≥2. With a median follow-up of 25.4 months, 86 (26.2%) died and 38 (11.6%) evolved to AML.Gender, ferritine level (<170, 170-350, >350 mg/ML) and all variables grouped according to different evaluated systems were significant predictive variables for prognosis. Table 1 shows the distribution of patients according to all evaluated systems and their respective median survival and time to evolution to AML. It also depicts that all systems were useful to predict outcome. The IPSS-R sustained its independence for both survival [p<0.001, exp(B) 1.676] and evolution to AML [p<0.001, exp(B) 2.544]. Also the classic MDA was useful for survival [p<0.001, exp(B) 1.987] and both WPSS for evolution to AML [p<0.001 and 0.02, exp(B) 2.281 and 0.554, respectively including either trf or Hb]. As the IPSS-R was the only system that sustained its independence to predict both survival and evolution to AML, all variables not included were analyzed in a multivariate model. Performance status and ferritine level were significative predictive parameters in the model to predict survival [p<0.001 and p=0.012, exp(B) 1.807 and 1.455]. However, any variable showed an independent prognostic impact for evolution to AML besides the IPSS-R.
Conclusion
WPSS, MDA, MDA-LR and IPSS-R systems allowed us to identify subgroups of patients (11.5% - 26.2%) that shift to worse prognosis categories in lower risk-IPSS patients. IPSS-R sustained its independence to predict both survival and evolution to AML, while the MDA did it for survival and the WPSS for leukemic evolution. Performance status and ferritine level were significative independent prognostic factors to predict survival along with the IPSS-R in lower risk patients.
Session topic: E-poster
Keyword(s): Myelodysplasia, Prognostic factor
Abstract: E1212
Type: Eposter Presentation
Background
Myelodysplastic syndromes (MSD) are a heterogeneous group of clonal haematopoietic stem cell malignancies characterized by defects in haematopoietic cell maduration/differentiation. According to the original IPSS, the majority of patients are classified within low or intermediate-I (lower) risk with a survival of >3.5 years. However, a large diversity exists within these patients varying in several characteristics at diagnosis. Up to 10% evolve to AML and 50% succumb as a result of the severity of cytopenias. The WPSS, MD Anderson (MDA) and IPSS-R recognized some IPSS limitations. The use of these systems has improved survival prediction but their usefulness is not clear in lower risk patients. Also, the inclusion of non-classical variables, as ferritine level or performance status, is also in debate.
Aims
To analyze the usefulness of risk stratification to predict survival and evolution to AML in lower risk patients. And, to test whether non classical variables are independent prognostic variables in these patients.
Methods
This is a retrospective study of 566 patients from the Registro Argentino de Enfermedades Hematologicas (RAEH), Sociedad Argentina de Hematologia, diagnosed between 2007 and 2015, last up-date Jan 2016. Out of the registry, 328 (57.9%) were selected and evaluated according to the IPSS criteria, excluding those with secondary MDS and with proliferative CMML.WPSS (both the one including transfusion dependence and with hemoglobin levels according to gender), MDA and the specific for Low Risk (MDA-LR), and IPSS-R systems were applied. Univariate (Kaplan-Meier and Long-rank) and multivariate (Cox regression) analysis were performed to evaluate survival and evolution to AML.
Results
The selected 328 lower risk patients showed a median age of 72.5 years, 54.6% were male and 17.7% showed a performance status ≥2. With a median follow-up of 25.4 months, 86 (26.2%) died and 38 (11.6%) evolved to AML.Gender, ferritine level (<170, 170-350, >350 mg/ML) and all variables grouped according to different evaluated systems were significant predictive variables for prognosis. Table 1 shows the distribution of patients according to all evaluated systems and their respective median survival and time to evolution to AML. It also depicts that all systems were useful to predict outcome. The IPSS-R sustained its independence for both survival [p<0.001, exp(B) 1.676] and evolution to AML [p<0.001, exp(B) 2.544]. Also the classic MDA was useful for survival [p<0.001, exp(B) 1.987] and both WPSS for evolution to AML [p<0.001 and 0.02, exp(B) 2.281 and 0.554, respectively including either trf or Hb]. As the IPSS-R was the only system that sustained its independence to predict both survival and evolution to AML, all variables not included were analyzed in a multivariate model. Performance status and ferritine level were significative predictive parameters in the model to predict survival [p<0.001 and p=0.012, exp(B) 1.807 and 1.455]. However, any variable showed an independent prognostic impact for evolution to AML besides the IPSS-R.
Conclusion
WPSS, MDA, MDA-LR and IPSS-R systems allowed us to identify subgroups of patients (11.5% - 26.2%) that shift to worse prognosis categories in lower risk-IPSS patients. IPSS-R sustained its independence to predict both survival and evolution to AML, while the MDA did it for survival and the WPSS for leukemic evolution. Performance status and ferritine level were significative independent prognostic factors to predict survival along with the IPSS-R in lower risk patients.
Session topic: E-poster
Keyword(s): Myelodysplasia, Prognostic factor
Type: Eposter Presentation
Background
Myelodysplastic syndromes (MSD) are a heterogeneous group of clonal haematopoietic stem cell malignancies characterized by defects in haematopoietic cell maduration/differentiation. According to the original IPSS, the majority of patients are classified within low or intermediate-I (lower) risk with a survival of >3.5 years. However, a large diversity exists within these patients varying in several characteristics at diagnosis. Up to 10% evolve to AML and 50% succumb as a result of the severity of cytopenias. The WPSS, MD Anderson (MDA) and IPSS-R recognized some IPSS limitations. The use of these systems has improved survival prediction but their usefulness is not clear in lower risk patients. Also, the inclusion of non-classical variables, as ferritine level or performance status, is also in debate.
Aims
To analyze the usefulness of risk stratification to predict survival and evolution to AML in lower risk patients. And, to test whether non classical variables are independent prognostic variables in these patients.
Methods
This is a retrospective study of 566 patients from the Registro Argentino de Enfermedades Hematologicas (RAEH), Sociedad Argentina de Hematologia, diagnosed between 2007 and 2015, last up-date Jan 2016. Out of the registry, 328 (57.9%) were selected and evaluated according to the IPSS criteria, excluding those with secondary MDS and with proliferative CMML.WPSS (both the one including transfusion dependence and with hemoglobin levels according to gender), MDA and the specific for Low Risk (MDA-LR), and IPSS-R systems were applied. Univariate (Kaplan-Meier and Long-rank) and multivariate (Cox regression) analysis were performed to evaluate survival and evolution to AML.
Results
The selected 328 lower risk patients showed a median age of 72.5 years, 54.6% were male and 17.7% showed a performance status ≥2. With a median follow-up of 25.4 months, 86 (26.2%) died and 38 (11.6%) evolved to AML.Gender, ferritine level (<170, 170-350, >350 mg/ML) and all variables grouped according to different evaluated systems were significant predictive variables for prognosis. Table 1 shows the distribution of patients according to all evaluated systems and their respective median survival and time to evolution to AML. It also depicts that all systems were useful to predict outcome. The IPSS-R sustained its independence for both survival [p<0.001, exp(B) 1.676] and evolution to AML [p<0.001, exp(B) 2.544]. Also the classic MDA was useful for survival [p<0.001, exp(B) 1.987] and both WPSS for evolution to AML [p<0.001 and 0.02, exp(B) 2.281 and 0.554, respectively including either trf or Hb]. As the IPSS-R was the only system that sustained its independence to predict both survival and evolution to AML, all variables not included were analyzed in a multivariate model. Performance status and ferritine level were significative predictive parameters in the model to predict survival [p<0.001 and p=0.012, exp(B) 1.807 and 1.455]. However, any variable showed an independent prognostic impact for evolution to AML besides the IPSS-R.
Conclusion
WPSS, MDA, MDA-LR and IPSS-R systems allowed us to identify subgroups of patients (11.5% - 26.2%) that shift to worse prognosis categories in lower risk-IPSS patients. IPSS-R sustained its independence to predict both survival and evolution to AML, while the MDA did it for survival and the WPSS for leukemic evolution. Performance status and ferritine level were significative independent prognostic factors to predict survival along with the IPSS-R in lower risk patients.
Session topic: E-poster
Keyword(s): Myelodysplasia, Prognostic factor
{{ help_message }}
{{filter}}


