THERAPY RELATED MYELOID NEOPLASM FOLLOWING RADIOTHERAPY HAS HIGHER INCIDENCE OF POOR RISK CYTOGENETICS AND ARE ASSOCIATED WITH POOR SURVIVAL COMPARED TO DE NOVO MDS CASES
(Abstract release date: 05/19/16)
EHA Library. Singhal D. 06/09/16; 132756; E1207

Dr. Deepak Singhal
Contributions
Contributions
Abstract
Abstract: E1207
Type: Eposter Presentation
Background
Therapy-related myeloid neoplasms (T-MN) are well-known complication of prior cytotoxic/radiation therapy for malignancies and auto-immune diseases and are associated with poor survival compared to de novo MDS cases;most probably due to higher rate of poor cytogenetic in T-MN cases. Poor prognosis of T-MN cases following prior cytotoxic chemotherapy (CT) exposure is well established, however, there is ongoing debate about the prognosis of radiotherapy (RT) only associated T-MN cases.
Aims
This study compares the prognosis of T-MN cases following CT, RT and de novo MDS cases enrolled in the South Australian MDS (SA-MDS) Registry.
Methods
Demographic, clinical, cytogenetic and laboratory data on 744 de-novo and 148 T-MN patients were analysed. Survivals between the groups were compared by using log-rank test and were plotted using Kaplan Meier curve. Categorical variables were compared by using Chi-square test.
Results
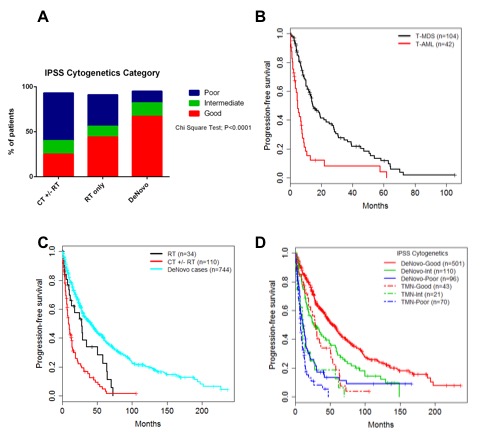
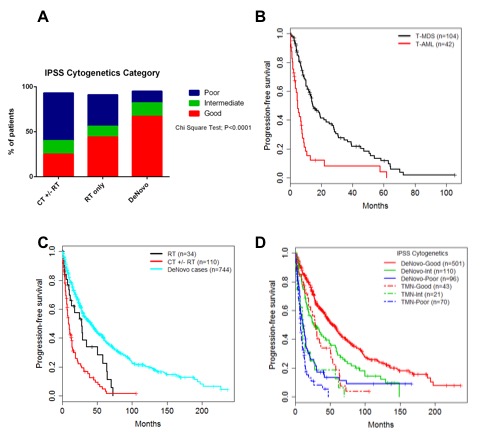
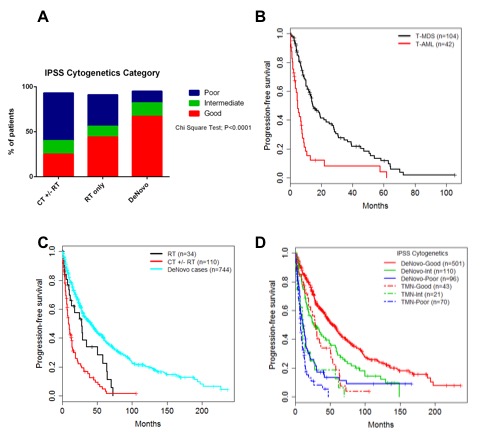
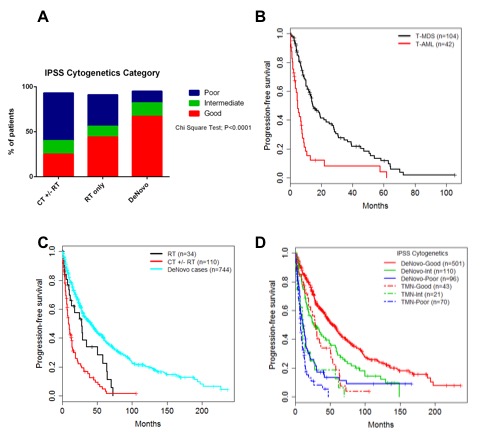
Median age of T-MN and de novo MDS was 71 (20-91) and 73 years (19-98). Most frequent primary diseases (PD) were lymphoproliferative diseases (n=56, 38%) and prostate cancer (n=22, 15%). Sixty-four (43%) patients had received CT only, 34 (23%) patients RT only, and 48 (32%) patients received both CT and RT for PD. 29(20%) patients received autologous stem cell transplant for their PD. During follow up, 42(28%) patients developed T-AML, while 104 (70%) developed T-MDS. The median time between cytotoxic treatment and t-MN diagnosis was 38.5months for RT only (range 0.9-123) and 31.9months (range 0.2-216.2) for CT(±RT) patients, respectively.As shown in table 1 and Fig1A, poor risk cytogenetic cases were significantly higher in T-MN cases treated with CT compared to cases treated with RT alone and de novo MDS cases (52% vs 25% vs 13% respectively; P<0.0001). Similarly, 47% CT(±RT)patients had R-IPSS defined poor and very poor cytogenetics compared to 35% of RT only and 13% of de-novo MDS/AML patients (P=<0.0001). Overall, 40(27%) of T-MN patients received disease modifying therapy (Induction CT, Hypomethylating agents, low dose Ara-C, and Allogeneic transplant).Within the T-MN group (144 patients), T-MDS patients had significantly better median survival than T-AML (14.7 vs 5.0 months, P<0.0001)(Fig 1B). T-MN patients who received prior RT only had worse median survival than de-novo patients but better than T-MN patients receiving prior CT (±RT) (9.7 vs 27.9 vs 41.3 months; p=0.001)(Fig 1C). Further, within the individual IPSS cytogenetic risk category, T-MN consistently had poor median survival than de-novo patients (Fig.1D) regardless of the type of prior therapy(p=0.001).Table1: Distribution of cytogenetic categories in de-novo &T-MN patients according to IPSS, R-IPSS and prior treatment type
Conclusion
T-MN patients receiving prior CT(± RT) have poorer survival compared to RT only & de novo MDS patients. Contrary to the published literature (Nardi et al JCO 2012), our data suggest that the incidence of adverse cytogenetics is higher in T-MN patients who received prior RT compared to de-novo patients. T-MN patients have consistently poor survival than de-novo patients even when matched for IPSS cytogenetic categories.
Session topic: E-poster
Keyword(s): Chemotherapy, Cytogenetics, Radiotherapy, Therapy-related AML
Type: Eposter Presentation
Background
Therapy-related myeloid neoplasms (T-MN) are well-known complication of prior cytotoxic/radiation therapy for malignancies and auto-immune diseases and are associated with poor survival compared to de novo MDS cases;most probably due to higher rate of poor cytogenetic in T-MN cases. Poor prognosis of T-MN cases following prior cytotoxic chemotherapy (CT) exposure is well established, however, there is ongoing debate about the prognosis of radiotherapy (RT) only associated T-MN cases.
Aims
This study compares the prognosis of T-MN cases following CT, RT and de novo MDS cases enrolled in the South Australian MDS (SA-MDS) Registry.
Methods
Demographic, clinical, cytogenetic and laboratory data on 744 de-novo and 148 T-MN patients were analysed. Survivals between the groups were compared by using log-rank test and were plotted using Kaplan Meier curve. Categorical variables were compared by using Chi-square test.
Results
Median age of T-MN and de novo MDS was 71 (20-91) and 73 years (19-98). Most frequent primary diseases (PD) were lymphoproliferative diseases (n=56, 38%) and prostate cancer (n=22, 15%). Sixty-four (43%) patients had received CT only, 34 (23%) patients RT only, and 48 (32%) patients received both CT and RT for PD. 29(20%) patients received autologous stem cell transplant for their PD. During follow up, 42(28%) patients developed T-AML, while 104 (70%) developed T-MDS. The median time between cytotoxic treatment and t-MN diagnosis was 38.5months for RT only (range 0.9-123) and 31.9months (range 0.2-216.2) for CT(±RT) patients, respectively.As shown in table 1 and Fig1A, poor risk cytogenetic cases were significantly higher in T-MN cases treated with CT compared to cases treated with RT alone and de novo MDS cases (52% vs 25% vs 13% respectively; P<0.0001). Similarly, 47% CT(±RT)patients had R-IPSS defined poor and very poor cytogenetics compared to 35% of RT only and 13% of de-novo MDS/AML patients (P=<0.0001). Overall, 40(27%) of T-MN patients received disease modifying therapy (Induction CT, Hypomethylating agents, low dose Ara-C, and Allogeneic transplant).Within the T-MN group (144 patients), T-MDS patients had significantly better median survival than T-AML (14.7 vs 5.0 months, P<0.0001)(Fig 1B). T-MN patients who received prior RT only had worse median survival than de-novo patients but better than T-MN patients receiving prior CT (±RT) (9.7 vs 27.9 vs 41.3 months; p=0.001)(Fig 1C). Further, within the individual IPSS cytogenetic risk category, T-MN consistently had poor median survival than de-novo patients (Fig.1D) regardless of the type of prior therapy(p=0.001).Table1: Distribution of cytogenetic categories in de-novo &T-MN patients according to IPSS, R-IPSS and prior treatment type
| IPSS cytogenetic category | CT±RTN=112 | RTN=34 | De novoN=741 | R-IPSScytogenetic category | CT±RTN=112 | RTN=34 | De novoN=741 |
| Good | 28(25%) | 15(44%) | 498(67%) | Very Good | 2(2%) | 1(3%) | 30(4%) |
| Intermediate | 17(15%) | 4(12%) | 111(15%) | Good | 26(23%) | 14(41%) | 474(64%) |
| Poor | 58(52%) | 12(35%) | 95(13%) | Intermediate | 22(20%) | 4(12%) | 103(14%) |
| Not available | 9(8%) | 3(9%) | 37(5%) | Poor | 25(22%) | 3(9%) | 31(4%) |
| Very Poor | 28(25%) | 9(26%) | 66(9%) | ||||
| Not available | 9(8%) | 3(9%) | 37(5%) |
Conclusion
T-MN patients receiving prior CT(± RT) have poorer survival compared to RT only & de novo MDS patients. Contrary to the published literature (Nardi et al JCO 2012), our data suggest that the incidence of adverse cytogenetics is higher in T-MN patients who received prior RT compared to de-novo patients. T-MN patients have consistently poor survival than de-novo patients even when matched for IPSS cytogenetic categories.
Session topic: E-poster
Keyword(s): Chemotherapy, Cytogenetics, Radiotherapy, Therapy-related AML
Abstract: E1207
Type: Eposter Presentation
Background
Therapy-related myeloid neoplasms (T-MN) are well-known complication of prior cytotoxic/radiation therapy for malignancies and auto-immune diseases and are associated with poor survival compared to de novo MDS cases;most probably due to higher rate of poor cytogenetic in T-MN cases. Poor prognosis of T-MN cases following prior cytotoxic chemotherapy (CT) exposure is well established, however, there is ongoing debate about the prognosis of radiotherapy (RT) only associated T-MN cases.
Aims
This study compares the prognosis of T-MN cases following CT, RT and de novo MDS cases enrolled in the South Australian MDS (SA-MDS) Registry.
Methods
Demographic, clinical, cytogenetic and laboratory data on 744 de-novo and 148 T-MN patients were analysed. Survivals between the groups were compared by using log-rank test and were plotted using Kaplan Meier curve. Categorical variables were compared by using Chi-square test.
Results
Median age of T-MN and de novo MDS was 71 (20-91) and 73 years (19-98). Most frequent primary diseases (PD) were lymphoproliferative diseases (n=56, 38%) and prostate cancer (n=22, 15%). Sixty-four (43%) patients had received CT only, 34 (23%) patients RT only, and 48 (32%) patients received both CT and RT for PD. 29(20%) patients received autologous stem cell transplant for their PD. During follow up, 42(28%) patients developed T-AML, while 104 (70%) developed T-MDS. The median time between cytotoxic treatment and t-MN diagnosis was 38.5months for RT only (range 0.9-123) and 31.9months (range 0.2-216.2) for CT(±RT) patients, respectively.As shown in table 1 and Fig1A, poor risk cytogenetic cases were significantly higher in T-MN cases treated with CT compared to cases treated with RT alone and de novo MDS cases (52% vs 25% vs 13% respectively; P<0.0001). Similarly, 47% CT(±RT)patients had R-IPSS defined poor and very poor cytogenetics compared to 35% of RT only and 13% of de-novo MDS/AML patients (P=<0.0001). Overall, 40(27%) of T-MN patients received disease modifying therapy (Induction CT, Hypomethylating agents, low dose Ara-C, and Allogeneic transplant).Within the T-MN group (144 patients), T-MDS patients had significantly better median survival than T-AML (14.7 vs 5.0 months, P<0.0001)(Fig 1B). T-MN patients who received prior RT only had worse median survival than de-novo patients but better than T-MN patients receiving prior CT (±RT) (9.7 vs 27.9 vs 41.3 months; p=0.001)(Fig 1C). Further, within the individual IPSS cytogenetic risk category, T-MN consistently had poor median survival than de-novo patients (Fig.1D) regardless of the type of prior therapy(p=0.001).Table1: Distribution of cytogenetic categories in de-novo &T-MN patients according to IPSS, R-IPSS and prior treatment type
Conclusion
T-MN patients receiving prior CT(± RT) have poorer survival compared to RT only & de novo MDS patients. Contrary to the published literature (Nardi et al JCO 2012), our data suggest that the incidence of adverse cytogenetics is higher in T-MN patients who received prior RT compared to de-novo patients. T-MN patients have consistently poor survival than de-novo patients even when matched for IPSS cytogenetic categories.
Session topic: E-poster
Keyword(s): Chemotherapy, Cytogenetics, Radiotherapy, Therapy-related AML
Type: Eposter Presentation
Background
Therapy-related myeloid neoplasms (T-MN) are well-known complication of prior cytotoxic/radiation therapy for malignancies and auto-immune diseases and are associated with poor survival compared to de novo MDS cases;most probably due to higher rate of poor cytogenetic in T-MN cases. Poor prognosis of T-MN cases following prior cytotoxic chemotherapy (CT) exposure is well established, however, there is ongoing debate about the prognosis of radiotherapy (RT) only associated T-MN cases.
Aims
This study compares the prognosis of T-MN cases following CT, RT and de novo MDS cases enrolled in the South Australian MDS (SA-MDS) Registry.
Methods
Demographic, clinical, cytogenetic and laboratory data on 744 de-novo and 148 T-MN patients were analysed. Survivals between the groups were compared by using log-rank test and were plotted using Kaplan Meier curve. Categorical variables were compared by using Chi-square test.
Results
Median age of T-MN and de novo MDS was 71 (20-91) and 73 years (19-98). Most frequent primary diseases (PD) were lymphoproliferative diseases (n=56, 38%) and prostate cancer (n=22, 15%). Sixty-four (43%) patients had received CT only, 34 (23%) patients RT only, and 48 (32%) patients received both CT and RT for PD. 29(20%) patients received autologous stem cell transplant for their PD. During follow up, 42(28%) patients developed T-AML, while 104 (70%) developed T-MDS. The median time between cytotoxic treatment and t-MN diagnosis was 38.5months for RT only (range 0.9-123) and 31.9months (range 0.2-216.2) for CT(±RT) patients, respectively.As shown in table 1 and Fig1A, poor risk cytogenetic cases were significantly higher in T-MN cases treated with CT compared to cases treated with RT alone and de novo MDS cases (52% vs 25% vs 13% respectively; P<0.0001). Similarly, 47% CT(±RT)patients had R-IPSS defined poor and very poor cytogenetics compared to 35% of RT only and 13% of de-novo MDS/AML patients (P=<0.0001). Overall, 40(27%) of T-MN patients received disease modifying therapy (Induction CT, Hypomethylating agents, low dose Ara-C, and Allogeneic transplant).Within the T-MN group (144 patients), T-MDS patients had significantly better median survival than T-AML (14.7 vs 5.0 months, P<0.0001)(Fig 1B). T-MN patients who received prior RT only had worse median survival than de-novo patients but better than T-MN patients receiving prior CT (±RT) (9.7 vs 27.9 vs 41.3 months; p=0.001)(Fig 1C). Further, within the individual IPSS cytogenetic risk category, T-MN consistently had poor median survival than de-novo patients (Fig.1D) regardless of the type of prior therapy(p=0.001).Table1: Distribution of cytogenetic categories in de-novo &T-MN patients according to IPSS, R-IPSS and prior treatment type
| IPSS cytogenetic category | CT±RTN=112 | RTN=34 | De novoN=741 | R-IPSScytogenetic category | CT±RTN=112 | RTN=34 | De novoN=741 |
| Good | 28(25%) | 15(44%) | 498(67%) | Very Good | 2(2%) | 1(3%) | 30(4%) |
| Intermediate | 17(15%) | 4(12%) | 111(15%) | Good | 26(23%) | 14(41%) | 474(64%) |
| Poor | 58(52%) | 12(35%) | 95(13%) | Intermediate | 22(20%) | 4(12%) | 103(14%) |
| Not available | 9(8%) | 3(9%) | 37(5%) | Poor | 25(22%) | 3(9%) | 31(4%) |
| Very Poor | 28(25%) | 9(26%) | 66(9%) | ||||
| Not available | 9(8%) | 3(9%) | 37(5%) |
Conclusion
T-MN patients receiving prior CT(± RT) have poorer survival compared to RT only & de novo MDS patients. Contrary to the published literature (Nardi et al JCO 2012), our data suggest that the incidence of adverse cytogenetics is higher in T-MN patients who received prior RT compared to de-novo patients. T-MN patients have consistently poor survival than de-novo patients even when matched for IPSS cytogenetic categories.
Session topic: E-poster
Keyword(s): Chemotherapy, Cytogenetics, Radiotherapy, Therapy-related AML
{{ help_message }}
{{filter}}


