RESPIRATORY VIRAL INFECTIONS IN HEMATOLOGIC PATIENTS IN OUR ENVIRONMENT. A RETROSPECTIVE STUDY.
(Abstract release date: 05/19/16)
EHA Library. Cidre R. 06/09/16; 132723; E1174

Ms. Raquel Cidre
Contributions
Contributions
Abstract
Abstract: E1174
Type: Eposter Presentation
Background
Respiratory viral infections are an important cause of morbidity and mortality in immunocompromised hosts. Hematology patients are especially susceptible due to their underlying disease and the treatments they receive. Rhinovirus, Influenza, Parainfluenza and RSV are some of the most frequent agents. Molecular diagnostic techniques have improved over time, providing fast and accurate results.
Aims
Analize the characteristics of viral respiratory infections in our patients.
Methods
A retrospective, descriptive study including 237 hematologic patients from the University Hospital Complex of Vigo with suspected respiratory viral infection for a period of two years (May 2013-May 2015). We collected 401 PCR samples of respiratory viruses in nasopharyngeal swab and BAL, focusing on the following data: demographic characteristics, underlying disease, comorbidities, symptoms, diagnostic tests, treatment and clinical evolution.
Results
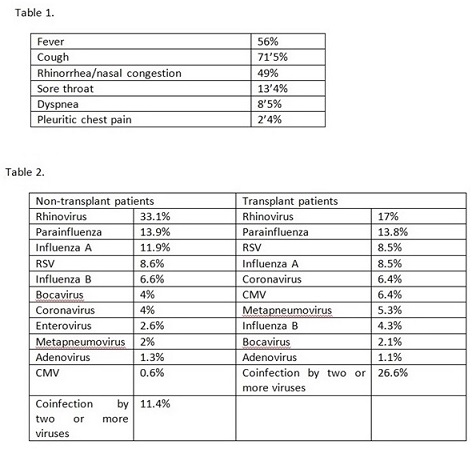
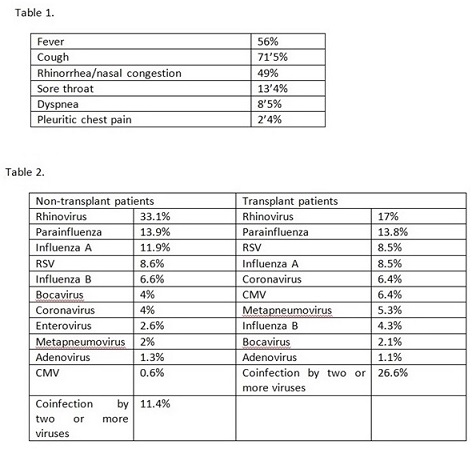
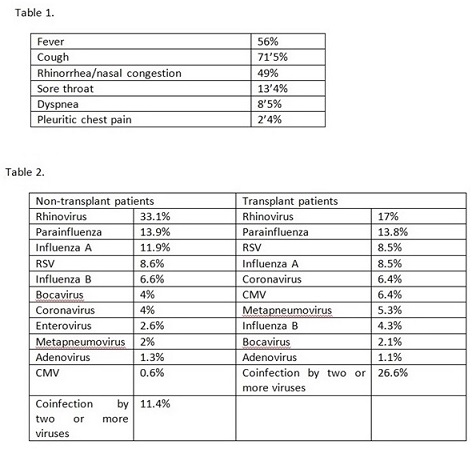
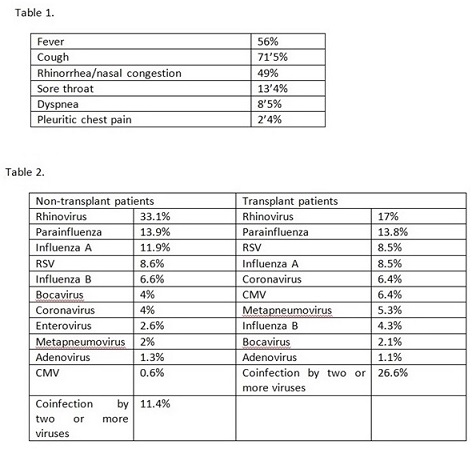
122 male patients and 115 female, with a median age of 64 years old (range 4-89). 88 underwent HSCT – 46 autologous, 42 allogeneic (35 HLA identical, 6 haploidentical and 1 cord blood).61’5% of the samples were positive for one or more respiratory viruses (63’9% in transplant patients vs 59’8% in non-transplant). 89’4% were positive in nasopharyngeal samples, 4’7% in BAL and 5’9% in both. Causal agents are shown in Table 2. 17% of samples were positive for more than one virus, and 15’4% had microbiologic evidence of infection by a different type of microorganism.30’5% of the infections were considered nosocomial. Concerning those with an infection acquired in the community, 59’6% patients required hospitalization due to the respiratory illness. The symptoms referred by our patients are shown in table 1. 61’4% of the demonstrated viral infections were associated with lymphopenia. Hypogammaglobulinemia was observed in 57%. 30’3% presented comorbidities associated with an increased risk of respiratory infection (underlying heart or lung disease, smoking, HIV positivity, DM or other tumors).Radiologic findings: 50’8% showed a normal X-ray chest image or nonspecific findings, 11’4% pneumonic consolidation and 6’5% signs of atypical infection.42 patients underwent a bronchoscopy. 12 obtained concordant results with nasopharyngeal samples. 10 patients with a negative nasopharyngeal swab had a viral identification in the BAL. We had an isolated case with different results in each sample (a RSV was found in the nasopharyngeal swab and a coronavirus in the BAL). In 8 patients we found other microorganisms (bacteria, fungus).Influenza virus infections were treated with oseltamivir. CMV infections in transplant recipients received immunoglobulins and ganciclovir. 28% of the RSV were treated with immunoglobulins and ribavirin. In most patients the outcome was good. 5 patients died, in 4 of them the respiratory infection was the main cause of death.
Conclusion
Our study confirms that viral respiratory infections are a common cause of morbidity in hematologic patients, even though related mortality was low. The most common symptoms were those of upper airway involvement. 44% of the patients remained afebrile during the course of infection. The presence of other comorbidities, lymphopenia and/or hypogammaglobulinemia seemed to be related with these infections. Although we didn’t find an increased rate of infection in transplant recipient patients, it seems that several microorganisms coinfections are more common in this group. Molecular techniques like PCR have replaced previous diagnostic procedures (like virus cultures), demonstrating a higher sensibility. Given the high rate of nosocomial infections, we would like to highlight the importance of vaccinating staff and family, and isolation measures in patients with suspected respiratory infections transmitted by droplets or contact.
Session topic: E-poster
Keyword(s): Infection
Type: Eposter Presentation
Background
Respiratory viral infections are an important cause of morbidity and mortality in immunocompromised hosts. Hematology patients are especially susceptible due to their underlying disease and the treatments they receive. Rhinovirus, Influenza, Parainfluenza and RSV are some of the most frequent agents. Molecular diagnostic techniques have improved over time, providing fast and accurate results.
Aims
Analize the characteristics of viral respiratory infections in our patients.
Methods
A retrospective, descriptive study including 237 hematologic patients from the University Hospital Complex of Vigo with suspected respiratory viral infection for a period of two years (May 2013-May 2015). We collected 401 PCR samples of respiratory viruses in nasopharyngeal swab and BAL, focusing on the following data: demographic characteristics, underlying disease, comorbidities, symptoms, diagnostic tests, treatment and clinical evolution.
Results
122 male patients and 115 female, with a median age of 64 years old (range 4-89). 88 underwent HSCT – 46 autologous, 42 allogeneic (35 HLA identical, 6 haploidentical and 1 cord blood).61’5% of the samples were positive for one or more respiratory viruses (63’9% in transplant patients vs 59’8% in non-transplant). 89’4% were positive in nasopharyngeal samples, 4’7% in BAL and 5’9% in both. Causal agents are shown in Table 2. 17% of samples were positive for more than one virus, and 15’4% had microbiologic evidence of infection by a different type of microorganism.30’5% of the infections were considered nosocomial. Concerning those with an infection acquired in the community, 59’6% patients required hospitalization due to the respiratory illness. The symptoms referred by our patients are shown in table 1. 61’4% of the demonstrated viral infections were associated with lymphopenia. Hypogammaglobulinemia was observed in 57%. 30’3% presented comorbidities associated with an increased risk of respiratory infection (underlying heart or lung disease, smoking, HIV positivity, DM or other tumors).Radiologic findings: 50’8% showed a normal X-ray chest image or nonspecific findings, 11’4% pneumonic consolidation and 6’5% signs of atypical infection.42 patients underwent a bronchoscopy. 12 obtained concordant results with nasopharyngeal samples. 10 patients with a negative nasopharyngeal swab had a viral identification in the BAL. We had an isolated case with different results in each sample (a RSV was found in the nasopharyngeal swab and a coronavirus in the BAL). In 8 patients we found other microorganisms (bacteria, fungus).Influenza virus infections were treated with oseltamivir. CMV infections in transplant recipients received immunoglobulins and ganciclovir. 28% of the RSV were treated with immunoglobulins and ribavirin. In most patients the outcome was good. 5 patients died, in 4 of them the respiratory infection was the main cause of death.
Conclusion
Our study confirms that viral respiratory infections are a common cause of morbidity in hematologic patients, even though related mortality was low. The most common symptoms were those of upper airway involvement. 44% of the patients remained afebrile during the course of infection. The presence of other comorbidities, lymphopenia and/or hypogammaglobulinemia seemed to be related with these infections. Although we didn’t find an increased rate of infection in transplant recipient patients, it seems that several microorganisms coinfections are more common in this group. Molecular techniques like PCR have replaced previous diagnostic procedures (like virus cultures), demonstrating a higher sensibility. Given the high rate of nosocomial infections, we would like to highlight the importance of vaccinating staff and family, and isolation measures in patients with suspected respiratory infections transmitted by droplets or contact.
Session topic: E-poster
Keyword(s): Infection
Abstract: E1174
Type: Eposter Presentation
Background
Respiratory viral infections are an important cause of morbidity and mortality in immunocompromised hosts. Hematology patients are especially susceptible due to their underlying disease and the treatments they receive. Rhinovirus, Influenza, Parainfluenza and RSV are some of the most frequent agents. Molecular diagnostic techniques have improved over time, providing fast and accurate results.
Aims
Analize the characteristics of viral respiratory infections in our patients.
Methods
A retrospective, descriptive study including 237 hematologic patients from the University Hospital Complex of Vigo with suspected respiratory viral infection for a period of two years (May 2013-May 2015). We collected 401 PCR samples of respiratory viruses in nasopharyngeal swab and BAL, focusing on the following data: demographic characteristics, underlying disease, comorbidities, symptoms, diagnostic tests, treatment and clinical evolution.
Results
122 male patients and 115 female, with a median age of 64 years old (range 4-89). 88 underwent HSCT – 46 autologous, 42 allogeneic (35 HLA identical, 6 haploidentical and 1 cord blood).61’5% of the samples were positive for one or more respiratory viruses (63’9% in transplant patients vs 59’8% in non-transplant). 89’4% were positive in nasopharyngeal samples, 4’7% in BAL and 5’9% in both. Causal agents are shown in Table 2. 17% of samples were positive for more than one virus, and 15’4% had microbiologic evidence of infection by a different type of microorganism.30’5% of the infections were considered nosocomial. Concerning those with an infection acquired in the community, 59’6% patients required hospitalization due to the respiratory illness. The symptoms referred by our patients are shown in table 1. 61’4% of the demonstrated viral infections were associated with lymphopenia. Hypogammaglobulinemia was observed in 57%. 30’3% presented comorbidities associated with an increased risk of respiratory infection (underlying heart or lung disease, smoking, HIV positivity, DM or other tumors).Radiologic findings: 50’8% showed a normal X-ray chest image or nonspecific findings, 11’4% pneumonic consolidation and 6’5% signs of atypical infection.42 patients underwent a bronchoscopy. 12 obtained concordant results with nasopharyngeal samples. 10 patients with a negative nasopharyngeal swab had a viral identification in the BAL. We had an isolated case with different results in each sample (a RSV was found in the nasopharyngeal swab and a coronavirus in the BAL). In 8 patients we found other microorganisms (bacteria, fungus).Influenza virus infections were treated with oseltamivir. CMV infections in transplant recipients received immunoglobulins and ganciclovir. 28% of the RSV were treated with immunoglobulins and ribavirin. In most patients the outcome was good. 5 patients died, in 4 of them the respiratory infection was the main cause of death.
Conclusion
Our study confirms that viral respiratory infections are a common cause of morbidity in hematologic patients, even though related mortality was low. The most common symptoms were those of upper airway involvement. 44% of the patients remained afebrile during the course of infection. The presence of other comorbidities, lymphopenia and/or hypogammaglobulinemia seemed to be related with these infections. Although we didn’t find an increased rate of infection in transplant recipient patients, it seems that several microorganisms coinfections are more common in this group. Molecular techniques like PCR have replaced previous diagnostic procedures (like virus cultures), demonstrating a higher sensibility. Given the high rate of nosocomial infections, we would like to highlight the importance of vaccinating staff and family, and isolation measures in patients with suspected respiratory infections transmitted by droplets or contact.
Session topic: E-poster
Keyword(s): Infection
Type: Eposter Presentation
Background
Respiratory viral infections are an important cause of morbidity and mortality in immunocompromised hosts. Hematology patients are especially susceptible due to their underlying disease and the treatments they receive. Rhinovirus, Influenza, Parainfluenza and RSV are some of the most frequent agents. Molecular diagnostic techniques have improved over time, providing fast and accurate results.
Aims
Analize the characteristics of viral respiratory infections in our patients.
Methods
A retrospective, descriptive study including 237 hematologic patients from the University Hospital Complex of Vigo with suspected respiratory viral infection for a period of two years (May 2013-May 2015). We collected 401 PCR samples of respiratory viruses in nasopharyngeal swab and BAL, focusing on the following data: demographic characteristics, underlying disease, comorbidities, symptoms, diagnostic tests, treatment and clinical evolution.
Results
122 male patients and 115 female, with a median age of 64 years old (range 4-89). 88 underwent HSCT – 46 autologous, 42 allogeneic (35 HLA identical, 6 haploidentical and 1 cord blood).61’5% of the samples were positive for one or more respiratory viruses (63’9% in transplant patients vs 59’8% in non-transplant). 89’4% were positive in nasopharyngeal samples, 4’7% in BAL and 5’9% in both. Causal agents are shown in Table 2. 17% of samples were positive for more than one virus, and 15’4% had microbiologic evidence of infection by a different type of microorganism.30’5% of the infections were considered nosocomial. Concerning those with an infection acquired in the community, 59’6% patients required hospitalization due to the respiratory illness. The symptoms referred by our patients are shown in table 1. 61’4% of the demonstrated viral infections were associated with lymphopenia. Hypogammaglobulinemia was observed in 57%. 30’3% presented comorbidities associated with an increased risk of respiratory infection (underlying heart or lung disease, smoking, HIV positivity, DM or other tumors).Radiologic findings: 50’8% showed a normal X-ray chest image or nonspecific findings, 11’4% pneumonic consolidation and 6’5% signs of atypical infection.42 patients underwent a bronchoscopy. 12 obtained concordant results with nasopharyngeal samples. 10 patients with a negative nasopharyngeal swab had a viral identification in the BAL. We had an isolated case with different results in each sample (a RSV was found in the nasopharyngeal swab and a coronavirus in the BAL). In 8 patients we found other microorganisms (bacteria, fungus).Influenza virus infections were treated with oseltamivir. CMV infections in transplant recipients received immunoglobulins and ganciclovir. 28% of the RSV were treated with immunoglobulins and ribavirin. In most patients the outcome was good. 5 patients died, in 4 of them the respiratory infection was the main cause of death.
Conclusion
Our study confirms that viral respiratory infections are a common cause of morbidity in hematologic patients, even though related mortality was low. The most common symptoms were those of upper airway involvement. 44% of the patients remained afebrile during the course of infection. The presence of other comorbidities, lymphopenia and/or hypogammaglobulinemia seemed to be related with these infections. Although we didn’t find an increased rate of infection in transplant recipient patients, it seems that several microorganisms coinfections are more common in this group. Molecular techniques like PCR have replaced previous diagnostic procedures (like virus cultures), demonstrating a higher sensibility. Given the high rate of nosocomial infections, we would like to highlight the importance of vaccinating staff and family, and isolation measures in patients with suspected respiratory infections transmitted by droplets or contact.
Session topic: E-poster
Keyword(s): Infection
{{ help_message }}
{{filter}}


