ANTIBIOTICS VERSUS G-CSFS VERSUS A COMBINATION OF BOTH TO PREVENT INFECTIOUS COMPLICATIONS AND DEATHS IN CANCER PATIENTS RECEIVING CHEMOTHERAPY: PRELIMINARY RESULTS OF A NETWORK META-ANALYSIS
(Abstract release date: 05/19/16)
EHA Library. Skoetz N. 06/09/16; 132719; E1170

Dr. Nicole Skoetz
Contributions
Contributions
Abstract
Abstract: E1170
Type: Eposter Presentation
Background
Cancer patients receiving chemotherapy are at an increased risk for infectious complications, which represent the most relevant treatment-related causes of death (2 to 21%). The risk of infection is dependent on the duration and intensity of treatment-induced neutropenia and often results in a reduction of the dose of chemotherapy. Uncertainty exists on the achievable degree of infection prevention and whether granulocyte colony stimulating factors (G-CSF), antibiotics or both should be administered.
Aims
The aims of this systematic review and network meta-analysis are to evaluate the benefits and risks of infection prophylaxis with antibiotics, G-CSF, or a combination of both in cancer patients receiving chemotherapy at risk for febrile neutropenia.
Methods
We developed sensitive search strategies for CENTRAL, MEDLINE, and conference proceedings (search date 12/2015).Study selection and data extraction:Randomized controlled trials evaluating infection prophylaxis with antibiotics, G-CSF or both in cancer patients at risk for febrile neutropenia. Only trials were included which clearly stated whether all patients received antibiotics or G-CSF in addition to the evaluated prophylaxis. Two authors independently assessed studies for eligibility, extracted data and assessed quality of trials. The primary outcome was mortality during the study. Secondary outcomes included infection related mortality, severe infection rate, rate of febrile neutropenia and adverse events.Data synthesis:Effect measures were odds ratios (OR). Direct comparisons within trials were combined with indirect evidence by using a Bayesian random-effects model. This project was funded by the Federal Ministry of Education and Research, grant number: 01KG1209.
Results
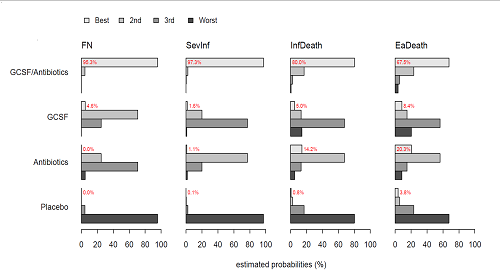
A total of 63 studies were identified, including 11838 patients. Only one study with 40 patients carried out a direct comparison of G-CSF versus antibiotics. Of all studies comparing antibiotics to no antibiotics, only 2 were from 2010 or later.The results of the direct comparisons found an advantage in terms of reduced rate of febrile neutropenia for those trials evaluating G-CSF, both in the studies using G-CSF versus placebo (OR 0.37; 95% CI 0.12 to 0.86) and in those evaluating G-CSF plus antibiotics versus antibiotics alone (OR 0.45; 95% CI 0.24 to 0.74). However, there is no evidence for a difference for the outcomes mortality during the study, infection-related mortality and severe infection rate between the various preventive options. Network meta-analyses show that the combination of G-CSF and antibiotics has the highest probability to be the best for all the observed outcomes (see figure 1). Between-trial heterogeneity was considerable for the outcomes febrile neutropenia and severe infections, potentially due to various definitions (tau 1.08 and 0.97, respectively) and negligible for the other two outcomes (tau 0.42 and 0.18 respectively). The endpoint adverse events was very rarely and inconsistently reported, so no overall statement is possible.
Conclusion
The currently available direct evidence does not show any difference in terms of mortality for the various prophylactic options. The evidence from the network meta-analyses shows an advantage if G-CSF is administered in conjunction with antibiotics compared to placebo, antibiotics or G-CSF alone. Most evidence on antibiotic prophylaxis stems from studies older than 10 years, i.e. before the ongoing pandemic of multi-resistant gram-negatives and vancomycin-resistant enterococci.Further studies with clearly defined inclusion and exclusion criteria (risk of febrile neutropenia) and endpoints (e.g. definition of febrile neutropenia) are necessary in order to properly compare the various prophylactic options and to obtain valid results.
Session topic: E-poster
Keyword(s): Meta-analysis, Systematic review
Type: Eposter Presentation
Background
Cancer patients receiving chemotherapy are at an increased risk for infectious complications, which represent the most relevant treatment-related causes of death (2 to 21%). The risk of infection is dependent on the duration and intensity of treatment-induced neutropenia and often results in a reduction of the dose of chemotherapy. Uncertainty exists on the achievable degree of infection prevention and whether granulocyte colony stimulating factors (G-CSF), antibiotics or both should be administered.
Aims
The aims of this systematic review and network meta-analysis are to evaluate the benefits and risks of infection prophylaxis with antibiotics, G-CSF, or a combination of both in cancer patients receiving chemotherapy at risk for febrile neutropenia.
Methods
We developed sensitive search strategies for CENTRAL, MEDLINE, and conference proceedings (search date 12/2015).Study selection and data extraction:Randomized controlled trials evaluating infection prophylaxis with antibiotics, G-CSF or both in cancer patients at risk for febrile neutropenia. Only trials were included which clearly stated whether all patients received antibiotics or G-CSF in addition to the evaluated prophylaxis. Two authors independently assessed studies for eligibility, extracted data and assessed quality of trials. The primary outcome was mortality during the study. Secondary outcomes included infection related mortality, severe infection rate, rate of febrile neutropenia and adverse events.Data synthesis:Effect measures were odds ratios (OR). Direct comparisons within trials were combined with indirect evidence by using a Bayesian random-effects model. This project was funded by the Federal Ministry of Education and Research, grant number: 01KG1209.
Results
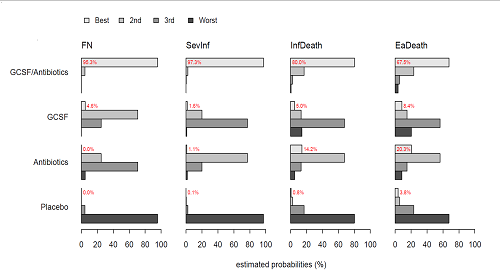
A total of 63 studies were identified, including 11838 patients. Only one study with 40 patients carried out a direct comparison of G-CSF versus antibiotics. Of all studies comparing antibiotics to no antibiotics, only 2 were from 2010 or later.The results of the direct comparisons found an advantage in terms of reduced rate of febrile neutropenia for those trials evaluating G-CSF, both in the studies using G-CSF versus placebo (OR 0.37; 95% CI 0.12 to 0.86) and in those evaluating G-CSF plus antibiotics versus antibiotics alone (OR 0.45; 95% CI 0.24 to 0.74). However, there is no evidence for a difference for the outcomes mortality during the study, infection-related mortality and severe infection rate between the various preventive options. Network meta-analyses show that the combination of G-CSF and antibiotics has the highest probability to be the best for all the observed outcomes (see figure 1). Between-trial heterogeneity was considerable for the outcomes febrile neutropenia and severe infections, potentially due to various definitions (tau 1.08 and 0.97, respectively) and negligible for the other two outcomes (tau 0.42 and 0.18 respectively). The endpoint adverse events was very rarely and inconsistently reported, so no overall statement is possible.
Conclusion
The currently available direct evidence does not show any difference in terms of mortality for the various prophylactic options. The evidence from the network meta-analyses shows an advantage if G-CSF is administered in conjunction with antibiotics compared to placebo, antibiotics or G-CSF alone. Most evidence on antibiotic prophylaxis stems from studies older than 10 years, i.e. before the ongoing pandemic of multi-resistant gram-negatives and vancomycin-resistant enterococci.Further studies with clearly defined inclusion and exclusion criteria (risk of febrile neutropenia) and endpoints (e.g. definition of febrile neutropenia) are necessary in order to properly compare the various prophylactic options and to obtain valid results.
Session topic: E-poster
Keyword(s): Meta-analysis, Systematic review
Abstract: E1170
Type: Eposter Presentation
Background
Cancer patients receiving chemotherapy are at an increased risk for infectious complications, which represent the most relevant treatment-related causes of death (2 to 21%). The risk of infection is dependent on the duration and intensity of treatment-induced neutropenia and often results in a reduction of the dose of chemotherapy. Uncertainty exists on the achievable degree of infection prevention and whether granulocyte colony stimulating factors (G-CSF), antibiotics or both should be administered.
Aims
The aims of this systematic review and network meta-analysis are to evaluate the benefits and risks of infection prophylaxis with antibiotics, G-CSF, or a combination of both in cancer patients receiving chemotherapy at risk for febrile neutropenia.
Methods
We developed sensitive search strategies for CENTRAL, MEDLINE, and conference proceedings (search date 12/2015).Study selection and data extraction:Randomized controlled trials evaluating infection prophylaxis with antibiotics, G-CSF or both in cancer patients at risk for febrile neutropenia. Only trials were included which clearly stated whether all patients received antibiotics or G-CSF in addition to the evaluated prophylaxis. Two authors independently assessed studies for eligibility, extracted data and assessed quality of trials. The primary outcome was mortality during the study. Secondary outcomes included infection related mortality, severe infection rate, rate of febrile neutropenia and adverse events.Data synthesis:Effect measures were odds ratios (OR). Direct comparisons within trials were combined with indirect evidence by using a Bayesian random-effects model. This project was funded by the Federal Ministry of Education and Research, grant number: 01KG1209.
Results
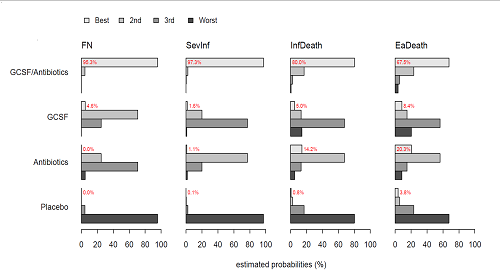
A total of 63 studies were identified, including 11838 patients. Only one study with 40 patients carried out a direct comparison of G-CSF versus antibiotics. Of all studies comparing antibiotics to no antibiotics, only 2 were from 2010 or later.The results of the direct comparisons found an advantage in terms of reduced rate of febrile neutropenia for those trials evaluating G-CSF, both in the studies using G-CSF versus placebo (OR 0.37; 95% CI 0.12 to 0.86) and in those evaluating G-CSF plus antibiotics versus antibiotics alone (OR 0.45; 95% CI 0.24 to 0.74). However, there is no evidence for a difference for the outcomes mortality during the study, infection-related mortality and severe infection rate between the various preventive options. Network meta-analyses show that the combination of G-CSF and antibiotics has the highest probability to be the best for all the observed outcomes (see figure 1). Between-trial heterogeneity was considerable for the outcomes febrile neutropenia and severe infections, potentially due to various definitions (tau 1.08 and 0.97, respectively) and negligible for the other two outcomes (tau 0.42 and 0.18 respectively). The endpoint adverse events was very rarely and inconsistently reported, so no overall statement is possible.
Conclusion
The currently available direct evidence does not show any difference in terms of mortality for the various prophylactic options. The evidence from the network meta-analyses shows an advantage if G-CSF is administered in conjunction with antibiotics compared to placebo, antibiotics or G-CSF alone. Most evidence on antibiotic prophylaxis stems from studies older than 10 years, i.e. before the ongoing pandemic of multi-resistant gram-negatives and vancomycin-resistant enterococci.Further studies with clearly defined inclusion and exclusion criteria (risk of febrile neutropenia) and endpoints (e.g. definition of febrile neutropenia) are necessary in order to properly compare the various prophylactic options and to obtain valid results.
Session topic: E-poster
Keyword(s): Meta-analysis, Systematic review
Type: Eposter Presentation
Background
Cancer patients receiving chemotherapy are at an increased risk for infectious complications, which represent the most relevant treatment-related causes of death (2 to 21%). The risk of infection is dependent on the duration and intensity of treatment-induced neutropenia and often results in a reduction of the dose of chemotherapy. Uncertainty exists on the achievable degree of infection prevention and whether granulocyte colony stimulating factors (G-CSF), antibiotics or both should be administered.
Aims
The aims of this systematic review and network meta-analysis are to evaluate the benefits and risks of infection prophylaxis with antibiotics, G-CSF, or a combination of both in cancer patients receiving chemotherapy at risk for febrile neutropenia.
Methods
We developed sensitive search strategies for CENTRAL, MEDLINE, and conference proceedings (search date 12/2015).Study selection and data extraction:Randomized controlled trials evaluating infection prophylaxis with antibiotics, G-CSF or both in cancer patients at risk for febrile neutropenia. Only trials were included which clearly stated whether all patients received antibiotics or G-CSF in addition to the evaluated prophylaxis. Two authors independently assessed studies for eligibility, extracted data and assessed quality of trials. The primary outcome was mortality during the study. Secondary outcomes included infection related mortality, severe infection rate, rate of febrile neutropenia and adverse events.Data synthesis:Effect measures were odds ratios (OR). Direct comparisons within trials were combined with indirect evidence by using a Bayesian random-effects model. This project was funded by the Federal Ministry of Education and Research, grant number: 01KG1209.
Results
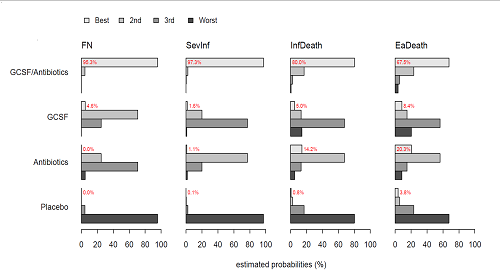
A total of 63 studies were identified, including 11838 patients. Only one study with 40 patients carried out a direct comparison of G-CSF versus antibiotics. Of all studies comparing antibiotics to no antibiotics, only 2 were from 2010 or later.The results of the direct comparisons found an advantage in terms of reduced rate of febrile neutropenia for those trials evaluating G-CSF, both in the studies using G-CSF versus placebo (OR 0.37; 95% CI 0.12 to 0.86) and in those evaluating G-CSF plus antibiotics versus antibiotics alone (OR 0.45; 95% CI 0.24 to 0.74). However, there is no evidence for a difference for the outcomes mortality during the study, infection-related mortality and severe infection rate between the various preventive options. Network meta-analyses show that the combination of G-CSF and antibiotics has the highest probability to be the best for all the observed outcomes (see figure 1). Between-trial heterogeneity was considerable for the outcomes febrile neutropenia and severe infections, potentially due to various definitions (tau 1.08 and 0.97, respectively) and negligible for the other two outcomes (tau 0.42 and 0.18 respectively). The endpoint adverse events was very rarely and inconsistently reported, so no overall statement is possible.
Conclusion
The currently available direct evidence does not show any difference in terms of mortality for the various prophylactic options. The evidence from the network meta-analyses shows an advantage if G-CSF is administered in conjunction with antibiotics compared to placebo, antibiotics or G-CSF alone. Most evidence on antibiotic prophylaxis stems from studies older than 10 years, i.e. before the ongoing pandemic of multi-resistant gram-negatives and vancomycin-resistant enterococci.Further studies with clearly defined inclusion and exclusion criteria (risk of febrile neutropenia) and endpoints (e.g. definition of febrile neutropenia) are necessary in order to properly compare the various prophylactic options and to obtain valid results.
Session topic: E-poster
Keyword(s): Meta-analysis, Systematic review
{{ help_message }}
{{filter}}


