IMPACT OF AZACITIDINE TREATMENT ON INFECTIONS IN PATIENTS WITH ACUTE MYELOID LEUKEMIA, MYELODYSPLASTIC SYNDROMES AND MYELODYSPLASTIC/MYELOPROLIFERATIVE SYNDROMES
(Abstract release date: 05/19/16)
EHA Library. Villegas Da Ros C. 06/09/16; 132716; E1167

Mrs. Carolina Villegas Da Ros
Contributions
Contributions
Abstract
Abstract: E1167
Type: Eposter Presentation
Background
It has been described in previous studies a benefit on infection rate in azacitidine (AZA) treated patients. However, the characteristics of infectious episodes in patients with AZA or best supportive care (BSC) were not described in detail.
Aims
We decided to analyze the impact of AZA treatment on the risk of infection, the characteristics of the infectious episodes and outcome in our patients with acute myeloid leukemia (AML), myelodysplastic syndromes (MDS) and myelodysplastic/myeloproliferative syndromes (SMD/MPS).
Methods
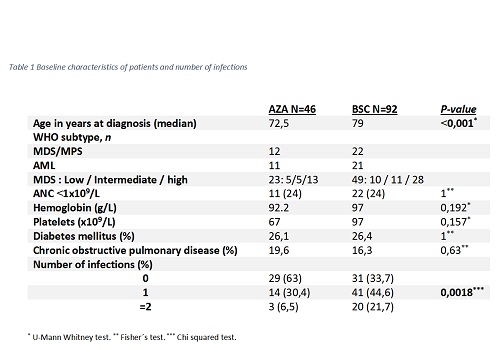
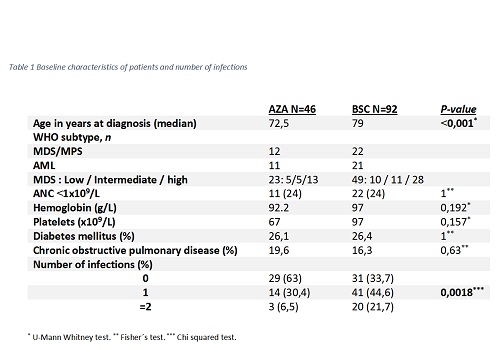
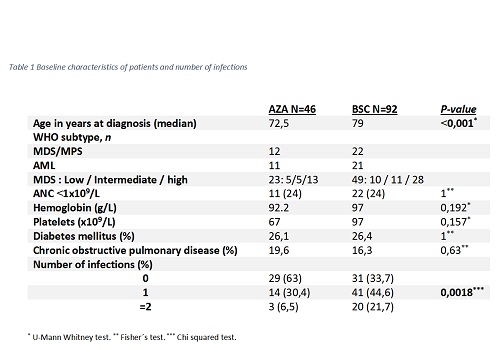
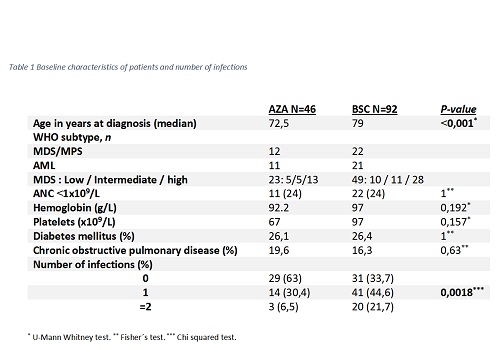
Infections were assessed by reviewing medical records of our department´s database of patients treated with AZA from January 2006 to November 2015. A cohort of matched control patients treated with BSC (two controls for each patient) based on World Health Organization (WHO) subtype, neutrophil count and IPSS-R risk was selected. We took only on account infection´s episodes which required hospitalization.
Results
We included 138 patients, 92 received BSC and 46 treated with AZA at standard schedule (75mg/m2/day 7 days every 28). The median follow up for both groups was 10 months.In the AZA group, 8/46 patients (17.4%) had < 0.5x109/L neutrophils at diagnosis and 6/44 (13.6%) at four months, with no significant increase in neutropenia incidence (p=0.773). However, In the BSC group, 7/92 (7.6%) patients had < 0,5x109/L neutrophils at diagnosis and 16/77 (20.8%) at four months, with a significant increase in the incidence of neutropenia. (p=0.022)The percentage of patients free of infection in AZA group was higher than BSC group. The median of infectious episodes per year was 1.17 in AZA group (CI 95% 0.44-1.90) and 3.08 in BSC group (CI 95% 1.56-4.60) (p=0.004).The days of hospitalization/year due to infection was 20.59 (CI95% 3.91-37.27) in the AZA group and 39.90 (CI 95% 21.63-58.18) in the BSC (p=0.003). The cumulative incidence of first infection, with death as competitive risk, was higher in BSC group than in AZA group; with a cumulative incidence at 12 months of 0.40 (CI 0.26-0.54) and 0.54 (CI 0.43-0.63) in the AZA and BSC group respectively (Grays´s test p=0.0195). In the AZA group 4 (18.2%) episodes were fatal and in the BSC group 24 (23.3%) (P=0.78).Multivariant logistical regression shows that only AZA treatment (HR 0.25 p=0.001 CI 0.12-0.55) and absolute neutrophil count (ANC) >0.5X109/L (HR 0.28 p=0.049 CI 0.08–1.03) showed an independent prognostic value. Age, comorbidities and WHO subtype were excluded by the test.
Conclusion
Azacitidine treated patients had less risk of infection, showed with cumulative incidence, less infectious episodes per year and less days of hospitalization per year. However, the outcome of infection episodes was similar in both groups. The higher incidence of infections in BSC group could be explained by the mayor progression to severe neutropenia.
Session topic: E-poster
Keyword(s): Infection, MDS/AML, Neutropenia, Treatment
Type: Eposter Presentation
Background
It has been described in previous studies a benefit on infection rate in azacitidine (AZA) treated patients. However, the characteristics of infectious episodes in patients with AZA or best supportive care (BSC) were not described in detail.
Aims
We decided to analyze the impact of AZA treatment on the risk of infection, the characteristics of the infectious episodes and outcome in our patients with acute myeloid leukemia (AML), myelodysplastic syndromes (MDS) and myelodysplastic/myeloproliferative syndromes (SMD/MPS).
Methods
Infections were assessed by reviewing medical records of our department´s database of patients treated with AZA from January 2006 to November 2015. A cohort of matched control patients treated with BSC (two controls for each patient) based on World Health Organization (WHO) subtype, neutrophil count and IPSS-R risk was selected. We took only on account infection´s episodes which required hospitalization.
Results
We included 138 patients, 92 received BSC and 46 treated with AZA at standard schedule (75mg/m2/day 7 days every 28). The median follow up for both groups was 10 months.In the AZA group, 8/46 patients (17.4%) had < 0.5x109/L neutrophils at diagnosis and 6/44 (13.6%) at four months, with no significant increase in neutropenia incidence (p=0.773). However, In the BSC group, 7/92 (7.6%) patients had < 0,5x109/L neutrophils at diagnosis and 16/77 (20.8%) at four months, with a significant increase in the incidence of neutropenia. (p=0.022)The percentage of patients free of infection in AZA group was higher than BSC group. The median of infectious episodes per year was 1.17 in AZA group (CI 95% 0.44-1.90) and 3.08 in BSC group (CI 95% 1.56-4.60) (p=0.004).The days of hospitalization/year due to infection was 20.59 (CI95% 3.91-37.27) in the AZA group and 39.90 (CI 95% 21.63-58.18) in the BSC (p=0.003). The cumulative incidence of first infection, with death as competitive risk, was higher in BSC group than in AZA group; with a cumulative incidence at 12 months of 0.40 (CI 0.26-0.54) and 0.54 (CI 0.43-0.63) in the AZA and BSC group respectively (Grays´s test p=0.0195). In the AZA group 4 (18.2%) episodes were fatal and in the BSC group 24 (23.3%) (P=0.78).Multivariant logistical regression shows that only AZA treatment (HR 0.25 p=0.001 CI 0.12-0.55) and absolute neutrophil count (ANC) >0.5X109/L (HR 0.28 p=0.049 CI 0.08–1.03) showed an independent prognostic value. Age, comorbidities and WHO subtype were excluded by the test.
Conclusion
Azacitidine treated patients had less risk of infection, showed with cumulative incidence, less infectious episodes per year and less days of hospitalization per year. However, the outcome of infection episodes was similar in both groups. The higher incidence of infections in BSC group could be explained by the mayor progression to severe neutropenia.
Session topic: E-poster
Keyword(s): Infection, MDS/AML, Neutropenia, Treatment
Abstract: E1167
Type: Eposter Presentation
Background
It has been described in previous studies a benefit on infection rate in azacitidine (AZA) treated patients. However, the characteristics of infectious episodes in patients with AZA or best supportive care (BSC) were not described in detail.
Aims
We decided to analyze the impact of AZA treatment on the risk of infection, the characteristics of the infectious episodes and outcome in our patients with acute myeloid leukemia (AML), myelodysplastic syndromes (MDS) and myelodysplastic/myeloproliferative syndromes (SMD/MPS).
Methods
Infections were assessed by reviewing medical records of our department´s database of patients treated with AZA from January 2006 to November 2015. A cohort of matched control patients treated with BSC (two controls for each patient) based on World Health Organization (WHO) subtype, neutrophil count and IPSS-R risk was selected. We took only on account infection´s episodes which required hospitalization.
Results
We included 138 patients, 92 received BSC and 46 treated with AZA at standard schedule (75mg/m2/day 7 days every 28). The median follow up for both groups was 10 months.In the AZA group, 8/46 patients (17.4%) had < 0.5x109/L neutrophils at diagnosis and 6/44 (13.6%) at four months, with no significant increase in neutropenia incidence (p=0.773). However, In the BSC group, 7/92 (7.6%) patients had < 0,5x109/L neutrophils at diagnosis and 16/77 (20.8%) at four months, with a significant increase in the incidence of neutropenia. (p=0.022)The percentage of patients free of infection in AZA group was higher than BSC group. The median of infectious episodes per year was 1.17 in AZA group (CI 95% 0.44-1.90) and 3.08 in BSC group (CI 95% 1.56-4.60) (p=0.004).The days of hospitalization/year due to infection was 20.59 (CI95% 3.91-37.27) in the AZA group and 39.90 (CI 95% 21.63-58.18) in the BSC (p=0.003). The cumulative incidence of first infection, with death as competitive risk, was higher in BSC group than in AZA group; with a cumulative incidence at 12 months of 0.40 (CI 0.26-0.54) and 0.54 (CI 0.43-0.63) in the AZA and BSC group respectively (Grays´s test p=0.0195). In the AZA group 4 (18.2%) episodes were fatal and in the BSC group 24 (23.3%) (P=0.78).Multivariant logistical regression shows that only AZA treatment (HR 0.25 p=0.001 CI 0.12-0.55) and absolute neutrophil count (ANC) >0.5X109/L (HR 0.28 p=0.049 CI 0.08–1.03) showed an independent prognostic value. Age, comorbidities and WHO subtype were excluded by the test.
Conclusion
Azacitidine treated patients had less risk of infection, showed with cumulative incidence, less infectious episodes per year and less days of hospitalization per year. However, the outcome of infection episodes was similar in both groups. The higher incidence of infections in BSC group could be explained by the mayor progression to severe neutropenia.
Session topic: E-poster
Keyword(s): Infection, MDS/AML, Neutropenia, Treatment
Type: Eposter Presentation
Background
It has been described in previous studies a benefit on infection rate in azacitidine (AZA) treated patients. However, the characteristics of infectious episodes in patients with AZA or best supportive care (BSC) were not described in detail.
Aims
We decided to analyze the impact of AZA treatment on the risk of infection, the characteristics of the infectious episodes and outcome in our patients with acute myeloid leukemia (AML), myelodysplastic syndromes (MDS) and myelodysplastic/myeloproliferative syndromes (SMD/MPS).
Methods
Infections were assessed by reviewing medical records of our department´s database of patients treated with AZA from January 2006 to November 2015. A cohort of matched control patients treated with BSC (two controls for each patient) based on World Health Organization (WHO) subtype, neutrophil count and IPSS-R risk was selected. We took only on account infection´s episodes which required hospitalization.
Results
We included 138 patients, 92 received BSC and 46 treated with AZA at standard schedule (75mg/m2/day 7 days every 28). The median follow up for both groups was 10 months.In the AZA group, 8/46 patients (17.4%) had < 0.5x109/L neutrophils at diagnosis and 6/44 (13.6%) at four months, with no significant increase in neutropenia incidence (p=0.773). However, In the BSC group, 7/92 (7.6%) patients had < 0,5x109/L neutrophils at diagnosis and 16/77 (20.8%) at four months, with a significant increase in the incidence of neutropenia. (p=0.022)The percentage of patients free of infection in AZA group was higher than BSC group. The median of infectious episodes per year was 1.17 in AZA group (CI 95% 0.44-1.90) and 3.08 in BSC group (CI 95% 1.56-4.60) (p=0.004).The days of hospitalization/year due to infection was 20.59 (CI95% 3.91-37.27) in the AZA group and 39.90 (CI 95% 21.63-58.18) in the BSC (p=0.003). The cumulative incidence of first infection, with death as competitive risk, was higher in BSC group than in AZA group; with a cumulative incidence at 12 months of 0.40 (CI 0.26-0.54) and 0.54 (CI 0.43-0.63) in the AZA and BSC group respectively (Grays´s test p=0.0195). In the AZA group 4 (18.2%) episodes were fatal and in the BSC group 24 (23.3%) (P=0.78).Multivariant logistical regression shows that only AZA treatment (HR 0.25 p=0.001 CI 0.12-0.55) and absolute neutrophil count (ANC) >0.5X109/L (HR 0.28 p=0.049 CI 0.08–1.03) showed an independent prognostic value. Age, comorbidities and WHO subtype were excluded by the test.
Conclusion
Azacitidine treated patients had less risk of infection, showed with cumulative incidence, less infectious episodes per year and less days of hospitalization per year. However, the outcome of infection episodes was similar in both groups. The higher incidence of infections in BSC group could be explained by the mayor progression to severe neutropenia.
Session topic: E-poster
Keyword(s): Infection, MDS/AML, Neutropenia, Treatment
{{ help_message }}
{{filter}}


