DISEASE SURVEILLANCE AND LONG-TERM OUTCOME OF PATIENTS WITH MUCOSA-ASSOCIATED LYMPHOID TISSUE (MALT) LYMPHOMA INVOLVING THE STOMACH: A RETROSPECTIVE MULTICENTRE STUDY OF 49 PATIENTS IN FIRST REMISSION
(Abstract release date: 05/19/16)
EHA Library. Nielsen S. 06/09/16; 132713; E1164

Dr. Søren Ramme Nielsen
Contributions
Contributions
Abstract
Abstract: E1164
Type: Eposter Presentation
Background
Gastric MALT lymphoma is a rare subtype of non-Hodgkin lymphoma with an indolent disease course. Treatment options span from simple eradication of Helicobacter Pylori with or without radiotherapy for patients with localized gastric MALT lymphoma to systemic, typically mild chemotherapy regimens and/or rituximab, for patients with non-localized disease. Complete remissions (CR) are often achieved, but relapses occur.
Aims
i) to analyze the relapse patterns and the efficacy of routine gastroscopy for patients with gastric MALT lymphoma in first remission, and ii) report the long-term outcomes of these patients relative to a matched background population.
Methods
We conducted a retrospective study of patients with localized and non-localized gastric MALT lymphoma from six Danish hematology centers between 2000 and 2012. Patients were identified from queries in the Danish Lymphoma registry (LYFO) and consecutive adult patients (>15 years) in CR or CRu were included in the study. Local investigators reviewed medical records and collected information regarding gastroscopic examinations, relapse (including relapse detection method and relapse histology), and cause of death. Gastroscopies were categorized as routine if prescribed to a patient in clinical remissions and clinical if prescribed to a patient with relapse suspicious symptoms/findings. Data collection was compliant with national regulations.
Results
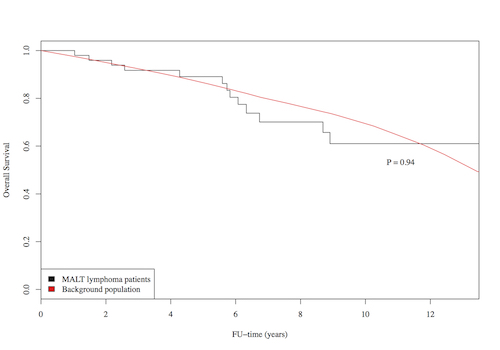
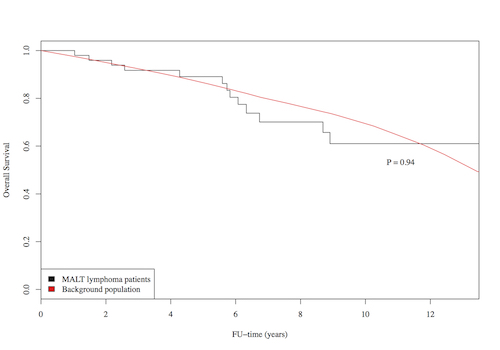
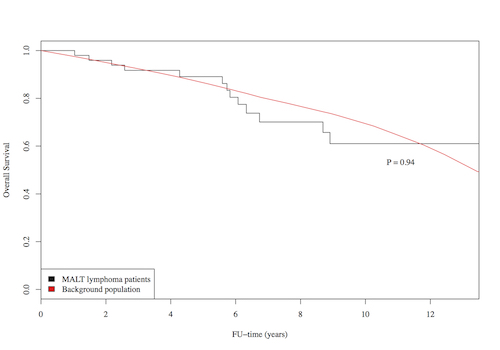
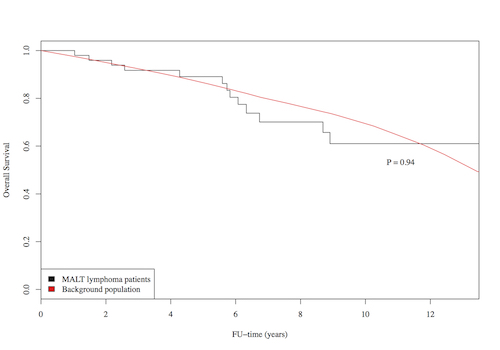
In total, 49 patients with gastric MALT lymphomas stage I-IV and in CR or CRu following first line treatment were included. Median age was 64 years (range 25-87) and male:female ratio was 1.1. During a median FU of 88.8 months, seven patients relapsed and 14 patients died. The five-year PFS and OS estimates were 73% (95% CI 61-88) and 89% (95% CI 80-99), respectively (Figure 1). The OS of a matched background population was not different from the MALT lymphoma (P=0.94, standardized mortality ratio, Figure 1). During follow-up, the 49 patients received 100 routine endoscopies (mean 2 range 0-6) and 15 clinical endoscopies. In four patients (8%), routine gastroscopy detected preclinical MALT relapse or another cancer at an asymptomatic stage (adenocarcinoma). Thus, 4/100 routine endoscopies (4%, 95% CI 1-10%) contributed significantly to detection of relapse or other malignancy. These findings resulted in chemotherapy for 2/4, helicobacter eradication with antibiotics for 1/4 and surgery for 1/4 (adenocarcinoma). A single MALT lymphoma relapse was detected as a result of patient reported symptoms. Thus, 1/15 (7%, 95% CI 0-32%) of the gastroscopies performed in response to clinical symptoms/findings confirmed relapse. A case of adenocarcinoma localized in the stomach was found 28 months after first MALT lymphoma diagnosis, but transformation to high-grade lymphoma was not reported for any patients. Of note, no deaths were related to progressive MALT lymphoma in this cohort of 49 patients.
Conclusion
This study confirms the very indolent nature of gastric MALT lymphoma with survival not statistically significantly different from the background population. Preclinical relapse detection has not been shown to improve outcome in gastric MALT lymphoma and asymptomatic relapse can be managed with a watch-and-wait strategy in selected patients. In this context, the yield of routine endoscopy is limited. However, one case of adenocarcinoma was detected at an early stage by routine endoscopy.
Session topic: E-poster
Keyword(s): Follow-up, MALT lymphoma, Survival
Type: Eposter Presentation
Background
Gastric MALT lymphoma is a rare subtype of non-Hodgkin lymphoma with an indolent disease course. Treatment options span from simple eradication of Helicobacter Pylori with or without radiotherapy for patients with localized gastric MALT lymphoma to systemic, typically mild chemotherapy regimens and/or rituximab, for patients with non-localized disease. Complete remissions (CR) are often achieved, but relapses occur.
Aims
i) to analyze the relapse patterns and the efficacy of routine gastroscopy for patients with gastric MALT lymphoma in first remission, and ii) report the long-term outcomes of these patients relative to a matched background population.
Methods
We conducted a retrospective study of patients with localized and non-localized gastric MALT lymphoma from six Danish hematology centers between 2000 and 2012. Patients were identified from queries in the Danish Lymphoma registry (LYFO) and consecutive adult patients (>15 years) in CR or CRu were included in the study. Local investigators reviewed medical records and collected information regarding gastroscopic examinations, relapse (including relapse detection method and relapse histology), and cause of death. Gastroscopies were categorized as routine if prescribed to a patient in clinical remissions and clinical if prescribed to a patient with relapse suspicious symptoms/findings. Data collection was compliant with national regulations.
Results
In total, 49 patients with gastric MALT lymphomas stage I-IV and in CR or CRu following first line treatment were included. Median age was 64 years (range 25-87) and male:female ratio was 1.1. During a median FU of 88.8 months, seven patients relapsed and 14 patients died. The five-year PFS and OS estimates were 73% (95% CI 61-88) and 89% (95% CI 80-99), respectively (Figure 1). The OS of a matched background population was not different from the MALT lymphoma (P=0.94, standardized mortality ratio, Figure 1). During follow-up, the 49 patients received 100 routine endoscopies (mean 2 range 0-6) and 15 clinical endoscopies. In four patients (8%), routine gastroscopy detected preclinical MALT relapse or another cancer at an asymptomatic stage (adenocarcinoma). Thus, 4/100 routine endoscopies (4%, 95% CI 1-10%) contributed significantly to detection of relapse or other malignancy. These findings resulted in chemotherapy for 2/4, helicobacter eradication with antibiotics for 1/4 and surgery for 1/4 (adenocarcinoma). A single MALT lymphoma relapse was detected as a result of patient reported symptoms. Thus, 1/15 (7%, 95% CI 0-32%) of the gastroscopies performed in response to clinical symptoms/findings confirmed relapse. A case of adenocarcinoma localized in the stomach was found 28 months after first MALT lymphoma diagnosis, but transformation to high-grade lymphoma was not reported for any patients. Of note, no deaths were related to progressive MALT lymphoma in this cohort of 49 patients.
Conclusion
This study confirms the very indolent nature of gastric MALT lymphoma with survival not statistically significantly different from the background population. Preclinical relapse detection has not been shown to improve outcome in gastric MALT lymphoma and asymptomatic relapse can be managed with a watch-and-wait strategy in selected patients. In this context, the yield of routine endoscopy is limited. However, one case of adenocarcinoma was detected at an early stage by routine endoscopy.
Session topic: E-poster
Keyword(s): Follow-up, MALT lymphoma, Survival
Abstract: E1164
Type: Eposter Presentation
Background
Gastric MALT lymphoma is a rare subtype of non-Hodgkin lymphoma with an indolent disease course. Treatment options span from simple eradication of Helicobacter Pylori with or without radiotherapy for patients with localized gastric MALT lymphoma to systemic, typically mild chemotherapy regimens and/or rituximab, for patients with non-localized disease. Complete remissions (CR) are often achieved, but relapses occur.
Aims
i) to analyze the relapse patterns and the efficacy of routine gastroscopy for patients with gastric MALT lymphoma in first remission, and ii) report the long-term outcomes of these patients relative to a matched background population.
Methods
We conducted a retrospective study of patients with localized and non-localized gastric MALT lymphoma from six Danish hematology centers between 2000 and 2012. Patients were identified from queries in the Danish Lymphoma registry (LYFO) and consecutive adult patients (>15 years) in CR or CRu were included in the study. Local investigators reviewed medical records and collected information regarding gastroscopic examinations, relapse (including relapse detection method and relapse histology), and cause of death. Gastroscopies were categorized as routine if prescribed to a patient in clinical remissions and clinical if prescribed to a patient with relapse suspicious symptoms/findings. Data collection was compliant with national regulations.
Results
In total, 49 patients with gastric MALT lymphomas stage I-IV and in CR or CRu following first line treatment were included. Median age was 64 years (range 25-87) and male:female ratio was 1.1. During a median FU of 88.8 months, seven patients relapsed and 14 patients died. The five-year PFS and OS estimates were 73% (95% CI 61-88) and 89% (95% CI 80-99), respectively (Figure 1). The OS of a matched background population was not different from the MALT lymphoma (P=0.94, standardized mortality ratio, Figure 1). During follow-up, the 49 patients received 100 routine endoscopies (mean 2 range 0-6) and 15 clinical endoscopies. In four patients (8%), routine gastroscopy detected preclinical MALT relapse or another cancer at an asymptomatic stage (adenocarcinoma). Thus, 4/100 routine endoscopies (4%, 95% CI 1-10%) contributed significantly to detection of relapse or other malignancy. These findings resulted in chemotherapy for 2/4, helicobacter eradication with antibiotics for 1/4 and surgery for 1/4 (adenocarcinoma). A single MALT lymphoma relapse was detected as a result of patient reported symptoms. Thus, 1/15 (7%, 95% CI 0-32%) of the gastroscopies performed in response to clinical symptoms/findings confirmed relapse. A case of adenocarcinoma localized in the stomach was found 28 months after first MALT lymphoma diagnosis, but transformation to high-grade lymphoma was not reported for any patients. Of note, no deaths were related to progressive MALT lymphoma in this cohort of 49 patients.
Conclusion
This study confirms the very indolent nature of gastric MALT lymphoma with survival not statistically significantly different from the background population. Preclinical relapse detection has not been shown to improve outcome in gastric MALT lymphoma and asymptomatic relapse can be managed with a watch-and-wait strategy in selected patients. In this context, the yield of routine endoscopy is limited. However, one case of adenocarcinoma was detected at an early stage by routine endoscopy.
Session topic: E-poster
Keyword(s): Follow-up, MALT lymphoma, Survival
Type: Eposter Presentation
Background
Gastric MALT lymphoma is a rare subtype of non-Hodgkin lymphoma with an indolent disease course. Treatment options span from simple eradication of Helicobacter Pylori with or without radiotherapy for patients with localized gastric MALT lymphoma to systemic, typically mild chemotherapy regimens and/or rituximab, for patients with non-localized disease. Complete remissions (CR) are often achieved, but relapses occur.
Aims
i) to analyze the relapse patterns and the efficacy of routine gastroscopy for patients with gastric MALT lymphoma in first remission, and ii) report the long-term outcomes of these patients relative to a matched background population.
Methods
We conducted a retrospective study of patients with localized and non-localized gastric MALT lymphoma from six Danish hematology centers between 2000 and 2012. Patients were identified from queries in the Danish Lymphoma registry (LYFO) and consecutive adult patients (>15 years) in CR or CRu were included in the study. Local investigators reviewed medical records and collected information regarding gastroscopic examinations, relapse (including relapse detection method and relapse histology), and cause of death. Gastroscopies were categorized as routine if prescribed to a patient in clinical remissions and clinical if prescribed to a patient with relapse suspicious symptoms/findings. Data collection was compliant with national regulations.
Results
In total, 49 patients with gastric MALT lymphomas stage I-IV and in CR or CRu following first line treatment were included. Median age was 64 years (range 25-87) and male:female ratio was 1.1. During a median FU of 88.8 months, seven patients relapsed and 14 patients died. The five-year PFS and OS estimates were 73% (95% CI 61-88) and 89% (95% CI 80-99), respectively (Figure 1). The OS of a matched background population was not different from the MALT lymphoma (P=0.94, standardized mortality ratio, Figure 1). During follow-up, the 49 patients received 100 routine endoscopies (mean 2 range 0-6) and 15 clinical endoscopies. In four patients (8%), routine gastroscopy detected preclinical MALT relapse or another cancer at an asymptomatic stage (adenocarcinoma). Thus, 4/100 routine endoscopies (4%, 95% CI 1-10%) contributed significantly to detection of relapse or other malignancy. These findings resulted in chemotherapy for 2/4, helicobacter eradication with antibiotics for 1/4 and surgery for 1/4 (adenocarcinoma). A single MALT lymphoma relapse was detected as a result of patient reported symptoms. Thus, 1/15 (7%, 95% CI 0-32%) of the gastroscopies performed in response to clinical symptoms/findings confirmed relapse. A case of adenocarcinoma localized in the stomach was found 28 months after first MALT lymphoma diagnosis, but transformation to high-grade lymphoma was not reported for any patients. Of note, no deaths were related to progressive MALT lymphoma in this cohort of 49 patients.
Conclusion
This study confirms the very indolent nature of gastric MALT lymphoma with survival not statistically significantly different from the background population. Preclinical relapse detection has not been shown to improve outcome in gastric MALT lymphoma and asymptomatic relapse can be managed with a watch-and-wait strategy in selected patients. In this context, the yield of routine endoscopy is limited. However, one case of adenocarcinoma was detected at an early stage by routine endoscopy.
Session topic: E-poster
Keyword(s): Follow-up, MALT lymphoma, Survival
{{ help_message }}
{{filter}}


