VERY YOUNG PATIENTS WITH CHRONIC LYMPHOCYTIC LEUKEMIA HAVE LOWER INCIDENCE OF ADVERSE CYTOGENETICS AND IMPROVED OVERALL SURVIVAL: 10-YEAR EXPERIENCE FROM MEMORIAL SLOAN KETTERING CANCER CENTER.
(Abstract release date: 05/19/16)
EHA Library. Getta B. 06/09/16; 132606; E1057

Dr. Bartlomiej Getta
Contributions
Contributions
Abstract
Abstract: E1057
Type: Eposter Presentation
Background
Young pts, arbitrarily defined as ≤ age 40, comprise a very small fraction of patients with CLL. Risk factors and outcomes in this young age group are not well described.
Aims
To compare biologic disease factors and clinical outcomes between patients age ≤40 with those > 40.
Methods
Young pts were arbitrarily defined as ≤40 at diagnosis. Pts from the MSKCC CLL database diagnosed between 1/1/2005 and12/31/2015 were included. Two control CLL pts age >40 were matched to each patient≤40 and served as controls. Matching was based on diagnosis year (+/- 2 yrs) and the time from diagnosis to the first MSKCC visit (+/- 2yrs). Patient and disease characteristics were compared using Fisher’s exact test. Cox regression analysis accounting for the matched pairs was used to estimate overall survival, time-to-first and –second treatment, and duration of first response. Survivor curves were estimated using Kaplan-Meier methods. The National Cancer Institute Surveillance, Epidemiology and End Results (SEER) database was used to compare the overall survival of pts ≤40 years with those >40 diagnosed between 1990-2005. Statistical analysis was performed using the R statistical package. The project was approved by the MSKCC institutional review board.
Results
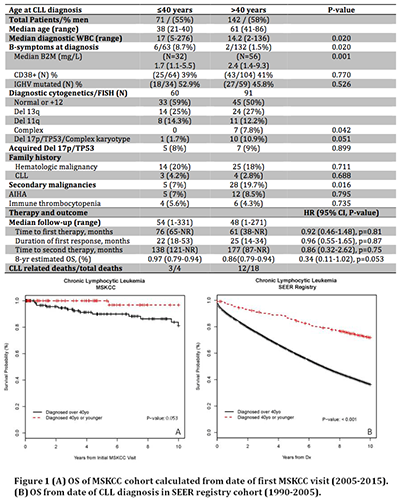
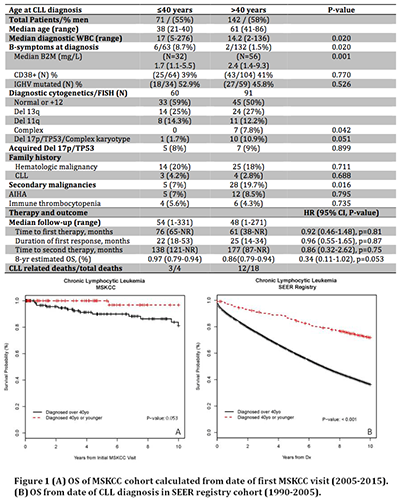
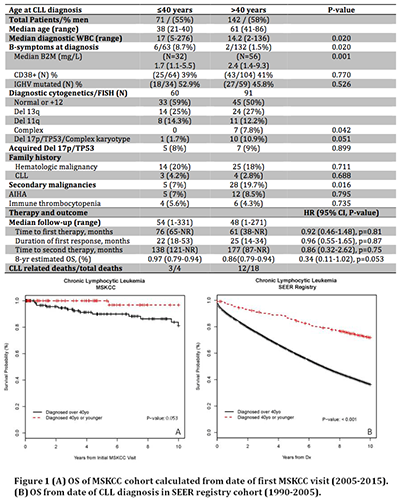
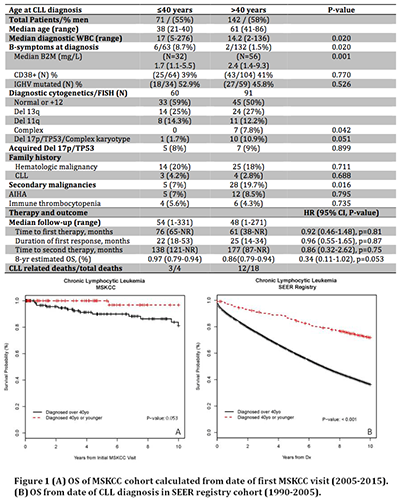
71/3455 (2.1%) pts in the MSKCC database were < age 40. Characteristics of the two groups are shown in Table 1. Significant differences included: initial WBC, presence of B symptoms, B2M and adverse cytogenetics. Second malignancies occurred more frequently in pts >40. There were 6 cases of Richter’s transformation (RT) to DLBCL in each group, one case of histologically ‘accelerated CLL’ in each group and two cases of transformation to Hodgkin lymphoma in the group >40. DLBCL with TP53 mutation/del17p was seen in 1/6 pts ≤40 and 3/6 in >40 group. DLBCL was the initial indication for CLL therapy in 5/6 young pts who had RT, 3 of whom presented concurrently with CLL and RT. No pt >age 40 presented with CLL and DLBCL. There was no difference in the incidence of autoimmune complications in the two groups and no difference in the incidence of hematologic or solid organ malignancy in 1st or 2nd degree family members.The median follow-up of the MSKCC pts ≤40 was 54 months (1-313) and those >40 was 48 months (0-271). 48% of pts in each group required treatment. The time to first therapy and duration of response following 1st and 2nd line therapy were similar (Table 1). Six pts ≤40 (8.5%) and 2 pts >40 (1.4%) underwent allo-BMT (p=0.018). There were 4 deaths in pts ≤40 (5.6%) and 18 deaths in pts >40 (12.7%). Seven of the 22 deaths were unrelated to CLL (Table 1); and 6 of these were due to secondary malignancies. The estimated OS at 8 years was 0.97% in the group <40 and 86% in the group >40 (p=0.053) (Fig 1A). Lastly, in order to compare our results with a larger database, we evaluated young pts in the SEER database. There were 29,822 CLL pts of whom 279 were ≤40 (0.94%). The median OS in SEER cohort for pts age ≤40 was not reached, and in those age>40 was 6.9 years (95% CI 6.8-7.0),(p<0.001) (Fig 1B).
Conclusion
A very small fraction of pts with CLL are diagnosed before the age of 40. These data suggest: a lower incidence of adverse cytogenetics at diagnosis, equivalent treatment response, and a higher incidence of RT that was not associated with del17p. MSKCC and SEER data suggest that young pts with CLL do not have an inferior survival compared pts >age 40.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Outcome, Young adult
Type: Eposter Presentation
Background
Young pts, arbitrarily defined as ≤ age 40, comprise a very small fraction of patients with CLL. Risk factors and outcomes in this young age group are not well described.
Aims
To compare biologic disease factors and clinical outcomes between patients age ≤40 with those > 40.
Methods
Young pts were arbitrarily defined as ≤40 at diagnosis. Pts from the MSKCC CLL database diagnosed between 1/1/2005 and12/31/2015 were included. Two control CLL pts age >40 were matched to each patient≤40 and served as controls. Matching was based on diagnosis year (+/- 2 yrs) and the time from diagnosis to the first MSKCC visit (+/- 2yrs). Patient and disease characteristics were compared using Fisher’s exact test. Cox regression analysis accounting for the matched pairs was used to estimate overall survival, time-to-first and –second treatment, and duration of first response. Survivor curves were estimated using Kaplan-Meier methods. The National Cancer Institute Surveillance, Epidemiology and End Results (SEER) database was used to compare the overall survival of pts ≤40 years with those >40 diagnosed between 1990-2005. Statistical analysis was performed using the R statistical package. The project was approved by the MSKCC institutional review board.
Results
71/3455 (2.1%) pts in the MSKCC database were < age 40. Characteristics of the two groups are shown in Table 1. Significant differences included: initial WBC, presence of B symptoms, B2M and adverse cytogenetics. Second malignancies occurred more frequently in pts >40. There were 6 cases of Richter’s transformation (RT) to DLBCL in each group, one case of histologically ‘accelerated CLL’ in each group and two cases of transformation to Hodgkin lymphoma in the group >40. DLBCL with TP53 mutation/del17p was seen in 1/6 pts ≤40 and 3/6 in >40 group. DLBCL was the initial indication for CLL therapy in 5/6 young pts who had RT, 3 of whom presented concurrently with CLL and RT. No pt >age 40 presented with CLL and DLBCL. There was no difference in the incidence of autoimmune complications in the two groups and no difference in the incidence of hematologic or solid organ malignancy in 1st or 2nd degree family members.The median follow-up of the MSKCC pts ≤40 was 54 months (1-313) and those >40 was 48 months (0-271). 48% of pts in each group required treatment. The time to first therapy and duration of response following 1st and 2nd line therapy were similar (Table 1). Six pts ≤40 (8.5%) and 2 pts >40 (1.4%) underwent allo-BMT (p=0.018). There were 4 deaths in pts ≤40 (5.6%) and 18 deaths in pts >40 (12.7%). Seven of the 22 deaths were unrelated to CLL (Table 1); and 6 of these were due to secondary malignancies. The estimated OS at 8 years was 0.97% in the group <40 and 86% in the group >40 (p=0.053) (Fig 1A). Lastly, in order to compare our results with a larger database, we evaluated young pts in the SEER database. There were 29,822 CLL pts of whom 279 were ≤40 (0.94%). The median OS in SEER cohort for pts age ≤40 was not reached, and in those age>40 was 6.9 years (95% CI 6.8-7.0),(p<0.001) (Fig 1B).
Conclusion
A very small fraction of pts with CLL are diagnosed before the age of 40. These data suggest: a lower incidence of adverse cytogenetics at diagnosis, equivalent treatment response, and a higher incidence of RT that was not associated with del17p. MSKCC and SEER data suggest that young pts with CLL do not have an inferior survival compared pts >age 40.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Outcome, Young adult
Abstract: E1057
Type: Eposter Presentation
Background
Young pts, arbitrarily defined as ≤ age 40, comprise a very small fraction of patients with CLL. Risk factors and outcomes in this young age group are not well described.
Aims
To compare biologic disease factors and clinical outcomes between patients age ≤40 with those > 40.
Methods
Young pts were arbitrarily defined as ≤40 at diagnosis. Pts from the MSKCC CLL database diagnosed between 1/1/2005 and12/31/2015 were included. Two control CLL pts age >40 were matched to each patient≤40 and served as controls. Matching was based on diagnosis year (+/- 2 yrs) and the time from diagnosis to the first MSKCC visit (+/- 2yrs). Patient and disease characteristics were compared using Fisher’s exact test. Cox regression analysis accounting for the matched pairs was used to estimate overall survival, time-to-first and –second treatment, and duration of first response. Survivor curves were estimated using Kaplan-Meier methods. The National Cancer Institute Surveillance, Epidemiology and End Results (SEER) database was used to compare the overall survival of pts ≤40 years with those >40 diagnosed between 1990-2005. Statistical analysis was performed using the R statistical package. The project was approved by the MSKCC institutional review board.
Results
71/3455 (2.1%) pts in the MSKCC database were < age 40. Characteristics of the two groups are shown in Table 1. Significant differences included: initial WBC, presence of B symptoms, B2M and adverse cytogenetics. Second malignancies occurred more frequently in pts >40. There were 6 cases of Richter’s transformation (RT) to DLBCL in each group, one case of histologically ‘accelerated CLL’ in each group and two cases of transformation to Hodgkin lymphoma in the group >40. DLBCL with TP53 mutation/del17p was seen in 1/6 pts ≤40 and 3/6 in >40 group. DLBCL was the initial indication for CLL therapy in 5/6 young pts who had RT, 3 of whom presented concurrently with CLL and RT. No pt >age 40 presented with CLL and DLBCL. There was no difference in the incidence of autoimmune complications in the two groups and no difference in the incidence of hematologic or solid organ malignancy in 1st or 2nd degree family members.The median follow-up of the MSKCC pts ≤40 was 54 months (1-313) and those >40 was 48 months (0-271). 48% of pts in each group required treatment. The time to first therapy and duration of response following 1st and 2nd line therapy were similar (Table 1). Six pts ≤40 (8.5%) and 2 pts >40 (1.4%) underwent allo-BMT (p=0.018). There were 4 deaths in pts ≤40 (5.6%) and 18 deaths in pts >40 (12.7%). Seven of the 22 deaths were unrelated to CLL (Table 1); and 6 of these were due to secondary malignancies. The estimated OS at 8 years was 0.97% in the group <40 and 86% in the group >40 (p=0.053) (Fig 1A). Lastly, in order to compare our results with a larger database, we evaluated young pts in the SEER database. There were 29,822 CLL pts of whom 279 were ≤40 (0.94%). The median OS in SEER cohort for pts age ≤40 was not reached, and in those age>40 was 6.9 years (95% CI 6.8-7.0),(p<0.001) (Fig 1B).
Conclusion
A very small fraction of pts with CLL are diagnosed before the age of 40. These data suggest: a lower incidence of adverse cytogenetics at diagnosis, equivalent treatment response, and a higher incidence of RT that was not associated with del17p. MSKCC and SEER data suggest that young pts with CLL do not have an inferior survival compared pts >age 40.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Outcome, Young adult
Type: Eposter Presentation
Background
Young pts, arbitrarily defined as ≤ age 40, comprise a very small fraction of patients with CLL. Risk factors and outcomes in this young age group are not well described.
Aims
To compare biologic disease factors and clinical outcomes between patients age ≤40 with those > 40.
Methods
Young pts were arbitrarily defined as ≤40 at diagnosis. Pts from the MSKCC CLL database diagnosed between 1/1/2005 and12/31/2015 were included. Two control CLL pts age >40 were matched to each patient≤40 and served as controls. Matching was based on diagnosis year (+/- 2 yrs) and the time from diagnosis to the first MSKCC visit (+/- 2yrs). Patient and disease characteristics were compared using Fisher’s exact test. Cox regression analysis accounting for the matched pairs was used to estimate overall survival, time-to-first and –second treatment, and duration of first response. Survivor curves were estimated using Kaplan-Meier methods. The National Cancer Institute Surveillance, Epidemiology and End Results (SEER) database was used to compare the overall survival of pts ≤40 years with those >40 diagnosed between 1990-2005. Statistical analysis was performed using the R statistical package. The project was approved by the MSKCC institutional review board.
Results
71/3455 (2.1%) pts in the MSKCC database were < age 40. Characteristics of the two groups are shown in Table 1. Significant differences included: initial WBC, presence of B symptoms, B2M and adverse cytogenetics. Second malignancies occurred more frequently in pts >40. There were 6 cases of Richter’s transformation (RT) to DLBCL in each group, one case of histologically ‘accelerated CLL’ in each group and two cases of transformation to Hodgkin lymphoma in the group >40. DLBCL with TP53 mutation/del17p was seen in 1/6 pts ≤40 and 3/6 in >40 group. DLBCL was the initial indication for CLL therapy in 5/6 young pts who had RT, 3 of whom presented concurrently with CLL and RT. No pt >age 40 presented with CLL and DLBCL. There was no difference in the incidence of autoimmune complications in the two groups and no difference in the incidence of hematologic or solid organ malignancy in 1st or 2nd degree family members.The median follow-up of the MSKCC pts ≤40 was 54 months (1-313) and those >40 was 48 months (0-271). 48% of pts in each group required treatment. The time to first therapy and duration of response following 1st and 2nd line therapy were similar (Table 1). Six pts ≤40 (8.5%) and 2 pts >40 (1.4%) underwent allo-BMT (p=0.018). There were 4 deaths in pts ≤40 (5.6%) and 18 deaths in pts >40 (12.7%). Seven of the 22 deaths were unrelated to CLL (Table 1); and 6 of these were due to secondary malignancies. The estimated OS at 8 years was 0.97% in the group <40 and 86% in the group >40 (p=0.053) (Fig 1A). Lastly, in order to compare our results with a larger database, we evaluated young pts in the SEER database. There were 29,822 CLL pts of whom 279 were ≤40 (0.94%). The median OS in SEER cohort for pts age ≤40 was not reached, and in those age>40 was 6.9 years (95% CI 6.8-7.0),(p<0.001) (Fig 1B).
Conclusion
A very small fraction of pts with CLL are diagnosed before the age of 40. These data suggest: a lower incidence of adverse cytogenetics at diagnosis, equivalent treatment response, and a higher incidence of RT that was not associated with del17p. MSKCC and SEER data suggest that young pts with CLL do not have an inferior survival compared pts >age 40.
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Outcome, Young adult
{{ help_message }}
{{filter}}


