ASSESSING TIME TO FIRST TREATMENT IN EARLY CLL: A COMPARATIVE PERFORMANCE ANALYSIS OF FIVE PROGNOSTIC MODELS WITH INCLUSION OF CLL-IPI.
(Abstract release date: 05/19/16)
EHA Library. molica s. 06/09/16; 132604; E1055

Dr. stefano molica
Contributions
Contributions
Abstract
Abstract: E1055
Type: Eposter Presentation
Background
Recent research in CLL focused on the development of prognostic scores which assemble in a same model different prognostic markers. However, analyses comparing the performances of these models are lacking.
Aims
In a prospective patient cohort we evaluated the capability of four recently proposed prognostic models in CLL (i.e., 2007 MDACC score, GCLLSG score, 2011 MDACC score,O-CLL1 score) to predict time to first treatment (TTFT). Results were compared with those obtained using the CLL-IPI.
Methods
Newly diagnosed Binet stage A patients (n=337) from several Italian Institutions prospectively enrolled into the O-CLL1 protocol (clinicaltrial.gov identifier: 115 NCT00917540) form the basis of this analysis.
Results
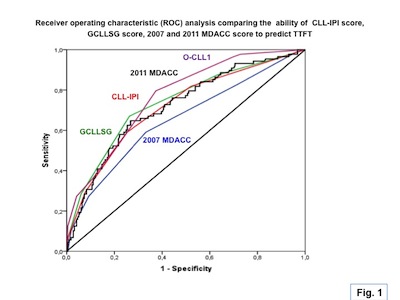
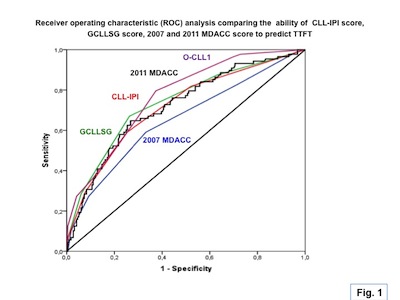
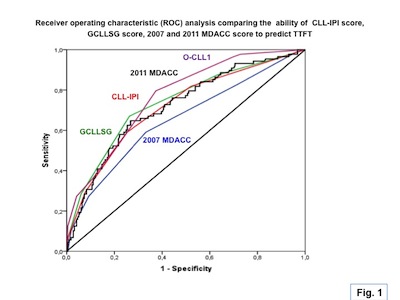
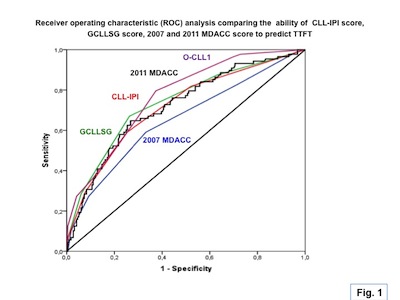
The Harrell’s c values which indicate the discriminatory power of the models (higher is better) were better for 2011 MDACC score (c-index, 0.71) and the O-CLL1 score (c-index,0.75) which were generated looking at TTFT as endpoint and combine clinical, biological and genetic markers. The same applied with GCLLSG (c-index,0.70) score and CLL-IPI (c-index, 0.70) even though they were originally developed with overall survival as main end pont. Finally, a c-statistic below 0.70 which is the threshold necessary to have value at the individual patient level was observed with 2007 MDACC score (c-index, 0.65) which was designed to assess overall survival as end point and did not incorporate major genetic factors. A global view of performances of different scores was also provided by the area under the receiver operating characteristic (ROC) curve figures considered an alternative measure of discrimination ( Figure 1). Furthermore, the time-dependent ROC analysis which is an extension of ROC curves demonstrated that for early time points (< 24 months) scores provided limited ability in distinguishing patients with different TTFT. In contrast, for late time points (≥ 24 months after diagnosis), the predictive accuracy of TTFT was higher for models including both clinical and genetic variables (i.e., O-CLL1, CLL-IPI,2011 MDACC score, GCLLSG score) in comparison with models which included only clinical variables (i.e., 2007 MDACC score). Finally, values of Aikaike information criterion (AIC) which indicates the goodness of the fit (lower is better) were better for the O-CLL1 score (AIC, 810) and worse for 2007 MDACC score (AIC, 851). In between there were the GCLLSG score (AIC, 837), the CLL-IPI (AIC, 841) and the 2011 MDACC score (AIC, 844), respectively .
Conclusion
Although different with respect to either the endpoints for which they were generated (i.e., OS versus TTFT) or the prognostic factors considered (i.e., only clinical versus clinical and genetic) all models used in this validation analysis worked in predicting TTFT. Results of AIC and Harrell’s c value demonstrated that the predictive accuracy of TTFT was higher for models including both clinical and genetic variables (i.e., CLL-01, CLL-IPI,2011 MDACC score, GCLLSG score).
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Prognosis
Type: Eposter Presentation
Background
Recent research in CLL focused on the development of prognostic scores which assemble in a same model different prognostic markers. However, analyses comparing the performances of these models are lacking.
Aims
In a prospective patient cohort we evaluated the capability of four recently proposed prognostic models in CLL (i.e., 2007 MDACC score, GCLLSG score, 2011 MDACC score,O-CLL1 score) to predict time to first treatment (TTFT). Results were compared with those obtained using the CLL-IPI.
Methods
Newly diagnosed Binet stage A patients (n=337) from several Italian Institutions prospectively enrolled into the O-CLL1 protocol (clinicaltrial.gov identifier: 115 NCT00917540) form the basis of this analysis.
Results
The Harrell’s c values which indicate the discriminatory power of the models (higher is better) were better for 2011 MDACC score (c-index, 0.71) and the O-CLL1 score (c-index,0.75) which were generated looking at TTFT as endpoint and combine clinical, biological and genetic markers. The same applied with GCLLSG (c-index,0.70) score and CLL-IPI (c-index, 0.70) even though they were originally developed with overall survival as main end pont. Finally, a c-statistic below 0.70 which is the threshold necessary to have value at the individual patient level was observed with 2007 MDACC score (c-index, 0.65) which was designed to assess overall survival as end point and did not incorporate major genetic factors. A global view of performances of different scores was also provided by the area under the receiver operating characteristic (ROC) curve figures considered an alternative measure of discrimination ( Figure 1). Furthermore, the time-dependent ROC analysis which is an extension of ROC curves demonstrated that for early time points (< 24 months) scores provided limited ability in distinguishing patients with different TTFT. In contrast, for late time points (≥ 24 months after diagnosis), the predictive accuracy of TTFT was higher for models including both clinical and genetic variables (i.e., O-CLL1, CLL-IPI,2011 MDACC score, GCLLSG score) in comparison with models which included only clinical variables (i.e., 2007 MDACC score). Finally, values of Aikaike information criterion (AIC) which indicates the goodness of the fit (lower is better) were better for the O-CLL1 score (AIC, 810) and worse for 2007 MDACC score (AIC, 851). In between there were the GCLLSG score (AIC, 837), the CLL-IPI (AIC, 841) and the 2011 MDACC score (AIC, 844), respectively .
Conclusion
Although different with respect to either the endpoints for which they were generated (i.e., OS versus TTFT) or the prognostic factors considered (i.e., only clinical versus clinical and genetic) all models used in this validation analysis worked in predicting TTFT. Results of AIC and Harrell’s c value demonstrated that the predictive accuracy of TTFT was higher for models including both clinical and genetic variables (i.e., CLL-01, CLL-IPI,2011 MDACC score, GCLLSG score).
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Prognosis
Abstract: E1055
Type: Eposter Presentation
Background
Recent research in CLL focused on the development of prognostic scores which assemble in a same model different prognostic markers. However, analyses comparing the performances of these models are lacking.
Aims
In a prospective patient cohort we evaluated the capability of four recently proposed prognostic models in CLL (i.e., 2007 MDACC score, GCLLSG score, 2011 MDACC score,O-CLL1 score) to predict time to first treatment (TTFT). Results were compared with those obtained using the CLL-IPI.
Methods
Newly diagnosed Binet stage A patients (n=337) from several Italian Institutions prospectively enrolled into the O-CLL1 protocol (clinicaltrial.gov identifier: 115 NCT00917540) form the basis of this analysis.
Results
The Harrell’s c values which indicate the discriminatory power of the models (higher is better) were better for 2011 MDACC score (c-index, 0.71) and the O-CLL1 score (c-index,0.75) which were generated looking at TTFT as endpoint and combine clinical, biological and genetic markers. The same applied with GCLLSG (c-index,0.70) score and CLL-IPI (c-index, 0.70) even though they were originally developed with overall survival as main end pont. Finally, a c-statistic below 0.70 which is the threshold necessary to have value at the individual patient level was observed with 2007 MDACC score (c-index, 0.65) which was designed to assess overall survival as end point and did not incorporate major genetic factors. A global view of performances of different scores was also provided by the area under the receiver operating characteristic (ROC) curve figures considered an alternative measure of discrimination ( Figure 1). Furthermore, the time-dependent ROC analysis which is an extension of ROC curves demonstrated that for early time points (< 24 months) scores provided limited ability in distinguishing patients with different TTFT. In contrast, for late time points (≥ 24 months after diagnosis), the predictive accuracy of TTFT was higher for models including both clinical and genetic variables (i.e., O-CLL1, CLL-IPI,2011 MDACC score, GCLLSG score) in comparison with models which included only clinical variables (i.e., 2007 MDACC score). Finally, values of Aikaike information criterion (AIC) which indicates the goodness of the fit (lower is better) were better for the O-CLL1 score (AIC, 810) and worse for 2007 MDACC score (AIC, 851). In between there were the GCLLSG score (AIC, 837), the CLL-IPI (AIC, 841) and the 2011 MDACC score (AIC, 844), respectively .
Conclusion
Although different with respect to either the endpoints for which they were generated (i.e., OS versus TTFT) or the prognostic factors considered (i.e., only clinical versus clinical and genetic) all models used in this validation analysis worked in predicting TTFT. Results of AIC and Harrell’s c value demonstrated that the predictive accuracy of TTFT was higher for models including both clinical and genetic variables (i.e., CLL-01, CLL-IPI,2011 MDACC score, GCLLSG score).
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Prognosis
Type: Eposter Presentation
Background
Recent research in CLL focused on the development of prognostic scores which assemble in a same model different prognostic markers. However, analyses comparing the performances of these models are lacking.
Aims
In a prospective patient cohort we evaluated the capability of four recently proposed prognostic models in CLL (i.e., 2007 MDACC score, GCLLSG score, 2011 MDACC score,O-CLL1 score) to predict time to first treatment (TTFT). Results were compared with those obtained using the CLL-IPI.
Methods
Newly diagnosed Binet stage A patients (n=337) from several Italian Institutions prospectively enrolled into the O-CLL1 protocol (clinicaltrial.gov identifier: 115 NCT00917540) form the basis of this analysis.
Results
The Harrell’s c values which indicate the discriminatory power of the models (higher is better) were better for 2011 MDACC score (c-index, 0.71) and the O-CLL1 score (c-index,0.75) which were generated looking at TTFT as endpoint and combine clinical, biological and genetic markers. The same applied with GCLLSG (c-index,0.70) score and CLL-IPI (c-index, 0.70) even though they were originally developed with overall survival as main end pont. Finally, a c-statistic below 0.70 which is the threshold necessary to have value at the individual patient level was observed with 2007 MDACC score (c-index, 0.65) which was designed to assess overall survival as end point and did not incorporate major genetic factors. A global view of performances of different scores was also provided by the area under the receiver operating characteristic (ROC) curve figures considered an alternative measure of discrimination ( Figure 1). Furthermore, the time-dependent ROC analysis which is an extension of ROC curves demonstrated that for early time points (< 24 months) scores provided limited ability in distinguishing patients with different TTFT. In contrast, for late time points (≥ 24 months after diagnosis), the predictive accuracy of TTFT was higher for models including both clinical and genetic variables (i.e., O-CLL1, CLL-IPI,2011 MDACC score, GCLLSG score) in comparison with models which included only clinical variables (i.e., 2007 MDACC score). Finally, values of Aikaike information criterion (AIC) which indicates the goodness of the fit (lower is better) were better for the O-CLL1 score (AIC, 810) and worse for 2007 MDACC score (AIC, 851). In between there were the GCLLSG score (AIC, 837), the CLL-IPI (AIC, 841) and the 2011 MDACC score (AIC, 844), respectively .
Conclusion
Although different with respect to either the endpoints for which they were generated (i.e., OS versus TTFT) or the prognostic factors considered (i.e., only clinical versus clinical and genetic) all models used in this validation analysis worked in predicting TTFT. Results of AIC and Harrell’s c value demonstrated that the predictive accuracy of TTFT was higher for models including both clinical and genetic variables (i.e., CLL-01, CLL-IPI,2011 MDACC score, GCLLSG score).
Session topic: E-poster
Keyword(s): Chronic lymphocytic leukemia, Prognosis
{{ help_message }}
{{filter}}


