ANTIPHOSPHOLIPID ANTIBODIES IN PATIENTS WITH IMMUNE THROMBOCYTOPENIC PURPURA
(Abstract release date: 05/19/16)
EHA Library. Caliskan U. 06/09/16; 132549; E1000

Prof. Dr. Umran Caliskan
Contributions
Contributions
Abstract
Abstract: E1000
Type: Eposter Presentation
Background
Presence of antiphospholipid antibodies (APAs) has been observed in children with immune thrombocytopenic purpura (ITP), but their role for the outcome of disease is controversial.
Aims
The aim of this study was to evaluate the relation between APAs and the clinical course, labarotory findings, response to treatment and prognosis of ITP in childhood.
Methods
The cross-sectional study included to patients with newly diagnosed ITP aged between 0-18 years, in the period of time between March 2014 and March 2015, at our centre. Clinical and laboratory findings, medical treatments, and the course of the diseases were recorded for all patients. At the time of diagnosis, anti-phospholipid antibodies including lupus anticoagulant, anticardiolipin antibodies (aCL), anti-beta-2 glycoprotein I antibodies were studied. The patients who have positive results for APAs at diagnosis were examined again for APAs at 12th week of follow-up period.
Results
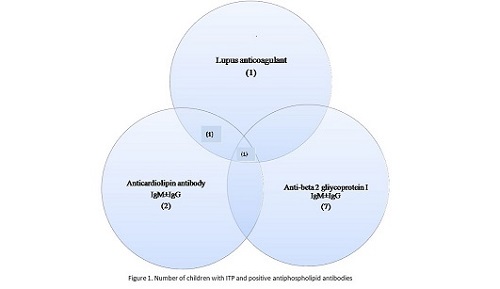
Forty children (21 (52.5%) females and 19 (47.5%) males) with newly diagnosed with ITP were enrolled the study. APA levels were positive at 12 patients (30%) at the time of diagnosis. Among the APA positive patients, only one patient had all of three APAs, one patient had both aCL IgM and LA, 10 patients had single positive results for APAs (figure 1). Among APA positive patients, the positivity of anti beta 2 glycoprotein I, aCL and LA were 58.3%, 16.7%, and 8.3% respectively. After 12 week, only 3 of these 20 cases were still positive for APA. One of them was positive both LA and anti beta 2 glycoprotein I, and two of them were positive for anti beta 2 glycoprotein I IgG. There was not a significant difference between APA positiveness (at the time of diagnosis and control) and gender groups, platelet counts, IgG levels or course of disease. At the time of diagnosis, mean age of APA positive patients was significantly higher than in APA negative patients (p<0.05). According to age interval; there was three patients aged between 0-1 year and none of them were APA positive. At the time of diagnosis, APA positiveness was found in 7 of 28 (25%) patients aged between1-9 years, and 5 of 9 patients (55.5%) aged between 9-18 years. There was no relationship between APAs and treatment response or outcome of disease.
Conclusion
Unlike in adults, pediatric studies about APAs and ITP are limited. APAs may be present in children with ITP. It may be related to underlying viral infections or idiopathic, and more common in adolescence. The persistence of APAs may contribute to thrombotic complications in the future. More comprehensive studies are needed to determine the relationship between APAs and İTP.
Session topic: E-poster
Keyword(s): Antiphospholipid antibody, Children, Immune thrombocytopenia (ITP)
Type: Eposter Presentation
Background
Presence of antiphospholipid antibodies (APAs) has been observed in children with immune thrombocytopenic purpura (ITP), but their role for the outcome of disease is controversial.
Aims
The aim of this study was to evaluate the relation between APAs and the clinical course, labarotory findings, response to treatment and prognosis of ITP in childhood.
Methods
The cross-sectional study included to patients with newly diagnosed ITP aged between 0-18 years, in the period of time between March 2014 and March 2015, at our centre. Clinical and laboratory findings, medical treatments, and the course of the diseases were recorded for all patients. At the time of diagnosis, anti-phospholipid antibodies including lupus anticoagulant, anticardiolipin antibodies (aCL), anti-beta-2 glycoprotein I antibodies were studied. The patients who have positive results for APAs at diagnosis were examined again for APAs at 12th week of follow-up period.
Results
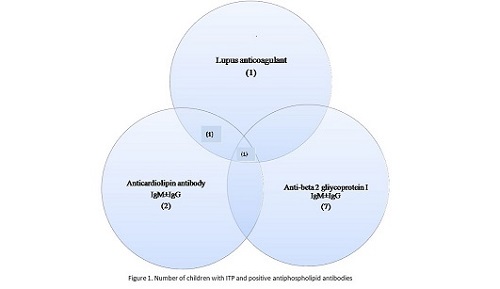
Forty children (21 (52.5%) females and 19 (47.5%) males) with newly diagnosed with ITP were enrolled the study. APA levels were positive at 12 patients (30%) at the time of diagnosis. Among the APA positive patients, only one patient had all of three APAs, one patient had both aCL IgM and LA, 10 patients had single positive results for APAs (figure 1). Among APA positive patients, the positivity of anti beta 2 glycoprotein I, aCL and LA were 58.3%, 16.7%, and 8.3% respectively. After 12 week, only 3 of these 20 cases were still positive for APA. One of them was positive both LA and anti beta 2 glycoprotein I, and two of them were positive for anti beta 2 glycoprotein I IgG. There was not a significant difference between APA positiveness (at the time of diagnosis and control) and gender groups, platelet counts, IgG levels or course of disease. At the time of diagnosis, mean age of APA positive patients was significantly higher than in APA negative patients (p<0.05). According to age interval; there was three patients aged between 0-1 year and none of them were APA positive. At the time of diagnosis, APA positiveness was found in 7 of 28 (25%) patients aged between1-9 years, and 5 of 9 patients (55.5%) aged between 9-18 years. There was no relationship between APAs and treatment response or outcome of disease.
Conclusion
Unlike in adults, pediatric studies about APAs and ITP are limited. APAs may be present in children with ITP. It may be related to underlying viral infections or idiopathic, and more common in adolescence. The persistence of APAs may contribute to thrombotic complications in the future. More comprehensive studies are needed to determine the relationship between APAs and İTP.
Session topic: E-poster
Keyword(s): Antiphospholipid antibody, Children, Immune thrombocytopenia (ITP)
Abstract: E1000
Type: Eposter Presentation
Background
Presence of antiphospholipid antibodies (APAs) has been observed in children with immune thrombocytopenic purpura (ITP), but their role for the outcome of disease is controversial.
Aims
The aim of this study was to evaluate the relation between APAs and the clinical course, labarotory findings, response to treatment and prognosis of ITP in childhood.
Methods
The cross-sectional study included to patients with newly diagnosed ITP aged between 0-18 years, in the period of time between March 2014 and March 2015, at our centre. Clinical and laboratory findings, medical treatments, and the course of the diseases were recorded for all patients. At the time of diagnosis, anti-phospholipid antibodies including lupus anticoagulant, anticardiolipin antibodies (aCL), anti-beta-2 glycoprotein I antibodies were studied. The patients who have positive results for APAs at diagnosis were examined again for APAs at 12th week of follow-up period.
Results
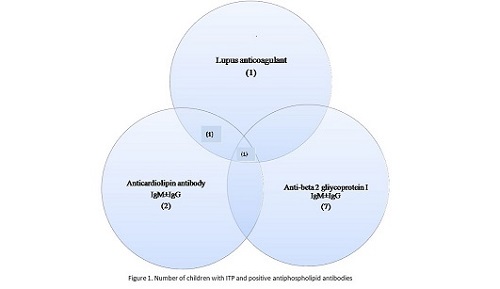
Forty children (21 (52.5%) females and 19 (47.5%) males) with newly diagnosed with ITP were enrolled the study. APA levels were positive at 12 patients (30%) at the time of diagnosis. Among the APA positive patients, only one patient had all of three APAs, one patient had both aCL IgM and LA, 10 patients had single positive results for APAs (figure 1). Among APA positive patients, the positivity of anti beta 2 glycoprotein I, aCL and LA were 58.3%, 16.7%, and 8.3% respectively. After 12 week, only 3 of these 20 cases were still positive for APA. One of them was positive both LA and anti beta 2 glycoprotein I, and two of them were positive for anti beta 2 glycoprotein I IgG. There was not a significant difference between APA positiveness (at the time of diagnosis and control) and gender groups, platelet counts, IgG levels or course of disease. At the time of diagnosis, mean age of APA positive patients was significantly higher than in APA negative patients (p<0.05). According to age interval; there was three patients aged between 0-1 year and none of them were APA positive. At the time of diagnosis, APA positiveness was found in 7 of 28 (25%) patients aged between1-9 years, and 5 of 9 patients (55.5%) aged between 9-18 years. There was no relationship between APAs and treatment response or outcome of disease.
Conclusion
Unlike in adults, pediatric studies about APAs and ITP are limited. APAs may be present in children with ITP. It may be related to underlying viral infections or idiopathic, and more common in adolescence. The persistence of APAs may contribute to thrombotic complications in the future. More comprehensive studies are needed to determine the relationship between APAs and İTP.
Session topic: E-poster
Keyword(s): Antiphospholipid antibody, Children, Immune thrombocytopenia (ITP)
Type: Eposter Presentation
Background
Presence of antiphospholipid antibodies (APAs) has been observed in children with immune thrombocytopenic purpura (ITP), but their role for the outcome of disease is controversial.
Aims
The aim of this study was to evaluate the relation between APAs and the clinical course, labarotory findings, response to treatment and prognosis of ITP in childhood.
Methods
The cross-sectional study included to patients with newly diagnosed ITP aged between 0-18 years, in the period of time between March 2014 and March 2015, at our centre. Clinical and laboratory findings, medical treatments, and the course of the diseases were recorded for all patients. At the time of diagnosis, anti-phospholipid antibodies including lupus anticoagulant, anticardiolipin antibodies (aCL), anti-beta-2 glycoprotein I antibodies were studied. The patients who have positive results for APAs at diagnosis were examined again for APAs at 12th week of follow-up period.
Results
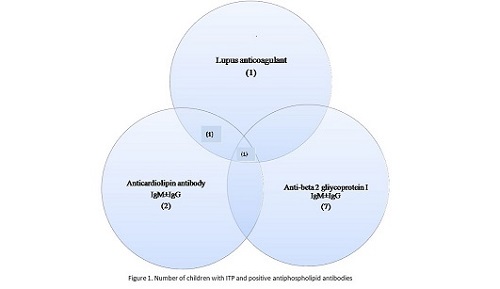
Forty children (21 (52.5%) females and 19 (47.5%) males) with newly diagnosed with ITP were enrolled the study. APA levels were positive at 12 patients (30%) at the time of diagnosis. Among the APA positive patients, only one patient had all of three APAs, one patient had both aCL IgM and LA, 10 patients had single positive results for APAs (figure 1). Among APA positive patients, the positivity of anti beta 2 glycoprotein I, aCL and LA were 58.3%, 16.7%, and 8.3% respectively. After 12 week, only 3 of these 20 cases were still positive for APA. One of them was positive both LA and anti beta 2 glycoprotein I, and two of them were positive for anti beta 2 glycoprotein I IgG. There was not a significant difference between APA positiveness (at the time of diagnosis and control) and gender groups, platelet counts, IgG levels or course of disease. At the time of diagnosis, mean age of APA positive patients was significantly higher than in APA negative patients (p<0.05). According to age interval; there was three patients aged between 0-1 year and none of them were APA positive. At the time of diagnosis, APA positiveness was found in 7 of 28 (25%) patients aged between1-9 years, and 5 of 9 patients (55.5%) aged between 9-18 years. There was no relationship between APAs and treatment response or outcome of disease.
Conclusion
Unlike in adults, pediatric studies about APAs and ITP are limited. APAs may be present in children with ITP. It may be related to underlying viral infections or idiopathic, and more common in adolescence. The persistence of APAs may contribute to thrombotic complications in the future. More comprehensive studies are needed to determine the relationship between APAs and İTP.
Session topic: E-poster
Keyword(s): Antiphospholipid antibody, Children, Immune thrombocytopenia (ITP)
{{ help_message }}
{{filter}}


