ACQUIRED ISOLATED PROTHROMBIN DEFICIENY IN A PATIENT WITH FOLLICULAR LYMPHOMA SUCCESSFULLY TREATED WITH IMMUNOCHEMOTHERAPY.
(Abstract release date: 05/19/16)
EHA Library. Müller K. 06/09/16; 132546; E997

Dr. Karsten Müller
Contributions
Contributions
Abstract
Abstract: E997
Type: Eposter Presentation
Background
Acquired haemophilia is rare bleeding disorder, that is caused by autoantibodies against clotting factors. Approximately 50% of cases are associated with either malignancies, autoimmune diseases or pregnancy, respectively. However, half of the cases remain idiopathic. While in the vast majority autoantibodies are directed against factor VIII leading to acquired haemophilia A, acquired prothrombin (factor II) deficiency is a rare event and information on treatment outcome is scarce.
Aims
Here we report on a case of a patient with follicular lymphoma and an acquired isolated prothrombin deficiency suffering from severe bleeding complications, who was successfully treated with immunochemotherapy.
Methods
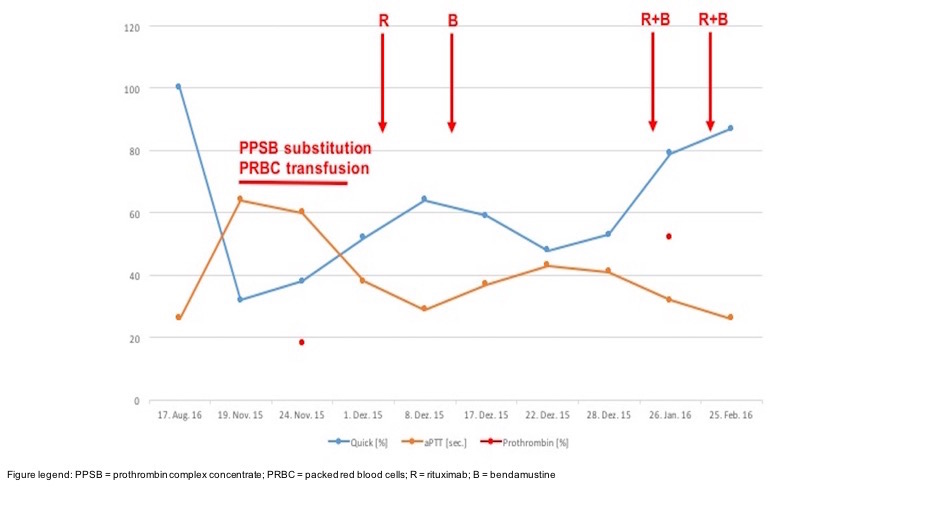
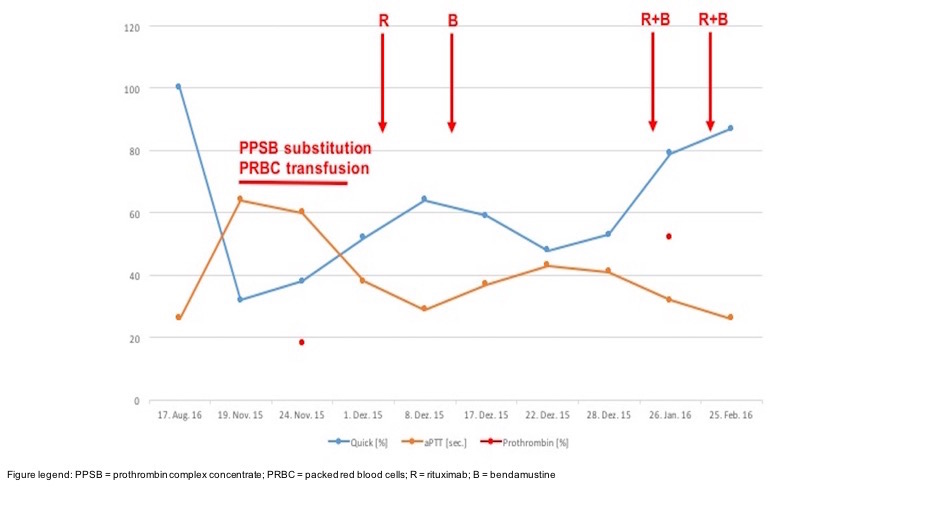
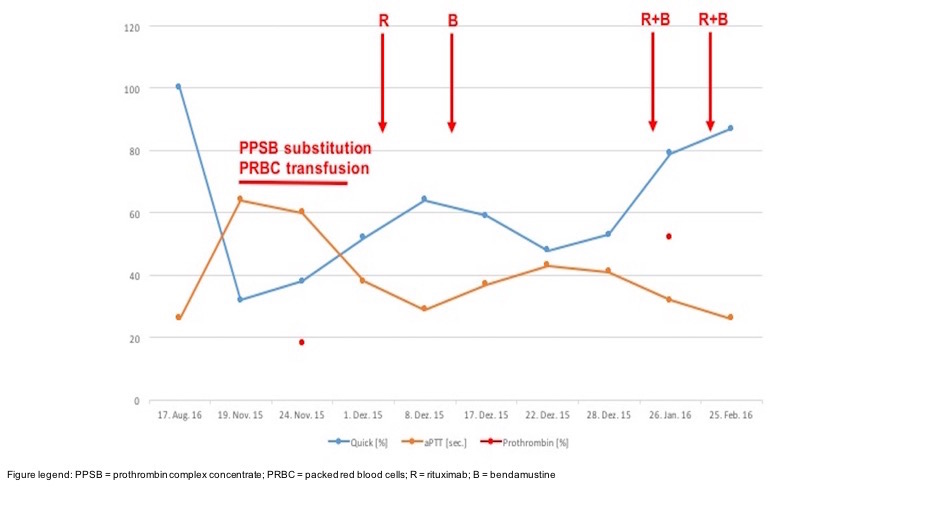
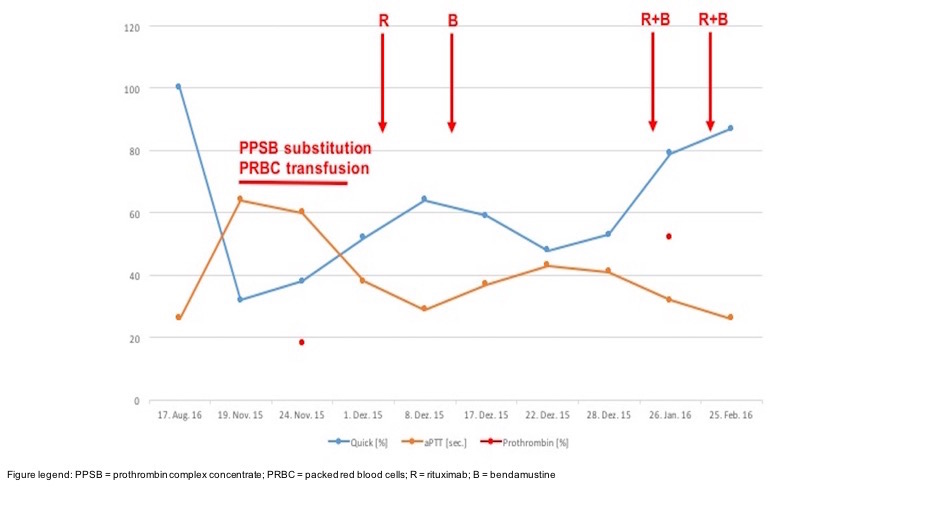
A 73-year old female patient was diagnosed with a grade I-II asymptomatic follicular lymphoma stage IV (intermediate risk according to FLIPI) in July 2015. In November 2015 the patient was admitted to our hospital due to macro haematuria and pain in the distal right thigh. The patient did not remember any trauma but MRI showed an intramuscular haematoma.Laboratory testing revealed decreased Quick values (32%) and a prolonged activated partial thromboplastin time (aPTT: 64 sec.) as compared to August 2015 (Quick 100%; aPTT 26 sec.) Since the patient received no anticoagulant treatment and diet-related vitamin K deficiency could be ruled out, single factor analyses were performed and showed an isolated prothrombin deficiency, which was confirmed by repeated analyses. Lupus anticoagulants were negative, as were analyses with regard to von-Willebrand-Jürgens syndrome.Moreover, the patient developed a haemoglobin relevant gastrointestinal bleeding with gastroscopy showing a diffuse bleeding in the fundus reflecting the haemorrhagic diathesis due to the coagulopathy. The patient received repetitive prothrombin substitution with prothrombin complex concentrates leading to transient stabilization of the coagulation system. Eventually she was subjected to successful surgical revision of the muscular haematoma.Although inhibitory antibodies were not detectable we assumed an association of the coagulopathy with the concomitant FCL and initiated an immunochemotherapy with rituximab and bendamustine in December 2015.
Results
Repetitive evaluation of coagulation parameters and prothrombin activity showed a successive improvement of the respective parameters after the first cycle of treatment (Figure 1). Since December 2015 no prothrombin substitution was necessary and prothrombin activity increased from 18% in November 2015 to 52% by January 2016. Currently, the patient has no signs of haemorrhage or relapse of the coagulopathy with continuous improvement of the global coagulation parameters.
Conclusion
Although rare events, isolated clotting factor deficiencies should be considered in cases of unexplained coagulopathy in patients with malignancy in general and malignant lymphoma in particular. Treatment of the underlying lymphoma by immunochemotherapy can reverse the haemophilic state in patients with NHL.
Session topic: E-poster
Keyword(s): Coagulopathy, Follicular lymphoma, Hemorrhage, Prothrombin
Type: Eposter Presentation
Background
Acquired haemophilia is rare bleeding disorder, that is caused by autoantibodies against clotting factors. Approximately 50% of cases are associated with either malignancies, autoimmune diseases or pregnancy, respectively. However, half of the cases remain idiopathic. While in the vast majority autoantibodies are directed against factor VIII leading to acquired haemophilia A, acquired prothrombin (factor II) deficiency is a rare event and information on treatment outcome is scarce.
Aims
Here we report on a case of a patient with follicular lymphoma and an acquired isolated prothrombin deficiency suffering from severe bleeding complications, who was successfully treated with immunochemotherapy.
Methods
A 73-year old female patient was diagnosed with a grade I-II asymptomatic follicular lymphoma stage IV (intermediate risk according to FLIPI) in July 2015. In November 2015 the patient was admitted to our hospital due to macro haematuria and pain in the distal right thigh. The patient did not remember any trauma but MRI showed an intramuscular haematoma.Laboratory testing revealed decreased Quick values (32%) and a prolonged activated partial thromboplastin time (aPTT: 64 sec.) as compared to August 2015 (Quick 100%; aPTT 26 sec.) Since the patient received no anticoagulant treatment and diet-related vitamin K deficiency could be ruled out, single factor analyses were performed and showed an isolated prothrombin deficiency, which was confirmed by repeated analyses. Lupus anticoagulants were negative, as were analyses with regard to von-Willebrand-Jürgens syndrome.Moreover, the patient developed a haemoglobin relevant gastrointestinal bleeding with gastroscopy showing a diffuse bleeding in the fundus reflecting the haemorrhagic diathesis due to the coagulopathy. The patient received repetitive prothrombin substitution with prothrombin complex concentrates leading to transient stabilization of the coagulation system. Eventually she was subjected to successful surgical revision of the muscular haematoma.Although inhibitory antibodies were not detectable we assumed an association of the coagulopathy with the concomitant FCL and initiated an immunochemotherapy with rituximab and bendamustine in December 2015.
Results
Repetitive evaluation of coagulation parameters and prothrombin activity showed a successive improvement of the respective parameters after the first cycle of treatment (Figure 1). Since December 2015 no prothrombin substitution was necessary and prothrombin activity increased from 18% in November 2015 to 52% by January 2016. Currently, the patient has no signs of haemorrhage or relapse of the coagulopathy with continuous improvement of the global coagulation parameters.
Conclusion
Although rare events, isolated clotting factor deficiencies should be considered in cases of unexplained coagulopathy in patients with malignancy in general and malignant lymphoma in particular. Treatment of the underlying lymphoma by immunochemotherapy can reverse the haemophilic state in patients with NHL.
Session topic: E-poster
Keyword(s): Coagulopathy, Follicular lymphoma, Hemorrhage, Prothrombin
Abstract: E997
Type: Eposter Presentation
Background
Acquired haemophilia is rare bleeding disorder, that is caused by autoantibodies against clotting factors. Approximately 50% of cases are associated with either malignancies, autoimmune diseases or pregnancy, respectively. However, half of the cases remain idiopathic. While in the vast majority autoantibodies are directed against factor VIII leading to acquired haemophilia A, acquired prothrombin (factor II) deficiency is a rare event and information on treatment outcome is scarce.
Aims
Here we report on a case of a patient with follicular lymphoma and an acquired isolated prothrombin deficiency suffering from severe bleeding complications, who was successfully treated with immunochemotherapy.
Methods
A 73-year old female patient was diagnosed with a grade I-II asymptomatic follicular lymphoma stage IV (intermediate risk according to FLIPI) in July 2015. In November 2015 the patient was admitted to our hospital due to macro haematuria and pain in the distal right thigh. The patient did not remember any trauma but MRI showed an intramuscular haematoma.Laboratory testing revealed decreased Quick values (32%) and a prolonged activated partial thromboplastin time (aPTT: 64 sec.) as compared to August 2015 (Quick 100%; aPTT 26 sec.) Since the patient received no anticoagulant treatment and diet-related vitamin K deficiency could be ruled out, single factor analyses were performed and showed an isolated prothrombin deficiency, which was confirmed by repeated analyses. Lupus anticoagulants were negative, as were analyses with regard to von-Willebrand-Jürgens syndrome.Moreover, the patient developed a haemoglobin relevant gastrointestinal bleeding with gastroscopy showing a diffuse bleeding in the fundus reflecting the haemorrhagic diathesis due to the coagulopathy. The patient received repetitive prothrombin substitution with prothrombin complex concentrates leading to transient stabilization of the coagulation system. Eventually she was subjected to successful surgical revision of the muscular haematoma.Although inhibitory antibodies were not detectable we assumed an association of the coagulopathy with the concomitant FCL and initiated an immunochemotherapy with rituximab and bendamustine in December 2015.
Results
Repetitive evaluation of coagulation parameters and prothrombin activity showed a successive improvement of the respective parameters after the first cycle of treatment (Figure 1). Since December 2015 no prothrombin substitution was necessary and prothrombin activity increased from 18% in November 2015 to 52% by January 2016. Currently, the patient has no signs of haemorrhage or relapse of the coagulopathy with continuous improvement of the global coagulation parameters.
Conclusion
Although rare events, isolated clotting factor deficiencies should be considered in cases of unexplained coagulopathy in patients with malignancy in general and malignant lymphoma in particular. Treatment of the underlying lymphoma by immunochemotherapy can reverse the haemophilic state in patients with NHL.
Session topic: E-poster
Keyword(s): Coagulopathy, Follicular lymphoma, Hemorrhage, Prothrombin
Type: Eposter Presentation
Background
Acquired haemophilia is rare bleeding disorder, that is caused by autoantibodies against clotting factors. Approximately 50% of cases are associated with either malignancies, autoimmune diseases or pregnancy, respectively. However, half of the cases remain idiopathic. While in the vast majority autoantibodies are directed against factor VIII leading to acquired haemophilia A, acquired prothrombin (factor II) deficiency is a rare event and information on treatment outcome is scarce.
Aims
Here we report on a case of a patient with follicular lymphoma and an acquired isolated prothrombin deficiency suffering from severe bleeding complications, who was successfully treated with immunochemotherapy.
Methods
A 73-year old female patient was diagnosed with a grade I-II asymptomatic follicular lymphoma stage IV (intermediate risk according to FLIPI) in July 2015. In November 2015 the patient was admitted to our hospital due to macro haematuria and pain in the distal right thigh. The patient did not remember any trauma but MRI showed an intramuscular haematoma.Laboratory testing revealed decreased Quick values (32%) and a prolonged activated partial thromboplastin time (aPTT: 64 sec.) as compared to August 2015 (Quick 100%; aPTT 26 sec.) Since the patient received no anticoagulant treatment and diet-related vitamin K deficiency could be ruled out, single factor analyses were performed and showed an isolated prothrombin deficiency, which was confirmed by repeated analyses. Lupus anticoagulants were negative, as were analyses with regard to von-Willebrand-Jürgens syndrome.Moreover, the patient developed a haemoglobin relevant gastrointestinal bleeding with gastroscopy showing a diffuse bleeding in the fundus reflecting the haemorrhagic diathesis due to the coagulopathy. The patient received repetitive prothrombin substitution with prothrombin complex concentrates leading to transient stabilization of the coagulation system. Eventually she was subjected to successful surgical revision of the muscular haematoma.Although inhibitory antibodies were not detectable we assumed an association of the coagulopathy with the concomitant FCL and initiated an immunochemotherapy with rituximab and bendamustine in December 2015.
Results
Repetitive evaluation of coagulation parameters and prothrombin activity showed a successive improvement of the respective parameters after the first cycle of treatment (Figure 1). Since December 2015 no prothrombin substitution was necessary and prothrombin activity increased from 18% in November 2015 to 52% by January 2016. Currently, the patient has no signs of haemorrhage or relapse of the coagulopathy with continuous improvement of the global coagulation parameters.
Conclusion
Although rare events, isolated clotting factor deficiencies should be considered in cases of unexplained coagulopathy in patients with malignancy in general and malignant lymphoma in particular. Treatment of the underlying lymphoma by immunochemotherapy can reverse the haemophilic state in patients with NHL.
Session topic: E-poster
Keyword(s): Coagulopathy, Follicular lymphoma, Hemorrhage, Prothrombin
{{ help_message }}
{{filter}}


