DIRECT ORAL ANTICOAGULANTS THERAPY AFTER INTRACRANIAL HAEMORRHAGE WHILE ON VITAMIN K ANTAGONISTS
(Abstract release date: 05/19/16)
EHA Library. Zabalza A. 06/09/16; 132543; E994

Amaya Zabalza
Contributions
Contributions
Abstract
Abstract: E994
Type: Eposter Presentation
Background
Restarting antithrombotic therapy after an intracranial haemorrhage while on vitamin K antagonists (VKA-ICH) treatment is challenging in many cases. When cardioembolic risk is high (CHADS2-Vasc ≥ 3) antithrombotic therapy should be offered to these patients. The lower rate of intracranial bleeding of direct oral anticoagulants (DOACs) compared to warfarin reported in recent phase III randomized trials for patients diagnosed of non valvular atrial fibrillation (NVAF), probably make these drugs a safer option to treat VKA-ICH patients.
Aims
The objective of this retrospective, observational study is to evaluate the efficacy and safety of restarting oral anticoagulation treatment with DOACs in NVAF patients with a high cardioembolic risk and a previous VKA-ICH episode.
Methods
From October 2012 until January 2016 a total of 23 patients at the Complejo Hospitalario de Navarra were treated with DOACs after a VKA-ICH episode while on treatment with the VKA acenocoumarol (sintrom®). We analysed the following variables: INR on admission, the time in the therapeutic range (TTR), the rate of spontaneous or posttraumatic ICH, the use of reversal drugs on admission, the median days to restart oral anticoagulation, and the cumulative incidence of a second ICH following the restart of anticoagulation treatment.
Results
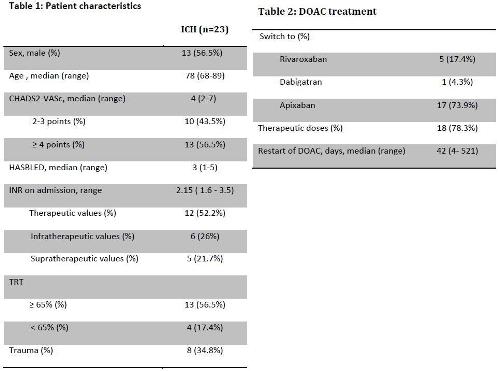
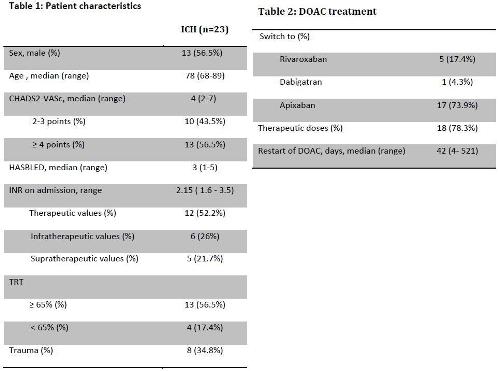
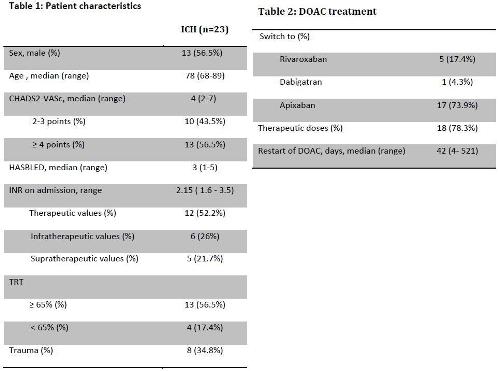
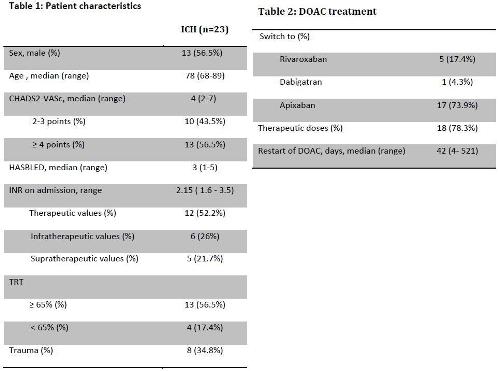
23 patients with intracranial hemorrhage during treatment with VKA restart anticoagulation with a DOAC at our institution. The median age was 78 (68-89), 56.5% were male. All patients had been treated with a VKA antagonist for NVAF with a median CHADS2VASc score of 4 (2-7) and a median HASBLED of 3 (1-5). The mayority of ICH events ocurred spontaneously (65.2%). In contrast, 34.8% ICH occurred after trauma. Only one patient in our cohort had a lobar ICH. International normalized ratio (INR) on admission was infratherapetic in 26 % (n=6), therapeutic in 52.2% (n=12) and supratherapetic in 21.7% (n=5). The mayority of cases were managed at the Emergency room with non activated prothrombin complex concentrate (PCC) (73.9%) as reversal agent with a median dose of 24.6 UI/kg (9.68-37.5) in combination with 10 intravenous mg of vitamin K. (Table 1).The median days to restart oral anticoagulation with a DOACs after an ICH was 42 (4-521). 17.4% rivaroxaban (n=5), 4.3% dabigatran (n=1) and 73.9% apixaban (n=17). With a median follow up of 32.88 months (3-88.58) the cumulative incidence of a second ICH was 7.1% (standard error 6.9%). Only 2 patients in our cohort had recurrent spontaneous ICH, one under rivaroxaban 15 mg once daily and a second one while on apixaban 2.5 mg bid, at 19 and 43 months after restarting DOACs, respectively. No thromboembolic event was recorded during the follow up in our cohort. (Table 2).
Conclusion
The use of direct oral anticoagulants after an ICH is a safe option for long-term anticoagulation treatment in patients with non-valvular atrial fibrillation at high risk of ischaemic stroke. However, further studies are required to assess longer-term efficacy and safety of DOAC after an ICH.
Session topic: E-poster
Keyword(s): Cerebral hemorrhage, Oral anticoagulant
Type: Eposter Presentation
Background
Restarting antithrombotic therapy after an intracranial haemorrhage while on vitamin K antagonists (VKA-ICH) treatment is challenging in many cases. When cardioembolic risk is high (CHADS2-Vasc ≥ 3) antithrombotic therapy should be offered to these patients. The lower rate of intracranial bleeding of direct oral anticoagulants (DOACs) compared to warfarin reported in recent phase III randomized trials for patients diagnosed of non valvular atrial fibrillation (NVAF), probably make these drugs a safer option to treat VKA-ICH patients.
Aims
The objective of this retrospective, observational study is to evaluate the efficacy and safety of restarting oral anticoagulation treatment with DOACs in NVAF patients with a high cardioembolic risk and a previous VKA-ICH episode.
Methods
From October 2012 until January 2016 a total of 23 patients at the Complejo Hospitalario de Navarra were treated with DOACs after a VKA-ICH episode while on treatment with the VKA acenocoumarol (sintrom®). We analysed the following variables: INR on admission, the time in the therapeutic range (TTR), the rate of spontaneous or posttraumatic ICH, the use of reversal drugs on admission, the median days to restart oral anticoagulation, and the cumulative incidence of a second ICH following the restart of anticoagulation treatment.
Results
23 patients with intracranial hemorrhage during treatment with VKA restart anticoagulation with a DOAC at our institution. The median age was 78 (68-89), 56.5% were male. All patients had been treated with a VKA antagonist for NVAF with a median CHADS2VASc score of 4 (2-7) and a median HASBLED of 3 (1-5). The mayority of ICH events ocurred spontaneously (65.2%). In contrast, 34.8% ICH occurred after trauma. Only one patient in our cohort had a lobar ICH. International normalized ratio (INR) on admission was infratherapetic in 26 % (n=6), therapeutic in 52.2% (n=12) and supratherapetic in 21.7% (n=5). The mayority of cases were managed at the Emergency room with non activated prothrombin complex concentrate (PCC) (73.9%) as reversal agent with a median dose of 24.6 UI/kg (9.68-37.5) in combination with 10 intravenous mg of vitamin K. (Table 1).The median days to restart oral anticoagulation with a DOACs after an ICH was 42 (4-521). 17.4% rivaroxaban (n=5), 4.3% dabigatran (n=1) and 73.9% apixaban (n=17). With a median follow up of 32.88 months (3-88.58) the cumulative incidence of a second ICH was 7.1% (standard error 6.9%). Only 2 patients in our cohort had recurrent spontaneous ICH, one under rivaroxaban 15 mg once daily and a second one while on apixaban 2.5 mg bid, at 19 and 43 months after restarting DOACs, respectively. No thromboembolic event was recorded during the follow up in our cohort. (Table 2).
Conclusion
The use of direct oral anticoagulants after an ICH is a safe option for long-term anticoagulation treatment in patients with non-valvular atrial fibrillation at high risk of ischaemic stroke. However, further studies are required to assess longer-term efficacy and safety of DOAC after an ICH.
Session topic: E-poster
Keyword(s): Cerebral hemorrhage, Oral anticoagulant
Abstract: E994
Type: Eposter Presentation
Background
Restarting antithrombotic therapy after an intracranial haemorrhage while on vitamin K antagonists (VKA-ICH) treatment is challenging in many cases. When cardioembolic risk is high (CHADS2-Vasc ≥ 3) antithrombotic therapy should be offered to these patients. The lower rate of intracranial bleeding of direct oral anticoagulants (DOACs) compared to warfarin reported in recent phase III randomized trials for patients diagnosed of non valvular atrial fibrillation (NVAF), probably make these drugs a safer option to treat VKA-ICH patients.
Aims
The objective of this retrospective, observational study is to evaluate the efficacy and safety of restarting oral anticoagulation treatment with DOACs in NVAF patients with a high cardioembolic risk and a previous VKA-ICH episode.
Methods
From October 2012 until January 2016 a total of 23 patients at the Complejo Hospitalario de Navarra were treated with DOACs after a VKA-ICH episode while on treatment with the VKA acenocoumarol (sintrom®). We analysed the following variables: INR on admission, the time in the therapeutic range (TTR), the rate of spontaneous or posttraumatic ICH, the use of reversal drugs on admission, the median days to restart oral anticoagulation, and the cumulative incidence of a second ICH following the restart of anticoagulation treatment.
Results
23 patients with intracranial hemorrhage during treatment with VKA restart anticoagulation with a DOAC at our institution. The median age was 78 (68-89), 56.5% were male. All patients had been treated with a VKA antagonist for NVAF with a median CHADS2VASc score of 4 (2-7) and a median HASBLED of 3 (1-5). The mayority of ICH events ocurred spontaneously (65.2%). In contrast, 34.8% ICH occurred after trauma. Only one patient in our cohort had a lobar ICH. International normalized ratio (INR) on admission was infratherapetic in 26 % (n=6), therapeutic in 52.2% (n=12) and supratherapetic in 21.7% (n=5). The mayority of cases were managed at the Emergency room with non activated prothrombin complex concentrate (PCC) (73.9%) as reversal agent with a median dose of 24.6 UI/kg (9.68-37.5) in combination with 10 intravenous mg of vitamin K. (Table 1).The median days to restart oral anticoagulation with a DOACs after an ICH was 42 (4-521). 17.4% rivaroxaban (n=5), 4.3% dabigatran (n=1) and 73.9% apixaban (n=17). With a median follow up of 32.88 months (3-88.58) the cumulative incidence of a second ICH was 7.1% (standard error 6.9%). Only 2 patients in our cohort had recurrent spontaneous ICH, one under rivaroxaban 15 mg once daily and a second one while on apixaban 2.5 mg bid, at 19 and 43 months after restarting DOACs, respectively. No thromboembolic event was recorded during the follow up in our cohort. (Table 2).
Conclusion
The use of direct oral anticoagulants after an ICH is a safe option for long-term anticoagulation treatment in patients with non-valvular atrial fibrillation at high risk of ischaemic stroke. However, further studies are required to assess longer-term efficacy and safety of DOAC after an ICH.
Session topic: E-poster
Keyword(s): Cerebral hemorrhage, Oral anticoagulant
Type: Eposter Presentation
Background
Restarting antithrombotic therapy after an intracranial haemorrhage while on vitamin K antagonists (VKA-ICH) treatment is challenging in many cases. When cardioembolic risk is high (CHADS2-Vasc ≥ 3) antithrombotic therapy should be offered to these patients. The lower rate of intracranial bleeding of direct oral anticoagulants (DOACs) compared to warfarin reported in recent phase III randomized trials for patients diagnosed of non valvular atrial fibrillation (NVAF), probably make these drugs a safer option to treat VKA-ICH patients.
Aims
The objective of this retrospective, observational study is to evaluate the efficacy and safety of restarting oral anticoagulation treatment with DOACs in NVAF patients with a high cardioembolic risk and a previous VKA-ICH episode.
Methods
From October 2012 until January 2016 a total of 23 patients at the Complejo Hospitalario de Navarra were treated with DOACs after a VKA-ICH episode while on treatment with the VKA acenocoumarol (sintrom®). We analysed the following variables: INR on admission, the time in the therapeutic range (TTR), the rate of spontaneous or posttraumatic ICH, the use of reversal drugs on admission, the median days to restart oral anticoagulation, and the cumulative incidence of a second ICH following the restart of anticoagulation treatment.
Results
23 patients with intracranial hemorrhage during treatment with VKA restart anticoagulation with a DOAC at our institution. The median age was 78 (68-89), 56.5% were male. All patients had been treated with a VKA antagonist for NVAF with a median CHADS2VASc score of 4 (2-7) and a median HASBLED of 3 (1-5). The mayority of ICH events ocurred spontaneously (65.2%). In contrast, 34.8% ICH occurred after trauma. Only one patient in our cohort had a lobar ICH. International normalized ratio (INR) on admission was infratherapetic in 26 % (n=6), therapeutic in 52.2% (n=12) and supratherapetic in 21.7% (n=5). The mayority of cases were managed at the Emergency room with non activated prothrombin complex concentrate (PCC) (73.9%) as reversal agent with a median dose of 24.6 UI/kg (9.68-37.5) in combination with 10 intravenous mg of vitamin K. (Table 1).The median days to restart oral anticoagulation with a DOACs after an ICH was 42 (4-521). 17.4% rivaroxaban (n=5), 4.3% dabigatran (n=1) and 73.9% apixaban (n=17). With a median follow up of 32.88 months (3-88.58) the cumulative incidence of a second ICH was 7.1% (standard error 6.9%). Only 2 patients in our cohort had recurrent spontaneous ICH, one under rivaroxaban 15 mg once daily and a second one while on apixaban 2.5 mg bid, at 19 and 43 months after restarting DOACs, respectively. No thromboembolic event was recorded during the follow up in our cohort. (Table 2).
Conclusion
The use of direct oral anticoagulants after an ICH is a safe option for long-term anticoagulation treatment in patients with non-valvular atrial fibrillation at high risk of ischaemic stroke. However, further studies are required to assess longer-term efficacy and safety of DOAC after an ICH.
Session topic: E-poster
Keyword(s): Cerebral hemorrhage, Oral anticoagulant
{{ help_message }}
{{filter}}


