PRIMARY BONE MARROW LYMPHOMA: A HEMATOLOGICAL EMERGENCY IN ADULTS WITH FEVER OF UNKNOWN ORIGIN
(Abstract release date: 05/19/16)
EHA Library. Yuan Wang H. 06/09/16; 132532; E983
Disclosure(s): I declare that I have no conflict of interest.

Dr. Hao Yuan Wang
Contributions
Contributions
Abstract
Abstract: E983
Type: Eposter Presentation
Background
Primary bone marrow lymphoma (PBML) denotes non-Hodgkin lymphoma (NHL) arising primarily in the bone marrow (BM) without any lymphadenopathy. It is often masked by prolonged fever leading to delayed diagnosis and notorious for various definitions adopted by previous studies.
Aims
This study aimed to lighten clinical panorama of PBML and to identify potentially warning parameters of PBML.
Methods
Two cohorts of PBML patients were enrolled. Cohort I consisted of 163 PBML cases from 16 case series and 23 case reports for meta-analysis of clinical characteristics. Cohort II comprised 221 adults with fever of unknown origin (FUO) from Taipei Veterans General Hospital who underwent a BM study, and 52 cases of them were finally diagnosed of NHLs, including 26 PBML cases. The latter cohort was used to identify warning parameters of PBML by comparing data upon admission between all FUO patients with and without a subsequent PBML diagnosis.
Results
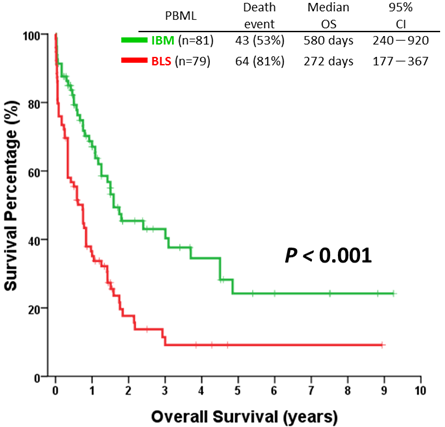
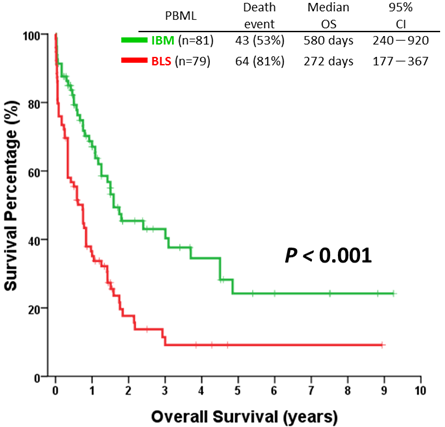
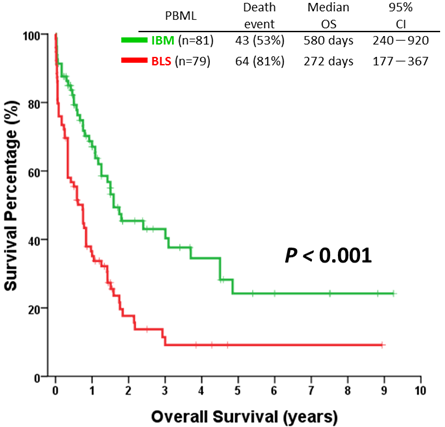
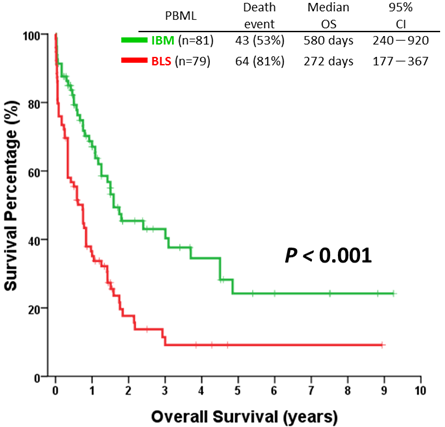
In cohort I, PBML had heterogenous histology and could be clinically separated into two distinct entities: lymphoma limited entirely to the BM, liver, and/or spleen (i.e. BLS-type, n=79), and isolated BM lymphoma (i.e. IBM-type, n=84). Two third (67%) of PBML patients initially manifested with fever, and one third (31%) complicated with hemophagocytic lymphohistiocytosis (HLH). The BLS-type cases were mainly reported from the countries in Eastern Asia, more often presented as FUO and HLH at diagnosis, and suffered from a poorer prognosis (median overall survival of BLS-type vs. IBM type = 272 vs. 580 days, P<0.001). For 26 PBML patients of the cohort II, 89 % were classified as BLS-type; median overall survival revealed dismal 9 days, with 54 % having early mortality within 30 days. Compared to non-PBML NHL in the cohort II, PBML is an independent risk factor of both early mortality and overall survival. Among 221 FUO adults in cohort II, 4 warning parameters able to alert underlying PBML were independently identified, including serum alkaline phosphate >2× UNL, serum immunoglobulin G <0.67× UNL, cytopenia ≥2 lineages, and leucoerythroblastosis in the peripheral blood.
Conclusion
As a particular clinical phenotype of NHL, PBML is often masked by prolonged fever and should be regarded as a hematological emergency when approaching patients with FUO. Our study provided additional diagnostic clues to early recognize FUO adults with underlying PBML.
Session topic: E-poster
Keyword(s): Fever, Non-Hodgkin's lymphoma
Type: Eposter Presentation
Background
Primary bone marrow lymphoma (PBML) denotes non-Hodgkin lymphoma (NHL) arising primarily in the bone marrow (BM) without any lymphadenopathy. It is often masked by prolonged fever leading to delayed diagnosis and notorious for various definitions adopted by previous studies.
Aims
This study aimed to lighten clinical panorama of PBML and to identify potentially warning parameters of PBML.
Methods
Two cohorts of PBML patients were enrolled. Cohort I consisted of 163 PBML cases from 16 case series and 23 case reports for meta-analysis of clinical characteristics. Cohort II comprised 221 adults with fever of unknown origin (FUO) from Taipei Veterans General Hospital who underwent a BM study, and 52 cases of them were finally diagnosed of NHLs, including 26 PBML cases. The latter cohort was used to identify warning parameters of PBML by comparing data upon admission between all FUO patients with and without a subsequent PBML diagnosis.
Results
In cohort I, PBML had heterogenous histology and could be clinically separated into two distinct entities: lymphoma limited entirely to the BM, liver, and/or spleen (i.e. BLS-type, n=79), and isolated BM lymphoma (i.e. IBM-type, n=84). Two third (67%) of PBML patients initially manifested with fever, and one third (31%) complicated with hemophagocytic lymphohistiocytosis (HLH). The BLS-type cases were mainly reported from the countries in Eastern Asia, more often presented as FUO and HLH at diagnosis, and suffered from a poorer prognosis (median overall survival of BLS-type vs. IBM type = 272 vs. 580 days, P<0.001). For 26 PBML patients of the cohort II, 89 % were classified as BLS-type; median overall survival revealed dismal 9 days, with 54 % having early mortality within 30 days. Compared to non-PBML NHL in the cohort II, PBML is an independent risk factor of both early mortality and overall survival. Among 221 FUO adults in cohort II, 4 warning parameters able to alert underlying PBML were independently identified, including serum alkaline phosphate >2× UNL, serum immunoglobulin G <0.67× UNL, cytopenia ≥2 lineages, and leucoerythroblastosis in the peripheral blood.
| TABLE 1. Univariate and multivariate analyses of warning parameters for primary bone marrow lymphoma in 221 adults with fever of unknown origin | ||||
| Warning parameters for PBML | Univariate | Multivariate | ||
| OR (95% CI) | P | OR (95% CI) | P | |
| Bicytopenia or pancytopenia | 22.844 (6.572–79.404) | <0.001 | 20.559 (3.101–136.279) | 0.002 |
| Leucoerythroblastosis in PB smear | 1.390 (1.193–1.619) | <0.001 | 1.384 (1.008–1.901) | 0.045 |
| LDH >500 IU/L (2x UNL) | 15.693 (4.543–54.212) | <0.001 | 4.956 (0.832–29.511) | 0.079 |
| IgG <1000 (0.67x UNL) | 4.912 (2.015–11.972) | <0.001 | 5.086 (1.046–24.728) | 0.044 |
| ALP >200 U/L (2x UNL) | 6.000 (2.473–14.556) | <0.001 | 5.857 (1.179–29.085) | 0.031 |
| PT >12 sec (1x UNL) | 6.416 (2.551–16.133) | <0.001 | 4.457 (0.939–21.161) | 0.060 |
Conclusion
As a particular clinical phenotype of NHL, PBML is often masked by prolonged fever and should be regarded as a hematological emergency when approaching patients with FUO. Our study provided additional diagnostic clues to early recognize FUO adults with underlying PBML.
Session topic: E-poster
Keyword(s): Fever, Non-Hodgkin's lymphoma
Abstract: E983
Type: Eposter Presentation
Background
Primary bone marrow lymphoma (PBML) denotes non-Hodgkin lymphoma (NHL) arising primarily in the bone marrow (BM) without any lymphadenopathy. It is often masked by prolonged fever leading to delayed diagnosis and notorious for various definitions adopted by previous studies.
Aims
This study aimed to lighten clinical panorama of PBML and to identify potentially warning parameters of PBML.
Methods
Two cohorts of PBML patients were enrolled. Cohort I consisted of 163 PBML cases from 16 case series and 23 case reports for meta-analysis of clinical characteristics. Cohort II comprised 221 adults with fever of unknown origin (FUO) from Taipei Veterans General Hospital who underwent a BM study, and 52 cases of them were finally diagnosed of NHLs, including 26 PBML cases. The latter cohort was used to identify warning parameters of PBML by comparing data upon admission between all FUO patients with and without a subsequent PBML diagnosis.
Results
In cohort I, PBML had heterogenous histology and could be clinically separated into two distinct entities: lymphoma limited entirely to the BM, liver, and/or spleen (i.e. BLS-type, n=79), and isolated BM lymphoma (i.e. IBM-type, n=84). Two third (67%) of PBML patients initially manifested with fever, and one third (31%) complicated with hemophagocytic lymphohistiocytosis (HLH). The BLS-type cases were mainly reported from the countries in Eastern Asia, more often presented as FUO and HLH at diagnosis, and suffered from a poorer prognosis (median overall survival of BLS-type vs. IBM type = 272 vs. 580 days, P<0.001). For 26 PBML patients of the cohort II, 89 % were classified as BLS-type; median overall survival revealed dismal 9 days, with 54 % having early mortality within 30 days. Compared to non-PBML NHL in the cohort II, PBML is an independent risk factor of both early mortality and overall survival. Among 221 FUO adults in cohort II, 4 warning parameters able to alert underlying PBML were independently identified, including serum alkaline phosphate >2× UNL, serum immunoglobulin G <0.67× UNL, cytopenia ≥2 lineages, and leucoerythroblastosis in the peripheral blood.
Conclusion
As a particular clinical phenotype of NHL, PBML is often masked by prolonged fever and should be regarded as a hematological emergency when approaching patients with FUO. Our study provided additional diagnostic clues to early recognize FUO adults with underlying PBML.
Session topic: E-poster
Keyword(s): Fever, Non-Hodgkin's lymphoma
Type: Eposter Presentation
Background
Primary bone marrow lymphoma (PBML) denotes non-Hodgkin lymphoma (NHL) arising primarily in the bone marrow (BM) without any lymphadenopathy. It is often masked by prolonged fever leading to delayed diagnosis and notorious for various definitions adopted by previous studies.
Aims
This study aimed to lighten clinical panorama of PBML and to identify potentially warning parameters of PBML.
Methods
Two cohorts of PBML patients were enrolled. Cohort I consisted of 163 PBML cases from 16 case series and 23 case reports for meta-analysis of clinical characteristics. Cohort II comprised 221 adults with fever of unknown origin (FUO) from Taipei Veterans General Hospital who underwent a BM study, and 52 cases of them were finally diagnosed of NHLs, including 26 PBML cases. The latter cohort was used to identify warning parameters of PBML by comparing data upon admission between all FUO patients with and without a subsequent PBML diagnosis.
Results
In cohort I, PBML had heterogenous histology and could be clinically separated into two distinct entities: lymphoma limited entirely to the BM, liver, and/or spleen (i.e. BLS-type, n=79), and isolated BM lymphoma (i.e. IBM-type, n=84). Two third (67%) of PBML patients initially manifested with fever, and one third (31%) complicated with hemophagocytic lymphohistiocytosis (HLH). The BLS-type cases were mainly reported from the countries in Eastern Asia, more often presented as FUO and HLH at diagnosis, and suffered from a poorer prognosis (median overall survival of BLS-type vs. IBM type = 272 vs. 580 days, P<0.001). For 26 PBML patients of the cohort II, 89 % were classified as BLS-type; median overall survival revealed dismal 9 days, with 54 % having early mortality within 30 days. Compared to non-PBML NHL in the cohort II, PBML is an independent risk factor of both early mortality and overall survival. Among 221 FUO adults in cohort II, 4 warning parameters able to alert underlying PBML were independently identified, including serum alkaline phosphate >2× UNL, serum immunoglobulin G <0.67× UNL, cytopenia ≥2 lineages, and leucoerythroblastosis in the peripheral blood.
| TABLE 1. Univariate and multivariate analyses of warning parameters for primary bone marrow lymphoma in 221 adults with fever of unknown origin | ||||
| Warning parameters for PBML | Univariate | Multivariate | ||
| OR (95% CI) | P | OR (95% CI) | P | |
| Bicytopenia or pancytopenia | 22.844 (6.572–79.404) | <0.001 | 20.559 (3.101–136.279) | 0.002 |
| Leucoerythroblastosis in PB smear | 1.390 (1.193–1.619) | <0.001 | 1.384 (1.008–1.901) | 0.045 |
| LDH >500 IU/L (2x UNL) | 15.693 (4.543–54.212) | <0.001 | 4.956 (0.832–29.511) | 0.079 |
| IgG <1000 (0.67x UNL) | 4.912 (2.015–11.972) | <0.001 | 5.086 (1.046–24.728) | 0.044 |
| ALP >200 U/L (2x UNL) | 6.000 (2.473–14.556) | <0.001 | 5.857 (1.179–29.085) | 0.031 |
| PT >12 sec (1x UNL) | 6.416 (2.551–16.133) | <0.001 | 4.457 (0.939–21.161) | 0.060 |
Conclusion
As a particular clinical phenotype of NHL, PBML is often masked by prolonged fever and should be regarded as a hematological emergency when approaching patients with FUO. Our study provided additional diagnostic clues to early recognize FUO adults with underlying PBML.
Session topic: E-poster
Keyword(s): Fever, Non-Hodgkin's lymphoma
{{ help_message }}
{{filter}}


