SURVIVAL IMPACT OF SERUM ALBUMIN (SA) IN PATIENTS WITH ACQUIRED IMMUNODEFICIENCY SYNDROME (AIDS) RELATED NON-HODGKIN’S LYMPHOMAS
(Abstract release date: 05/19/16)
EHA Library. Clara J. 06/09/16; 132526; E977

Dr. Joseph Clara
Contributions
Contributions
Abstract
Abstract: E977
Type: Eposter Presentation
Background
Despite effective combination antiretroviral therapy for HIV, there is still increased incidence of Acquired Immunodeficiency Syndrome (AIDS) related Non-Hodgkin lymphomas (NHLs). AIDS related NHLs represent a challenge for the practicing oncologist. Prognostic factors have been shown to be useful to risk stratify the disease.
Aims
Here we examine potential prognostic indicators that may improve the performance of current prognostic systems in AIDS related NHLs.
Methods
Patients with HIV associated aggressive B-cell NHL were identified between 2001- 2014 at Moffitt Cancer Center. Patients with and primary central nervous system lymphoma were excluded. Clinical data including CD4 count, HIV viral load (VL) and opportunistic infections (OI) were included. Survival curves analyzed using the Kaplan Meier method and statistical significance was assessed using the log-rank test. A p < 0.05 was considered statistically significant.
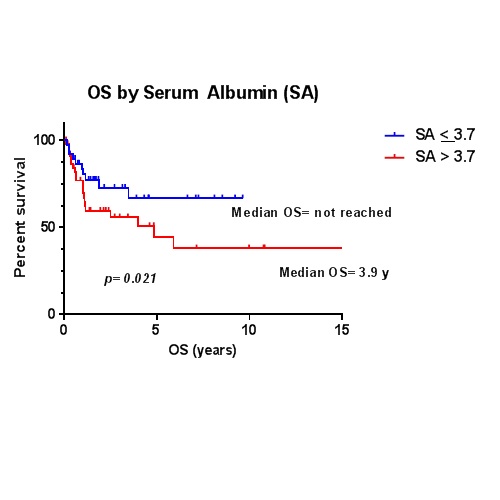
Results
A total of 85 patients were included. The male:female ratio was 6.7. Median age was 44.3 years (range 25 – 65). The median time from HIV to NHL diagnosis was 29 months (0 – 284). Seventy-eight percent presented with stage III/IV disease. The Eastern Cooperative Oncology Group performance (ECOG) status was > 1 in 62%. The most common histologies were Diffuse Large B Cell Lymphoma (DLBCL) and Burkitt’s lymphoma with 49 and 34%, respectively. Bulky disease was present in 27.3%, elevated LDH in 61.5%, and CD4 count < 100/mL at diagnosis in 29.5% patients. The mean Hb, SA and CD4 count were 3.6 g/dL, 11.8 g/dL and 205.9 k/uL, respectively. A serum albumin (SA) < 3.7 g/dL and Hb < 10 g/dl were present in 33% and 23.2% of patients, respectively. Forty-six percent had had cART at time of diagnosis. The cohort’s median OS was 5.9 years. KM curves showed poor median OS with SA < 3.7 g/dl (OS=3.9 y, p=0.021), Hb < 10 g/dl (0.7 y, p= 0.001) and OI (OS= 1.0 y, p=0.018), There was a trend with worse OS with NCCN-IPI score > 3 (OS=1.1 y, p= 0.165). MV analysis showed that SA < 3.7 retained statistical significance (HR: 2.45, CI: 1.03-5.84, p=0.042).
Conclusion
New prognostic scoring systems have improved the risk stratification of AIDS-related lymphomas (Barta el al, Haematologica 2014). SA < 3.7 is associated with worse OS in this study. SA could improve the stratification of AIDS related lymphomas in the cART era. A validation of the role of SA should be performed in larger cohorts.
Session topic: E-poster
Keyword(s): HIV related lymphoma, Non-Hodgkin's lymphoma, Prognostic factor
Type: Eposter Presentation
Background
Despite effective combination antiretroviral therapy for HIV, there is still increased incidence of Acquired Immunodeficiency Syndrome (AIDS) related Non-Hodgkin lymphomas (NHLs). AIDS related NHLs represent a challenge for the practicing oncologist. Prognostic factors have been shown to be useful to risk stratify the disease.
Aims
Here we examine potential prognostic indicators that may improve the performance of current prognostic systems in AIDS related NHLs.
Methods
Patients with HIV associated aggressive B-cell NHL were identified between 2001- 2014 at Moffitt Cancer Center. Patients with and primary central nervous system lymphoma were excluded. Clinical data including CD4 count, HIV viral load (VL) and opportunistic infections (OI) were included. Survival curves analyzed using the Kaplan Meier method and statistical significance was assessed using the log-rank test. A p < 0.05 was considered statistically significant.
Results
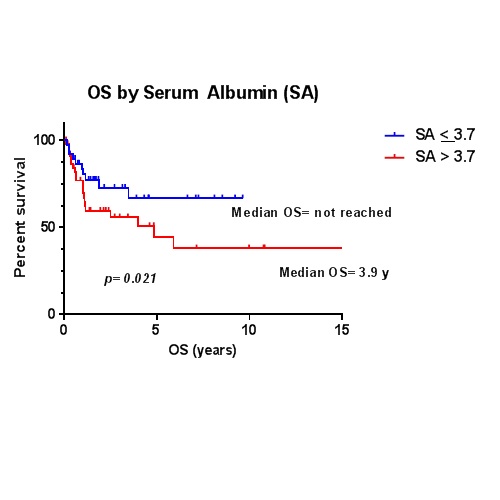
A total of 85 patients were included. The male:female ratio was 6.7. Median age was 44.3 years (range 25 – 65). The median time from HIV to NHL diagnosis was 29 months (0 – 284). Seventy-eight percent presented with stage III/IV disease. The Eastern Cooperative Oncology Group performance (ECOG) status was > 1 in 62%. The most common histologies were Diffuse Large B Cell Lymphoma (DLBCL) and Burkitt’s lymphoma with 49 and 34%, respectively. Bulky disease was present in 27.3%, elevated LDH in 61.5%, and CD4 count < 100/mL at diagnosis in 29.5% patients. The mean Hb, SA and CD4 count were 3.6 g/dL, 11.8 g/dL and 205.9 k/uL, respectively. A serum albumin (SA) < 3.7 g/dL and Hb < 10 g/dl were present in 33% and 23.2% of patients, respectively. Forty-six percent had had cART at time of diagnosis. The cohort’s median OS was 5.9 years. KM curves showed poor median OS with SA < 3.7 g/dl (OS=3.9 y, p=0.021), Hb < 10 g/dl (0.7 y, p= 0.001) and OI (OS= 1.0 y, p=0.018), There was a trend with worse OS with NCCN-IPI score > 3 (OS=1.1 y, p= 0.165). MV analysis showed that SA < 3.7 retained statistical significance (HR: 2.45, CI: 1.03-5.84, p=0.042).
Conclusion
New prognostic scoring systems have improved the risk stratification of AIDS-related lymphomas (Barta el al, Haematologica 2014). SA < 3.7 is associated with worse OS in this study. SA could improve the stratification of AIDS related lymphomas in the cART era. A validation of the role of SA should be performed in larger cohorts.
Session topic: E-poster
Keyword(s): HIV related lymphoma, Non-Hodgkin's lymphoma, Prognostic factor
Abstract: E977
Type: Eposter Presentation
Background
Despite effective combination antiretroviral therapy for HIV, there is still increased incidence of Acquired Immunodeficiency Syndrome (AIDS) related Non-Hodgkin lymphomas (NHLs). AIDS related NHLs represent a challenge for the practicing oncologist. Prognostic factors have been shown to be useful to risk stratify the disease.
Aims
Here we examine potential prognostic indicators that may improve the performance of current prognostic systems in AIDS related NHLs.
Methods
Patients with HIV associated aggressive B-cell NHL were identified between 2001- 2014 at Moffitt Cancer Center. Patients with and primary central nervous system lymphoma were excluded. Clinical data including CD4 count, HIV viral load (VL) and opportunistic infections (OI) were included. Survival curves analyzed using the Kaplan Meier method and statistical significance was assessed using the log-rank test. A p < 0.05 was considered statistically significant.
Results
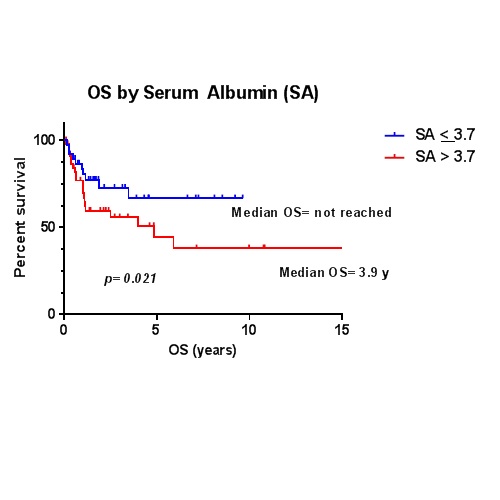
A total of 85 patients were included. The male:female ratio was 6.7. Median age was 44.3 years (range 25 – 65). The median time from HIV to NHL diagnosis was 29 months (0 – 284). Seventy-eight percent presented with stage III/IV disease. The Eastern Cooperative Oncology Group performance (ECOG) status was > 1 in 62%. The most common histologies were Diffuse Large B Cell Lymphoma (DLBCL) and Burkitt’s lymphoma with 49 and 34%, respectively. Bulky disease was present in 27.3%, elevated LDH in 61.5%, and CD4 count < 100/mL at diagnosis in 29.5% patients. The mean Hb, SA and CD4 count were 3.6 g/dL, 11.8 g/dL and 205.9 k/uL, respectively. A serum albumin (SA) < 3.7 g/dL and Hb < 10 g/dl were present in 33% and 23.2% of patients, respectively. Forty-six percent had had cART at time of diagnosis. The cohort’s median OS was 5.9 years. KM curves showed poor median OS with SA < 3.7 g/dl (OS=3.9 y, p=0.021), Hb < 10 g/dl (0.7 y, p= 0.001) and OI (OS= 1.0 y, p=0.018), There was a trend with worse OS with NCCN-IPI score > 3 (OS=1.1 y, p= 0.165). MV analysis showed that SA < 3.7 retained statistical significance (HR: 2.45, CI: 1.03-5.84, p=0.042).
Conclusion
New prognostic scoring systems have improved the risk stratification of AIDS-related lymphomas (Barta el al, Haematologica 2014). SA < 3.7 is associated with worse OS in this study. SA could improve the stratification of AIDS related lymphomas in the cART era. A validation of the role of SA should be performed in larger cohorts.
Session topic: E-poster
Keyword(s): HIV related lymphoma, Non-Hodgkin's lymphoma, Prognostic factor
Type: Eposter Presentation
Background
Despite effective combination antiretroviral therapy for HIV, there is still increased incidence of Acquired Immunodeficiency Syndrome (AIDS) related Non-Hodgkin lymphomas (NHLs). AIDS related NHLs represent a challenge for the practicing oncologist. Prognostic factors have been shown to be useful to risk stratify the disease.
Aims
Here we examine potential prognostic indicators that may improve the performance of current prognostic systems in AIDS related NHLs.
Methods
Patients with HIV associated aggressive B-cell NHL were identified between 2001- 2014 at Moffitt Cancer Center. Patients with and primary central nervous system lymphoma were excluded. Clinical data including CD4 count, HIV viral load (VL) and opportunistic infections (OI) were included. Survival curves analyzed using the Kaplan Meier method and statistical significance was assessed using the log-rank test. A p < 0.05 was considered statistically significant.
Results
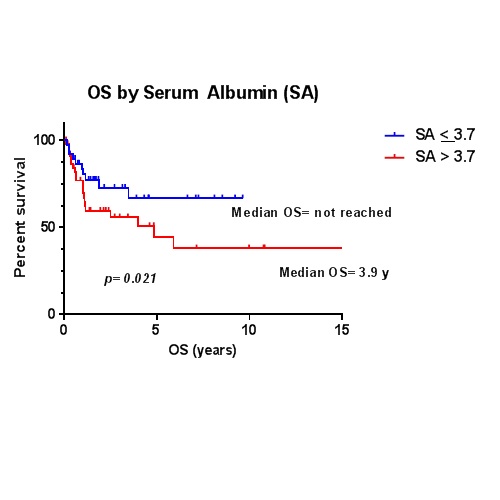
A total of 85 patients were included. The male:female ratio was 6.7. Median age was 44.3 years (range 25 – 65). The median time from HIV to NHL diagnosis was 29 months (0 – 284). Seventy-eight percent presented with stage III/IV disease. The Eastern Cooperative Oncology Group performance (ECOG) status was > 1 in 62%. The most common histologies were Diffuse Large B Cell Lymphoma (DLBCL) and Burkitt’s lymphoma with 49 and 34%, respectively. Bulky disease was present in 27.3%, elevated LDH in 61.5%, and CD4 count < 100/mL at diagnosis in 29.5% patients. The mean Hb, SA and CD4 count were 3.6 g/dL, 11.8 g/dL and 205.9 k/uL, respectively. A serum albumin (SA) < 3.7 g/dL and Hb < 10 g/dl were present in 33% and 23.2% of patients, respectively. Forty-six percent had had cART at time of diagnosis. The cohort’s median OS was 5.9 years. KM curves showed poor median OS with SA < 3.7 g/dl (OS=3.9 y, p=0.021), Hb < 10 g/dl (0.7 y, p= 0.001) and OI (OS= 1.0 y, p=0.018), There was a trend with worse OS with NCCN-IPI score > 3 (OS=1.1 y, p= 0.165). MV analysis showed that SA < 3.7 retained statistical significance (HR: 2.45, CI: 1.03-5.84, p=0.042).
Conclusion
New prognostic scoring systems have improved the risk stratification of AIDS-related lymphomas (Barta el al, Haematologica 2014). SA < 3.7 is associated with worse OS in this study. SA could improve the stratification of AIDS related lymphomas in the cART era. A validation of the role of SA should be performed in larger cohorts.
Session topic: E-poster
Keyword(s): HIV related lymphoma, Non-Hodgkin's lymphoma, Prognostic factor
{{ help_message }}
{{filter}}


