EVALUATION OF THE NEW PROGNOSTIC SCORE IN HIV RELATED NON HODGKIN LYMPHOMA. EXPERIENCE IN UNIVERSITY HOSPITAL SON ESPASES.
(Abstract release date: 05/19/16)
EHA Library. Ruiz De Gracia S. 06/09/16; 132509; E960

Mrs. Silvia Ruiz De Gracia
Contributions
Contributions
Abstract
Abstract: E960
Type: Eposter Presentation
Background
The use of the International Prognostic Index (IPI) in aggressive lymphoma is widespread in the context of HIV infection. However recently it has been reported a new index tailored to patients infected with human immunodeficiency virus (HIV) which takes into account the characteristics of immunosuppression, viral load and evolutionary status of HIV infection: the AIDS-related lymphoma International Prognostic Index (ARL- IPI).
Aims
To evaluate this new index inside the Balearic Lymphoma Group in comparison with other prognostic scores used in aggressive lymphomas.
Methods
We identified all aggressive lymphomas diagnosed between 2002 and 2015 based on the records of the Service of Pathology contrasted with their HIV status. After that, the characteristics of their HIV infection (CD4 counts, viral load and AIDS-defining illness) with the main prognostic factors, treatment and evolution of the lymphoma were subsequently collected. Survival analysis was performed using Kaplan - Meier curves with the log -rank test.
Results
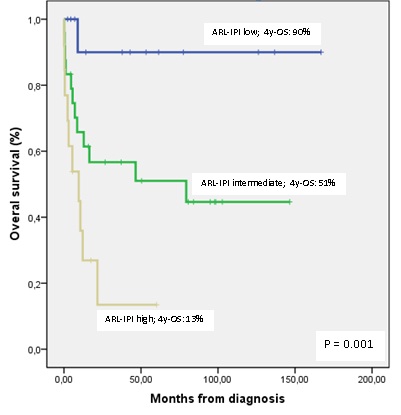
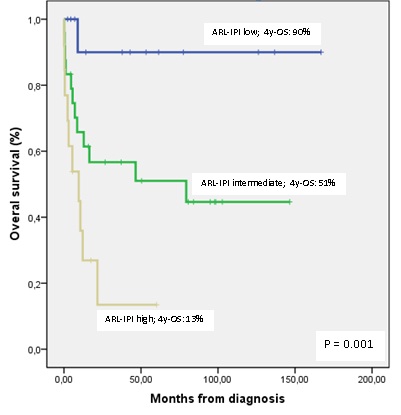
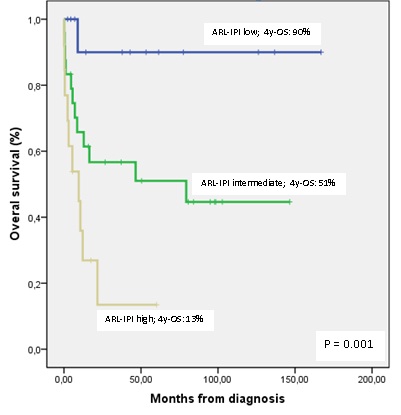
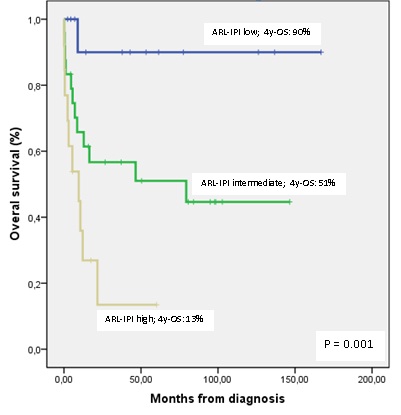
Table 1 shows main characteristics of the patients (n=50). Median age was 41 years, most with advanced disease (84% Ann Arbor (AA) stage III-IV) and poor prognosis factors: 70% a-IPI >1 and 71% TS>2. Seventy-two percent of cases had a prior history of AIDS; while 46% had CD4 counts lower than 200 / microL and 54% VIH viral loads higher than 10000 copies/mL. ARL-IPI showed 26%, 42% and 26% of patients respectively in the low, intermediate and high risk subgroups. Overall response (p=0.002) and CR rates (p=0.012) were significantly different in these three risk subgroups: respectively low risk (92% and 77%), intermediate risk (74% and 65%) and high risk (31% and 23%). Median follow-up was 53 (0-167) months. PFS and OS at 4 years was 53% and 51%, respectively. Univaried survival analysis showed several factors significantly associated to worse PFS (ECOG PS>1, p=0.001; III-IV AA stage, p=0.018; a-IPI 2-3, p=0.01; R-IPI 1-2 or 3-5, p=0.029; TS>2, p=0.006; intermediate and high ARL, p=0.002 and lower CD4 count, p=0.019) and OS (ECOG PS>1, p<0.001; bulky disease, p=0.043; a-IPI 2-3, p=0.041; intermediate and high ARL-IPI, p=0.001 and lower CD4 count, p=0.001) (Image 1). Table 1:
Conclusion
In our study ARL-IPI showed a very good definition of prognostic groups in terms of response and survival. Interestingly, ARL-IPI identifies a high risk subgroup with a very poor prognosis. Our results validate the usefulness of this new prognostic index in the HIV population with aggressive lymphoma.
Session topic: E-poster
Keyword(s): HIV related lymphoma, Non-Hodgkin's lymphoma, Prognosis
Type: Eposter Presentation
Background
The use of the International Prognostic Index (IPI) in aggressive lymphoma is widespread in the context of HIV infection. However recently it has been reported a new index tailored to patients infected with human immunodeficiency virus (HIV) which takes into account the characteristics of immunosuppression, viral load and evolutionary status of HIV infection: the AIDS-related lymphoma International Prognostic Index (ARL- IPI).
Aims
To evaluate this new index inside the Balearic Lymphoma Group in comparison with other prognostic scores used in aggressive lymphomas.
Methods
We identified all aggressive lymphomas diagnosed between 2002 and 2015 based on the records of the Service of Pathology contrasted with their HIV status. After that, the characteristics of their HIV infection (CD4 counts, viral load and AIDS-defining illness) with the main prognostic factors, treatment and evolution of the lymphoma were subsequently collected. Survival analysis was performed using Kaplan - Meier curves with the log -rank test.
Results
Table 1 shows main characteristics of the patients (n=50). Median age was 41 years, most with advanced disease (84% Ann Arbor (AA) stage III-IV) and poor prognosis factors: 70% a-IPI >1 and 71% TS>2. Seventy-two percent of cases had a prior history of AIDS; while 46% had CD4 counts lower than 200 / microL and 54% VIH viral loads higher than 10000 copies/mL. ARL-IPI showed 26%, 42% and 26% of patients respectively in the low, intermediate and high risk subgroups. Overall response (p=0.002) and CR rates (p=0.012) were significantly different in these three risk subgroups: respectively low risk (92% and 77%), intermediate risk (74% and 65%) and high risk (31% and 23%). Median follow-up was 53 (0-167) months. PFS and OS at 4 years was 53% and 51%, respectively. Univaried survival analysis showed several factors significantly associated to worse PFS (ECOG PS>1, p=0.001; III-IV AA stage, p=0.018; a-IPI 2-3, p=0.01; R-IPI 1-2 or 3-5, p=0.029; TS>2, p=0.006; intermediate and high ARL, p=0.002 and lower CD4 count, p=0.019) and OS (ECOG PS>1, p<0.001; bulky disease, p=0.043; a-IPI 2-3, p=0.041; intermediate and high ARL-IPI, p=0.001 and lower CD4 count, p=0.001) (Image 1). Table 1:
| Sex (M/F) | 45 (90%) / 5 (10%) |
| ECOG PS > 1 | 16 (32%) |
| B symptoms | 29 (58%) |
| High LDH | 32 (64%) |
| High Beta-2-microglobuline | 40 (91%) |
| > 1 extranodal site | 12 (24%) |
| Bulky disease | 5 (10%) |
| Diagnosis:- DLBCL- Plasmablastic lymphoma- Burkitt lymphoma- Peripheral T-cell lymphoma | 31 (62%)10 (20%)7 (14%)2 (4%) |
| a-IPI:- 0-1- 2-3 | 15 (30%)35 (70%) |
| R-IPI:- Low risk (0)- Intemediate risk (1-2)- High risk (3-5) | 4 (8%)32 (64%)14 (28%) |
| LRS-IPI:- Low risk- Intermediate risk- High risk | 13 (26%)24 (48%)13 (26%) |
| CD4 count:- <50- 50-199- 200-499- >500 | 5 (10%)18 (36%)12 (24%)15 (30%) |
Conclusion
In our study ARL-IPI showed a very good definition of prognostic groups in terms of response and survival. Interestingly, ARL-IPI identifies a high risk subgroup with a very poor prognosis. Our results validate the usefulness of this new prognostic index in the HIV population with aggressive lymphoma.
Session topic: E-poster
Keyword(s): HIV related lymphoma, Non-Hodgkin's lymphoma, Prognosis
Abstract: E960
Type: Eposter Presentation
Background
The use of the International Prognostic Index (IPI) in aggressive lymphoma is widespread in the context of HIV infection. However recently it has been reported a new index tailored to patients infected with human immunodeficiency virus (HIV) which takes into account the characteristics of immunosuppression, viral load and evolutionary status of HIV infection: the AIDS-related lymphoma International Prognostic Index (ARL- IPI).
Aims
To evaluate this new index inside the Balearic Lymphoma Group in comparison with other prognostic scores used in aggressive lymphomas.
Methods
We identified all aggressive lymphomas diagnosed between 2002 and 2015 based on the records of the Service of Pathology contrasted with their HIV status. After that, the characteristics of their HIV infection (CD4 counts, viral load and AIDS-defining illness) with the main prognostic factors, treatment and evolution of the lymphoma were subsequently collected. Survival analysis was performed using Kaplan - Meier curves with the log -rank test.
Results
Table 1 shows main characteristics of the patients (n=50). Median age was 41 years, most with advanced disease (84% Ann Arbor (AA) stage III-IV) and poor prognosis factors: 70% a-IPI >1 and 71% TS>2. Seventy-two percent of cases had a prior history of AIDS; while 46% had CD4 counts lower than 200 / microL and 54% VIH viral loads higher than 10000 copies/mL. ARL-IPI showed 26%, 42% and 26% of patients respectively in the low, intermediate and high risk subgroups. Overall response (p=0.002) and CR rates (p=0.012) were significantly different in these three risk subgroups: respectively low risk (92% and 77%), intermediate risk (74% and 65%) and high risk (31% and 23%). Median follow-up was 53 (0-167) months. PFS and OS at 4 years was 53% and 51%, respectively. Univaried survival analysis showed several factors significantly associated to worse PFS (ECOG PS>1, p=0.001; III-IV AA stage, p=0.018; a-IPI 2-3, p=0.01; R-IPI 1-2 or 3-5, p=0.029; TS>2, p=0.006; intermediate and high ARL, p=0.002 and lower CD4 count, p=0.019) and OS (ECOG PS>1, p<0.001; bulky disease, p=0.043; a-IPI 2-3, p=0.041; intermediate and high ARL-IPI, p=0.001 and lower CD4 count, p=0.001) (Image 1). Table 1:
Conclusion
In our study ARL-IPI showed a very good definition of prognostic groups in terms of response and survival. Interestingly, ARL-IPI identifies a high risk subgroup with a very poor prognosis. Our results validate the usefulness of this new prognostic index in the HIV population with aggressive lymphoma.
Session topic: E-poster
Keyword(s): HIV related lymphoma, Non-Hodgkin's lymphoma, Prognosis
Type: Eposter Presentation
Background
The use of the International Prognostic Index (IPI) in aggressive lymphoma is widespread in the context of HIV infection. However recently it has been reported a new index tailored to patients infected with human immunodeficiency virus (HIV) which takes into account the characteristics of immunosuppression, viral load and evolutionary status of HIV infection: the AIDS-related lymphoma International Prognostic Index (ARL- IPI).
Aims
To evaluate this new index inside the Balearic Lymphoma Group in comparison with other prognostic scores used in aggressive lymphomas.
Methods
We identified all aggressive lymphomas diagnosed between 2002 and 2015 based on the records of the Service of Pathology contrasted with their HIV status. After that, the characteristics of their HIV infection (CD4 counts, viral load and AIDS-defining illness) with the main prognostic factors, treatment and evolution of the lymphoma were subsequently collected. Survival analysis was performed using Kaplan - Meier curves with the log -rank test.
Results
Table 1 shows main characteristics of the patients (n=50). Median age was 41 years, most with advanced disease (84% Ann Arbor (AA) stage III-IV) and poor prognosis factors: 70% a-IPI >1 and 71% TS>2. Seventy-two percent of cases had a prior history of AIDS; while 46% had CD4 counts lower than 200 / microL and 54% VIH viral loads higher than 10000 copies/mL. ARL-IPI showed 26%, 42% and 26% of patients respectively in the low, intermediate and high risk subgroups. Overall response (p=0.002) and CR rates (p=0.012) were significantly different in these three risk subgroups: respectively low risk (92% and 77%), intermediate risk (74% and 65%) and high risk (31% and 23%). Median follow-up was 53 (0-167) months. PFS and OS at 4 years was 53% and 51%, respectively. Univaried survival analysis showed several factors significantly associated to worse PFS (ECOG PS>1, p=0.001; III-IV AA stage, p=0.018; a-IPI 2-3, p=0.01; R-IPI 1-2 or 3-5, p=0.029; TS>2, p=0.006; intermediate and high ARL, p=0.002 and lower CD4 count, p=0.019) and OS (ECOG PS>1, p<0.001; bulky disease, p=0.043; a-IPI 2-3, p=0.041; intermediate and high ARL-IPI, p=0.001 and lower CD4 count, p=0.001) (Image 1). Table 1:
| Sex (M/F) | 45 (90%) / 5 (10%) |
| ECOG PS > 1 | 16 (32%) |
| B symptoms | 29 (58%) |
| High LDH | 32 (64%) |
| High Beta-2-microglobuline | 40 (91%) |
| > 1 extranodal site | 12 (24%) |
| Bulky disease | 5 (10%) |
| Diagnosis:- DLBCL- Plasmablastic lymphoma- Burkitt lymphoma- Peripheral T-cell lymphoma | 31 (62%)10 (20%)7 (14%)2 (4%) |
| a-IPI:- 0-1- 2-3 | 15 (30%)35 (70%) |
| R-IPI:- Low risk (0)- Intemediate risk (1-2)- High risk (3-5) | 4 (8%)32 (64%)14 (28%) |
| LRS-IPI:- Low risk- Intermediate risk- High risk | 13 (26%)24 (48%)13 (26%) |
| CD4 count:- <50- 50-199- 200-499- >500 | 5 (10%)18 (36%)12 (24%)15 (30%) |
Conclusion
In our study ARL-IPI showed a very good definition of prognostic groups in terms of response and survival. Interestingly, ARL-IPI identifies a high risk subgroup with a very poor prognosis. Our results validate the usefulness of this new prognostic index in the HIV population with aggressive lymphoma.
Session topic: E-poster
Keyword(s): HIV related lymphoma, Non-Hodgkin's lymphoma, Prognosis
{{ help_message }}
{{filter}}


